-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(8): 572-575
doi:10.5923/j.ajmms.20201008.07

Phenotypic Features of Red Blood Cell Antigens in Uzbekistan
Gulnoza Xabibjon Qizi Kayumova1, A’lonur Bakhtinurovich Saidov2
1Department of Extracorporeal Blood Purification, Republican Specialized Scientific and Practical Medical Center of Hematology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
2Administration, Republican Blood Transfusion Center, Tashkent, Uzbekistan
Correspondence to: Gulnoza Xabibjon Qizi Kayumova, Department of Extracorporeal Blood Purification, Republican Specialized Scientific and Practical Medical Center of Hematology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

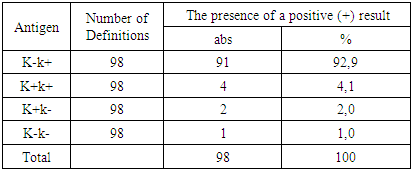
The aim of the study was to study the antigenic properties of red blood cells in healthy donors of blood components. 100 conditionally healthy donors examined at the Republican Center for Blood Transfusion took part in this study. Rhesus, Kell, and Kidd System red blood cell antigens were determined using monoclonal antibodies. The results indicate that in healthy donors, all 4 phenotypes of the Kell system antigens - K-k +, K-k-, K + k + and K + k- - are found. The most common phenotype was the phenotype - K-k + (92.9%). Kell phenotypes of healthy donors are arranged in the following sequence: K-k + >> K + k +> K + k-> K-k-. Our studies made it possible not only to understand the prevalence of major antigens of the AB0 system and Rhesus in all regions of the Republic of Uzbekistan, but also to consider the prevalence of phenotypes of antigens of the AB0 system, Rhesus and Kell in healthy donors.
Keywords: Erythrocyte antigenic properties, Conditionally healthy donors, Monoclonal antibodies, Kell system antigen phenotypes, K-k + phenotype
Cite this paper: Gulnoza Xabibjon Qizi Kayumova, A’lonur Bakhtinurovich Saidov, Phenotypic Features of Red Blood Cell Antigens in Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 572-575. doi: 10.5923/j.ajmms.20201008.07.
Article Outline
1. Introduction
- Transfusion of erythrocyte-containing components can cause problems due to the presence in the blood of recipients and donors of alloimmune anti-erythrocyte antibodies. Blood group antigens are located on the outer surface of the erythrocyte membrane and are genetic traits inherited from parents and not changing throughout life or can only change in pathological conditions [5].The alloimmunization index of a healthy population, calculated on the basis of the results of an immunohematological examination of blood component donors, is a basic criterion for determining the risk of post-transfusion complications (PTC) and post-transfusion reactions (PTR), the effectiveness of the prevention of alloimmunization due to pregnancy and transfusion of blood components. It is known that the values of this criterion vary in countries and regions and are associated primarily with the national composition of the population and the nature of the distribution of blood cell antigens [6,12,14].In addition, this indicator depends on the methods used to study antibodies. This index rises when using more sensitive laboratory tests. Antibodies are immunoglobulins produced by cells of the immune system in response to antigenic stimulation. Depending on the genesis, they distinguish: 1) autoantibodies interacting with their own blood cells; 2) alloantibodies directed to the blood cells of another individual within the species; 3) heteroantibodies, agglutinating red blood cells of animals of another species.Antibodies that react with a specific antigen are classified as specific, and antibodies that interact with several antigens or with antigens that are widely distributed in the population and are not identifiable are antibodies with undetermined specificity [9].If the patient’s antibodies react with all test erythrocytes and erythrocytes of all donors, then the presence of “panagglutinating” antibodies in the patient is noted.To date, about 270 red blood cell antigens are known that form 26 blood group antigens [1,2,8,13,15].Most important are the most immunogenic (immunogenicity - the ability to cause complications after transfusion of blood components) antigens, primarily the systems AB0, Rh (Rhesus), Kell, etc. [4,6,7,10].The phenotype of human erythrocyte antigens includes a set of antigens of different systems of blood groups located on the surface of red blood cells. This set is individual for each person. Therefore, when transfusing blood and red blood cells, it is necessary to take into account the compatibility not only of the erythrocyte antigens of the AB0 and Rhesus systems, but also of the antigens of other systems [11,15].It is known that in addition to the most highly immunogenic D antigen, there are also a number of Rhesus antigens, denoted by the letters C, c, E, e, Cw, which have certain clinical meanings. These antigens are synthesized by the RHD and RHCE genes located on the 1st chromosome. Both genes are closely related. Cw antigen is a product of the mutated RHCE gene, and therefore it is a modification of C antigen [3,13].A literature search for blood antigens in the Republic showed that no such studies were conducted. Of particular importance is the role of minor antigens in hematological patients, as well as in pregnant women. It is known that minor antigens cause blood transfusion complications of varying severity. Analysis of transfusion sheets of patients showed that they received blood components from 2 to 10-20 per year. These data show that in hematological patients in the blood there are antigens of at least 10-20 different donors. All of the above data and many different allogeneic sensitizations motivated us to conduct this study [4].
2. Main Body
2.1. Purpose of the Study
- Study of the antigenic properties of red blood cells in healthy donors of blood components.
2.2. Material and Methods of Investigation
- This study was attended by 100 conditionally healthy donors examined at the Republican Center for Blood Transfusion. The following research methods were used: the isoserological method using monoclonal reagents of various specificity, the determination of antibodies against red blood cells using antiglobulin serum, and the method of conglutination using a 33% polyglucin solution.During blood transfusions, erythrocyte erythrocyte antigens from Rhesus, Kell, and Kidd Systems were determined using monoclonal antibodies that are produced by in vitro hybridoma cell lines [9,10]. Statistical data processing was performed using Microsoft Excel 2007 software.
2.3. Results and Discussion
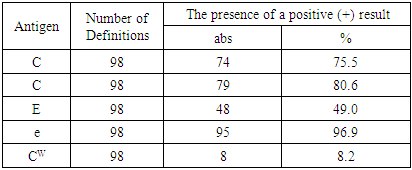
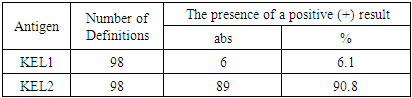
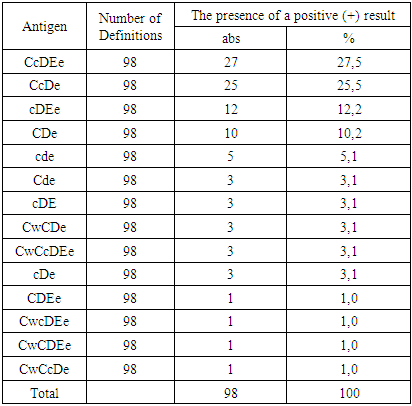
- We studied the distribution of antigens of the RH system - C, c, E, e, and Cw, the Kell system, as well as the phenotype of the RHCE and Kell system among the population of Uzbekistan. The results showed that antigens C and C are found with approximately the same frequency - 75.5 and 80.6% (table 1).
|
|
|
|
3. Conclusions
- Thus, our studies made it possible to understand the prevalence of major antigens of the AB0 system and rhesus in all regions of the Republic of Uzbekistan, as well as to consider the prevalence of phenotypes of antigens of the AB0 system, Rhesus and Kell in healthy donors. Judging by the immunogenicity of antigens, about 2% of donors have the K + antigen that can cause sensitization and an immune complication. A study of the distribution of blood groups in the population will create the prerequisites for creating a bank for the long-term storage of phenotyped donated blood, which will significantly increase the immunological safety of blood and its components for recipients in the conditions of planned work and in emergency situations.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML