-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(8): 557-562
doi:10.5923/j.ajmms.20201008.04

Clinical and Laboratory Characteristics of Patients with Hepatocellular Carcinoma Associated with Viral Hepatitis B
Krestina Stepanovna Brigida 1, Erkin Isakovich Musabaev 1, Dilshod Mahmudovich Egamberdiev 2, Aziza Saydullaevna Khikmatullaeva 1
1Scientific Research Institute of Virology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
2Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology, Tashkent, Uzbekistan
Correspondence to: Krestina Stepanovna Brigida , Scientific Research Institute of Virology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The presence of cirrhosis increases the risk of developing hepatocellular carcinoma by more than 30 times compared with patients without cirrhosis. Such a high risk of developing primary liver cancer is due to the fact that cirrhosis is the final stage in the progression of a large number of lesions and liver diseases. It should be borne in mind that in most patients, cirrhosis of the liver is compensated in nature and, accordingly, is asymptomatic. In such cases, the onset of symptoms and, accordingly, the diagnosis of the disease occurs either at the onset of the decompensation phase of liver cirrhosis, or when signs of neoplasm appear. The work included data from a retrospective and prospective analysis of case histories of patients diagnosed with hepatocellular carcinoma who were hospitalized at the Republican Specialized Scientific and Practical Medical Center for Oncology and Radiology of the Republic of Uzbekistan from 2016 to 2019. 68 Patients were divided into 2 groups. The main group consisted of patients with hepatocellular carcinoma and positive tests for HBsAg. The control group included patients with hepatocellular carcinoma, in which serological markers for viral hepatitis were negative. This is due to the direct participation of the hepatitis B virus itself in the development of oncogenesis of hepatocellular carcinoma. In addition, the clinical picture consists of the symptoms of the oncological process on the one hand and the clinical picture of a prolonged viral liver damage, on the other hand.
Keywords: Hepatocellular carcinoma, Viral hepatitis B, Cirrhosis
Cite this paper: Krestina Stepanovna Brigida , Erkin Isakovich Musabaev , Dilshod Mahmudovich Egamberdiev , Aziza Saydullaevna Khikmatullaeva , Clinical and Laboratory Characteristics of Patients with Hepatocellular Carcinoma Associated with Viral Hepatitis B, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 557-562. doi: 10.5923/j.ajmms.20201008.04.
Article Outline
1. Introduction
- According to the International Organization for Research on Cancer, liver cancer is in 5th place among the most common malignant neoplasms in men (523,000 cases per year; 7.9%) and 17th place in women (226,000 cases per year; 6.5%) in the world [1]. Unlike other more common neoplasms, which tend to decrease in incidence, the incidence of liver cancer increases [2]. Hepatocellular carcinoma is the sixth most common type of cancer in the world, accounting for 7% of all cancers. The incidence of hepatocellular carcinoma is about 749,000 new cases each year. The highest incidence rates of hepatocellular carcinoma (about 85% of cases) are observed in East Asia and Africa [3]. Hepatocellular carcinoma is the fourth leading cause of death among oncological diseases in the world. About 33% of all deaths from hepatocellular carcinoma are associated with chronic viral hepatitis B infection, while 30% are associated with alcohol abuse, 21% with chronic viral hepatitis C infection, and 16% with the rest of the etiology [4]. With chronic carriage of viral hepatitis B, the risk of hepatocellular carcinoma increases by 5–15 times compared with patients not suffering from chronic viral hepatitis [5].The introduction of vaccination programs at birth significantly reduced the frequency and prevalence of viral hepatitis B in several areas with high endemicity, which had a serious impact on the incidence of the liver, especially hepatocellular carcinoma [6,7]. Despite the fact that the prevalence of viral hepatitis B infection in the world is decreasing, the absolute number of infected people continues to grow as a result of global population growth [8]. Since chronic viral hepatitis B, as a rule, is asymptomatic until progressive liver disease develops, up to approximately 80% of infected patients are not aware of their infection and concomitant liver disease [9].Hepatocellular carcinoma associated with viral hepatitis B is mainly observed among men (203,000 new cases in 2015 versus 70,000 in women), while the ratio of men to women is about 3: 1, and also causes one third of deaths from hepatocellular carcinoma [10]. An additional factor associated with an increased risk of hepatocellular carcinoma is the duration of the disease [11]. Chronic inflammatory condition and hepatic oxidative stress caused by chronic hepatitis B accelerate cell aging processes. Aging processes are at the genomic level and are associated with the shortening of telomeres, the length of which is inversely proportional to the degree of fibrosis and reaches the lowest values for hepatocellular carcinoma [12].The presence of cirrhosis increases the risk of developing hepatocellular carcinoma by more than 30 times compared with patients without cirrhosis [13]. Such a high risk of developing primary liver cancer is due to the fact that cirrhosis is the final stage in the progression of a large number of lesions and liver diseases. It should be borne in mind that in most patients, cirrhosis of the liver is compensated in nature and, accordingly, is asymptomatic. In such cases, the onset of symptoms and, accordingly, the diagnosis of the disease occurs either at the onset of the decompensation phase of liver cirrhosis, or when signs of neoplasm appear.
2. Materials and Methods
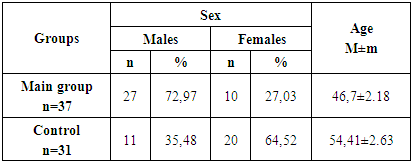
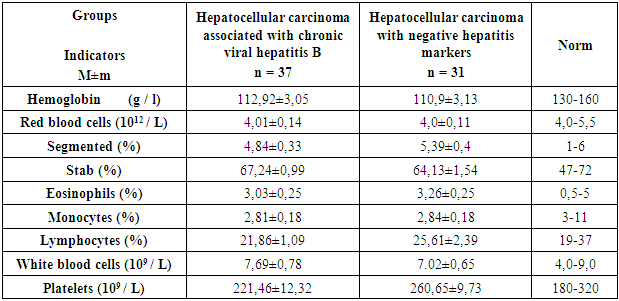
- The work included data from a retrospective and prospective analysis of case histories of patients diagnosed with hepatocellular carcinoma who were hospitalized at the Republican Specialized Scientific and Practical Medical Center for Oncology and Radiology of the Republic of Uzbekistan from 2016 to 2019.Patients were divided into 2 groups. The main group consisted of patients with hepatocellular carcinoma and positive tests for HBsAg. The control group included patients with hepatocellular carcinoma, in which serological markers for viral hepatitis were negative.The criteria for inclusion in the main group were the presence of hepatocellular carcinoma, confirmed by ultrasound and computed tomography and / or magnetic resonance imaging and histological confirmation of the diagnosis, as well as the presence of HBsAg. Exclusion criteria were negative markers for HBsAg, the presence of concomitant hepatitis C, human immunodeficiency virus (HIV), under 18 years of age and all other causes of cirrhosis eg. alcoholic, primary biliary cirrhosis.The criteria for inclusion in the control group were the presence of hepatocellular carcinoma confirmed by ultrasound and computed tomography and / or magnetic resonance imaging and histological confirmation of the diagnosis of negative markers for viral hepatitis and human immunodeficiency virus (HIV), under the age of 18 years.The average age of patients in group 1 was 46.7 ± 2.18 years. Men were 27 (72.97%), women were 10 (27.03%). The average age of patients in the second group was 54.41 ± 2.63 years. There were 11 men (35.48%), 20 women (64.52%).The examination of the patients consisted of an assessment of complaints, physical examination, data from general laboratory tests (general and biochemical blood tests), instrumental methods of investigation (ultrasound, computed tomography and / or magnetic resonance imaging), histological data.Statistical analysis was performed using Excel 16.0 programs. For each series of results, the arithmetic mean (M), the error of the mean (m), were calculated. In the tables, the results are presented as M ± m. Comparison of two samples was carried out using the xi-square. When comparing the average values, the Student t-test was used. For the level of reliability of statistical indicators, p <0.05 was taken.
3. Results
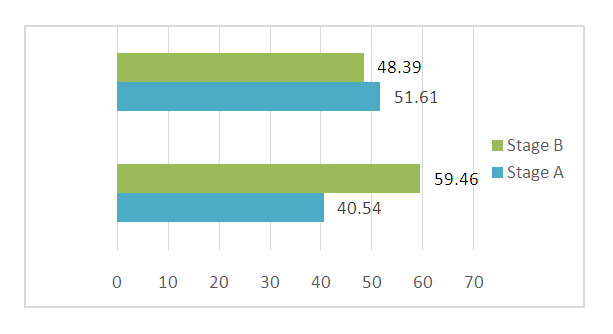
- In the analysis, hepatocellular carcinoma was more common in men - 59 people (62.77%) than in women-35 (37.23%) people. The number of men predominated in the group with hepatocellular carcinoma associated with viral hepatitis B, while in the group of patients with hepatocellular carcinoma without viral hepatitis, the numerical advantage was in women. (table 1).
|
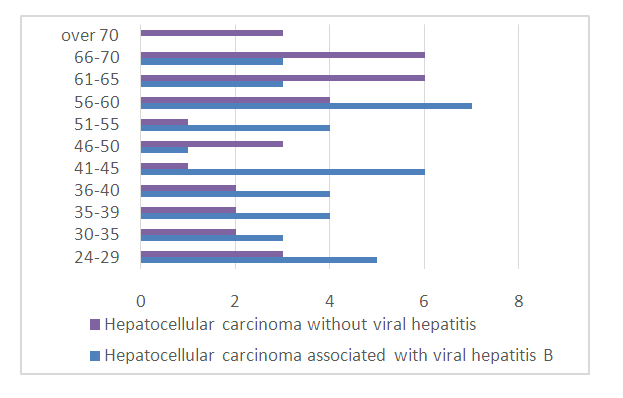 | Figure 1. Age distribution in the study groups |
|
|
|
 | Figure 2. Distribution of patients with hepatocellular carcinoma according to the Barcelona Clinical Classification of Cancer |
4. Discussion
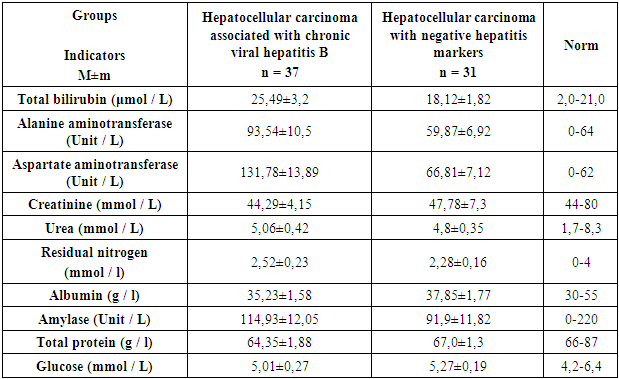
- The results of our studies show that hepatocellular carcinoma associated with chronic hepatitis B was statistically more common at a younger age compared with hepatocellular carcinoma without viral hepatitis, which developed mainly after 50 years. Apparently this is due to early infection, leading to malignant transformation of hepatocytes. In our studies, the majority of patients in the group with hepatocellular carcinoma associated with chronic hepatitis B are men, which is consistent with world literature. Patients with hepatocellular carcinoma associated with chronic hepatitis B were statistically more likely to complain of pain in the right hypochondrium and weight loss compared with the control group. Despite the fact that patients in the main group more often complained of weakness, malaise, decreased appetite and nausea, nevertheless, there were no statistically significant differences in the studied groups. On examination, the ictericity of the sclera and skin, splenomegaly and ascites were statistically more common in the group with hepatocellular carcinoma associated with chronic hepatitis B, which is associated as a direct effect of the hepatitis B virus on hepatocytes. In a general blood test in patients with hepatocellular carcinoma associated with chronic hepatitis B, thrombocytopenia was statistically more common, which is associated with the phenomena of hypersplenism characteristic of liver cirrhosis. A detailed examination of the blood chemistry data of patients with hepatocellular carcinoma associated with chronic hepatitis B showed a significantly higher level of total and direct bilirubin, Alanine aminotransferase and Aspartate aminotransferase. Thus, cytolytic syndrome caused by viral liver damage and the immuno-mediated action of viral hepatitis B came to the fore. Patients with hepatocellular carcinoma associated with chronic hepatitis B were more likely to experience cirrhosis, which is also associated with prolonged persistence of viral hepatitis B. In addition, in 24.32% of patients in the main group hepatocellular carcinoma developed without cirrhosis, which is explained by the direct influence of the presence of hepatitis B viruses themselves on the oncogenesis of hepatocellular carcinoma. Tumor nodes in patients with hepatocellular carcinoma associated with chronic hepatitis B were statistically more often located in the right lobe of the liver compared to the control group. Metastases to neighboring organs were also statistically more often observed in patients with hepatocellular carcinoma associated with chronic hepatitis B.
5. Conclusions
- Despite the similar picture, the clinical picture of hepatocellular carcinoma associated with viral hepatitis B has a number of features compared to hepatocellular carcinoma without viral hepatitis. This is due to the direct participation of the hepatitis B virus itself in the development of oncogenesis of hepatocellular carcinoma. In addition, the clinical picture consists of the symptoms of the oncological process on the one hand and the clinical picture of a prolonged viral liver damage, on the other hand.
ACKNOWLEDGEMENTS
- We are grateful to the staff members of Scientific Research Institute of Virology and Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology for the cooperation and support in our research. The participants kindly gave full written permission for this report.
Ethical Approval
- The ethical approval for the study was granted by the Committee of Ethical Approval for Researches under the Ministry of Health of the Republic of Uzbekistan.
Consent
- Written informed consent was obtained from all participants of the research for publication of this paper and any accompanying information related to this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML