E. Yu. Valiev1, O. E. Valiev2, A. M. Azizov2
1Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
2Republican Specialized Scientific and Practical Center of Traumatology and Orthopedics, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Injury of the bone structures in the hip joint refers to severe trauma of the musculoskeletal system for the elderly and senile patients leading to an adverse outcome. One of the important problems of geriatric practice is comorbidity which affects the prognosis for life, increases the likelihood of lethal outcome. The frequency analysis of presence and level of comorbidity in 201 patients with fractures of the femoral neck has been conducted. The mean age was 71.4 ± 7.1 years. When evaluating the comorbidity indices, its high indicators were found: the Charlson index averaged 9.12 ± 1.05 points, the Cumulative Illness Rating Scale (CIRS) index madeup 16.2 ± 3.9 points. The main contingent of treated 147 (73.1%) patients were individuals with a high level of physical activity. The analysis showed a direct dependence of the tactics choice and treatment methods on age, somatic status, degree of comorbidity index, level of physical activity, level of operational risk according to ASA, as well as dependence on the type of fractures according to Garden classification. Depending on the treatment tactics, the patients were divided into three groups: conservative treatment - 54 (26.9%); operative treatment (osteosynthesis) - 81 (40.3%) and total hip replacement - 66 (32.8%).The most promising method of treating patients with fractures of the femoral neck in the elderly and senile is hip arthroplastyat the current stage of traumatology development. It should be performed with adequate technical equipment, after preliminary preparation of patients and at the earliest possible time, before the development of complications.
Keywords:
Femoral neck fracture, Older age group, Comorbid pathology, Osteosynthesis, Hip arthroplasty
Cite this paper: E. Yu. Valiev, O. E. Valiev, A. M. Azizov, The Effect of Comorbid Pathology on the Treatment Tactics of Femoral Neck Fractures in Elderly and Senile Patients, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 552-556. doi: 10.5923/j.ajmms.20201008.03.
1. Introduction
Injury of bone structures in the hip joint refers to severe injuries of the musculoskeletal system, the features of which are prolonged disability, a high percentage of disability, prolonged bedriddenness for the elderly and senile with the development of complications leading to an unfavorable outcome. According to various researchers’ data, from 15 to 45% of injuries in the structure of the musculoskeletal system are fractures of the femur, fractures of the femoral neck make up 50 to 55% among them [1]. Such a large proportion of the femoral neck fractures are due to an increase in the number of elderly people. One of the important problems of geriatric practice is polymorbidity (comorbidity) - the presence of several diseases in one patient. Age is a strong risk factor for numerous chronic diseases, therefore elderly patients and especially senile age are characterized by high comorbidity, the prevalence of which reaches 62% among 65-74 years old people and 82% among people ≥85 years old [2-3].Researchers have made numerous attempts to quantify the clinical and prognostic significance of patients with comorbid pathology for the last decades [4-7]. A number of indices and systems have been developed for this purpose. One of the most popular in clinical practice is the Charlson Index [8-9].Comorbidity affects the prognosis for life, increases the likelihood of death. The presence of comorbid diseases increases bed days, increases disability, prevents rehabilitation, increases the number of complications after surgical interventions, and increases the likelihood of falls in the elderly people [10-11,8,12].Thus, the presence of comorbidity should be considered when choosing a diagnostic algorithm and treatment plan for a particular disease. The presence of comorbid pathology leads to greater economic costs than in the treatment of a single nosology [13-15]. All of the above mentioned shows the need to pay a great attention to the comorbid pathology of patients with a surgical profile.Aim of the research is to study the factors affecting the choice of tactics and methods for treating femoral neck fractures in elderly and senile patients taking into account the level and severity of comorbid pathology.
2. Material and Methods
Analysis of the frequency and level of comorbidity in elderly patients with a femoral neck fracture treated in the Department of Adult Traumatology of the Republican Research Center of Emergency Medicine (RRCEM) and the Department of Adult Orthopedics of the Republican Specialized Scientific and Practical Center of Traumatology and Orthopedics (RSSPCTO) for the period of 2016–2018 was carried out. Anamnestic, clinical and instrumental data were taken into account. The profile of concomitant somatic pathology was also studied. 201 history cases were analyzed. There were 82 males (40.8%) and 119 females (59.2%). The age of patients ranged from 60 to 93 years (mean age - 71.4 ± 7.1 years). Femoral neck fractures resulting from minimal trauma were noted in all treated patients. We used the Garden classification (1961), which was important in the choice of treatment tactics in detailing damage to the proximal femur. Depending on the type of fractures according to the Garden classification, patients were distributed as follows: type I - 67 (33.3%); type II - 43 (21.4%); type III - 35 (17.4%) and type IV - 56 (27.9%). According to the treatment tactics, patients were divided into three groups: conservative treatment - 54 (26.9%); operative treatment (osteosynthesis) - 81 (40.3%) and total hip replacement - 66 (32.8%). Among the concomitant diseases, first of all, the presence of cardiovascular diseases and their complications (myocardial infarction and acute cerebrovascular accident (ACVA), cerebral atherosclerosis (CAS) with dementia development), pathologies of the bronchopulmonary system, digestive tract, kidneys, and the presence of diabetes mellitus. The estimation of comorbidity was carried out using special comorbidity indices — the Charlson index proposed for assessing the long-term prognosis of patients [9] and the Cumulative Illness Rating Scale (CIRS) index [16].
3. Results
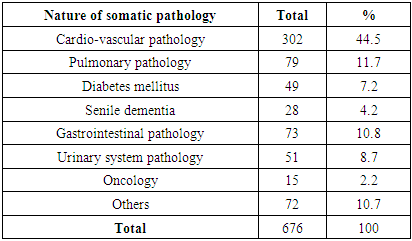
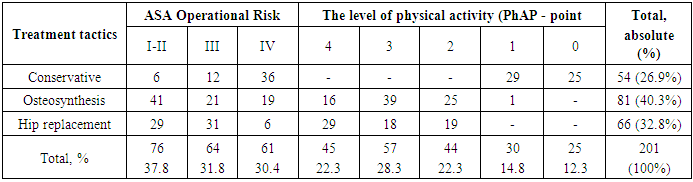
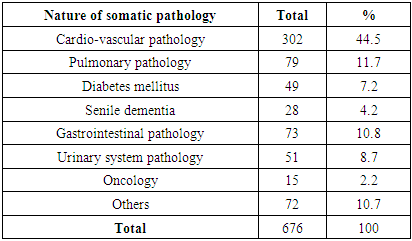
When evaluating the comorbidity indices, its high indicators were found, since the mean age of the patients included in the study was 71.4 ± 7.1 years. Concomitant diseases developed before the moment of the injury occurred in all patients. We took into account only the pathology that required medical correction and had an impact on the severity of the patients' condition, the choice of treatment tactics, the degree of physical activity, as well as on the quality of life before the injury (Tab. 1.).Table 1. The nature and frequency of the identified concomitant somatic pathology (n = 201)
 |
| |
|
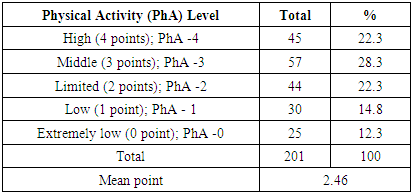
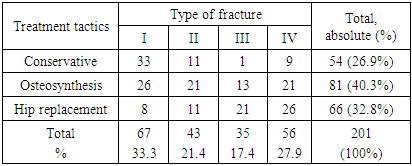
As it can be seen from the table, 676 concomitant diseases were revealed in patients (3.4 pathologies per patient at average). The greatest number of observations was made by the pathology of the cardiovascular system - 302 (44.5%), then the pulmonary pathology - 79 (11.7%) and the pathology of the gastrointestinal tract - 73 (10.8%). Blood diseases, collagenoses, diseases of the sensory organs, osteoarthritis and one case of AIDS (72 (10.7%) cases) were referred to others. The Charlson comorbidity index averaged 9.12 ± 1.05 points. To facilitate the interpretation of our data, the indicators of comorbidity, depending on the amount of points, were divided into three levels: low (up to 4 points) - 45 (22.4%); middle (5-10 points) - 97 (48.3%); high (more than 11 points) - 59 (29.3%) observations. Evaluation of comorbidity using the CIRS index allowed us to estimate not only the presence of concomitant pathology, but also its severity. The CIRS comorbidity index among patients included in the examination made up 16.2 ± 3.9 points on average. We used the division into three levels to interpret the CIRS comorbidity index: low (up to 10 points) -51 (25.4%) cases; middle (11-20 points) - 86 (42.8%); high (more than 21 points) - 64 (31.8%) observations.One of the important factors in determining treatment tactics is the degree of motor activity of patients in the period before the injury. We took the 5-point scale as a basis: high level of motor activity (4 points); middle level (3 points); limited level of activity (2 points); low activity level (1 point) and extremely low level (0 point) [1].The main contingent of treated patients (147 (73.1%)) consisted of individuals with a high level of physical activity which was important when choosing active surgical treatment tactics (Tab. 2).Table 2. Estimation of patients’ physical activity level before the injury (according to anamnesis)
 |
| |
|
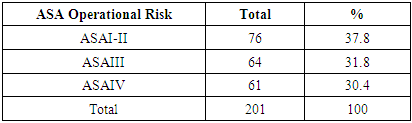
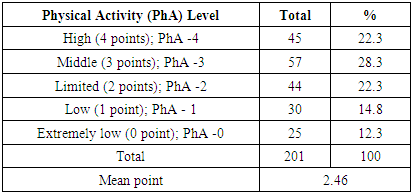
In addition to standard clinical and instrumental methods of investigation and examination of related specialists, all hospitalized patients, regardless of the upcoming treatment tactics, were examined by an anesthesiologist. The specialists took into account three main criteria when determining the operational-anesthetic risk: the general condition of the patient at the time of hospitalization, the volume and nature of the upcoming surgery, the nature of anesthesia. We used the classification of the American Society of Anesthesiologists (ASA) for the estimation of patients’ physical condition in our hospital. According to the ASA classification, there were no severe patients of class V in our clinical material. The main contingent of patients - 140 (69.6%) - were assigned to I, II, III level of anesthesiologic-operational risk, who had no significant limitations in the choice of methods for surgical correction of injuries (Tab. 3).Table 3. Distribution of patients by operational risk level
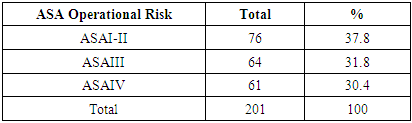 |
| |
|
4. Discussion
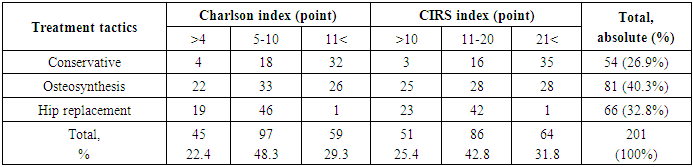
A retrospective analysis of the case histories of patients with femoral neck fractures of the older age group revealed a direct dependence on the choice of tactics and treatment methods depending on the age, somatic status, degree of comorbidity index, level of physical activity, level of operational risk for ASA, as well as depending on the type of fractures according to the Garden’s classification. Depending on the treatment tactics, patients were divided into three groups: conservative treatment - 54 (26.9%); operative treatment (osteosynthesis) - 81 (40.3%) and total hip replacement - 66 (32.8%). The choice of treatment tactics based on the level of comorbidity is presented in Table 4.Table 4. Justification of treatment tactics based on comorbidity indices
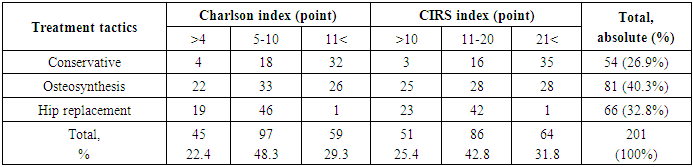 |
| |
|
A conservative method of treating patients was justified by a high comorbidity index and an unfavorable prognosis of survival. So, the Charlson index was more than 11 points in 32 (59.3%), and the CIRS index of more than 21 points in 35 (64.8%) patients. The comorbidity indices in the group of patients who underwent surgical interventions - osteosynthesis with the use of minimally invasive technologies were significantly better: high rates of Charlson and CIRS indices were observed in 26 (32.1%) and 28 (34.6%) cases. But in patients who were performed total hip replacement, a high level of comorbidity was at a minimum level of 1 (1.5%).High levels of comorbidity corresponded to indicators of the physical condition of patients at the time of hospitalization. At the estimation of the level of operational-anesthetic risk according to the classification of the American Society of Anesthesiologists (ASA), a high operational risk (IV) was observed in the group of patients performed conservative therapy - 36 (66.6%). We observed a direct relationship between the level of comorbidity, the degree of anesthetic risk according to ASA and the anamnestic data of physical activity level (Tab. 5). Low and extremely low levels of physical activity were revealed in the group of patients with conservative treatment. Thus, in patients with low and medium levels of comorbidity (group with a positive survival prognosis) there was an opportunity for active surgical treatment tactics.Table 5. Justification of treatment tactics based on the level of physical activity and anesthetic risk by ASA
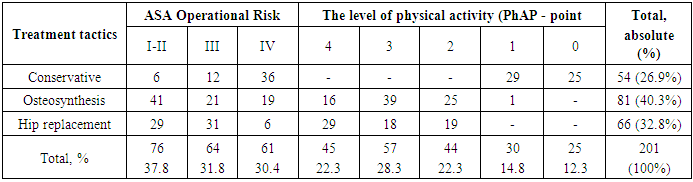 |
| |
|
Along with the somatic status of patients, we took into account the nature of the fracture at choosing treatment tactics - we used the Garden classification for it (Tab. 6).Table 6. Justification of treatment tactics based on the type of fracture according to Garden classification
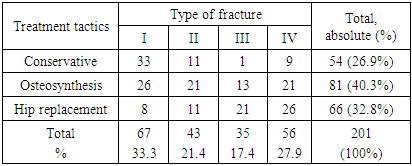 |
| |
|
The analysis showed that a conservative treatment option - an orthopedic regimen with a deratization boot was used in 54 (26.9%) patients, the reason for choosing the tactics was the concomitant severe somatic pathology, low physical activity of the patients, and type I of fractures, favorable in the orthopedic plan, in 33 (61.1%) of patients. Osteosynthesis was performed in 81 (40.3%) patients, in 63 (77.7%) of them closed cortical osteosynthesis with the use of conjugated screws (most of them for type I and II fractures) was performed. In 18 (32.3%) cases, we used the method of closed intramedullary osteosynthesis with the “Gamma” blocking system. Total hip arthroplasty was performed in 66 (32.8%) patients, mainly at the fractures of type III and IV.Thus, comorbidity affects almost all patients, the level of which increases with age and becomes one of the leading problems in the providing of specialized trauma care for the femoral neck fractures. It is always necessary to take into account the high risk of unfavorable complications development at all stages of treatment when choosing treatment tactics. We fully agree with the opinion of experts that, in order to increase the effectiveness of treatment, it seems appropriate to single out the following stages of management of a comorbid patient:- a thorough collection of complaints and medical history for all diseases, accounting and estimation of risk factors, evaluation of the stage comorbidity evolution;- isolation in the formulation of the diagnosis of main disease, concomitant diseases and associated conditions; conducting consultations or joint examinations with specialists of other profiles (cardiologist, gastroenterologist, pulmonologist, urologist, endocrinologist, surgeon and others according to indications);- identification of changes in systems and organs caused by diseases, for which diagnostic measures are necessary;- development of treatment tactics and patient follow-up [14-15].Summing up, it should be emphasized that practicing traumatologists should take into account the comorbid background in patients and strictly individualize approaches at choosing treatment tactics.
5. Conclusions
In elderly and senile patients with injuries of the femoral neck concomitant pathology corresponding to an increase in the level of comorbidity was revealed in all cases. At choosing treatment methods, it is necessary to take into account the age of the victim, the level of comorbidity, the degree of physical activity before the injury, the degree of operational-anesthetic risk and the type of fracture.At the current stage of development of traumatology, the most promising method of treating patients with fractures of the femoral neck in elderly and senile patients is hip arthroplasty. It should be performed with adequate technical equipment, after preliminary preparation of patients and at the earliest possible time, before the development of complications.
References
| [1] | Yakimov L.A. "The treatment of fractures of the hip joint in the early post-traumatic period" / Dis .... doct. Medical sciences. M., -2007. –P. 306. |
| [2] | Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012; 380(9836): 37-43. doi:10.1016/S0140-6736(12)60240-2. |
| [3] | Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American geriatrics society expert panel on the care of older adults with multimorbidity. J Am Geriatr Soc. 2012; 60(10): E1-E25. doi:10.1111/j.1532-5415.2012.04188.x. |
| [4] | Vertkin A. L., Skotnikov A. S. “Comorbidity”. The attending physician, 2013; No. 6, P.66-69. |
| [5] | Nurgazizova AK, The origin, development and modern interpretation of the concepts of “Comorbidity” and “Polymorbidity”. Kazan Medical Journal, 2014.; P. 292-296. |
| [6] | Zhuravlev Yu. I., Tkhorikova V. N. "Modern problems of measuring polymorbidity." Scientific statements of BelSU. Series Medicine. Pharmacy, 2013; 11 (154), Issue 22, P.214-219. |
| [7] | Oganov R. G. “Cardiovascular diseases at the beginning of the XXI century: medical, social, demographic aspects and ways of prophylactics” http://federalbook.ru/files/FSZ/soderghanie/2013/IV/Oganov.pdf. |
| [8] | Shirinsky V.S., Shirinsky I.V., “Comorbid diseases are an actual problem of clinical medicine” Siberian Medical Journal. 2014, Volume 29, No 1. P.8-11. |
| [9] | Charlson M.E., Pompei P., Ales K.L. et al. (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chron. Dis., 40: 373–383. |
| [10] | Ginard K. N. "When one interferes with the other - comorbidity on the wickedness of the day." New Millennium Medicine, 2012; No. 6, P. 22-24. |
| [11] | Shemetova G.N. “Approaches to the management of patients with comorbid conditions,” Saratov, 2016. P.1. |
| [12] | Global status report on noncommunicable diseases 2014. Attaining the nine global noncommunicable diseases targets; a shared responsibility” WHO, 2014. |
| [13] | Comorbid pathology in clinical practice. Clinical recommendations. Cardiovascular Therapy and Prevention. 2017; 16(6): 5-56. https://doi.org/10.15829/1728-8800-2017-6-5-56. |
| [14] | Styazhkina S.N., Chernyshova T.E., Ledneva A.V. “Comorbidity in surgical practice”, 2012. P. 43-44. |
| [15] | Styazhkina S.N., et al. "The role of comorbid pathology in surgery." Science, education and culture. 2017, P. 82-83. |
| [16] | Huntley AL, et al. Measures of Multimorbidity and Morbidity Burden for Use in Primary Care and Community Settings: A Systematic Review and Guide. Annals of Family Medicine. 2012; 10 (2): 134-41. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML