-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(8): 547-551
doi:10.5923/j.ajmms.20201008.02

Impact of Non-motor Symptoms on the Quality of Life in Parkinson's Disease Patients
Rakhmatova S., Akhmatova N., Pulatov S., Akhmatova G.
Bukhara State Medical Institute, Republic of Uzbekistan, Bukhara
Correspondence to: Akhmatova N., Bukhara State Medical Institute, Republic of Uzbekistan, Bukhara.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Parkinson’s disease (PD) affects about 1–2% of the population over 65 years of age and up to 3–5% of people 85 years of age and older. PD is a neurodegenerative disease characterized by a combination of motor and non-motor symptoms. NMS contribute to overall healthcare costs and have a profound impact on the quality of life of both patients and caregivers. Their improved management has been identified as a major unmet medical need. The main clinical symptoms of PD are well understood, but it is necessary to continue studying the changes of symptoms as it progresses. The nonmotor symptoms (NMS) of Parkinson’s disease (PD) are important factors for quality of life (QOL). Few studies on NMS have been conducted in Asian PD patients. The aims of the research. To study the structure of non-motor symptoms (NMS) at the early and last stages of PD, to determine the frequency and clinical significance of the NMS at different stages of PD, comparing the severity of NMS in PD with the severity of the same symptoms in the natural aging, to study the quality of life (QOL) of patients with the impact assessment of the NMS and the assessment of motor symptoms on this features. The material and methods. The study included 40 patients with PD and 15 patients without neurodegenerative disorders (control group). The degree of movement disorders severity was assessed using UPDRS scale. Cognitive function was assessed using the Montreal Cognitive Rating Scale (MoCA). To identify and assess the severity of NMS questionnaire used NMSS. Assessment of quality of life of patients was carried out by PDQ-26 questionnaire. Results. There was a significant difference between the intensity of the NMS in PD patients and the control group. Intensity of NMS significantly correlated with disease stage, disease duration, with the points on the UPDRS scale. NMS had at least some impact on quality of life for 84% of the respondents; 48% indicated that NMS represented a greater challenge than motor symptoms. Conclusion. NMS significantly affect the quality of life, their severity and structure varies considerably from early to late stage PD, and they are the result of a neurodegenerative process, and not the natural aging process.
Keywords: Parkinson’s disease (PD), Non-motor symptoms (NMS), Quality of life (QOL)
Cite this paper: Rakhmatova S., Akhmatova N., Pulatov S., Akhmatova G., Impact of Non-motor Symptoms on the Quality of Life in Parkinson's Disease Patients, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 547-551. doi: 10.5923/j.ajmms.20201008.02.
Article Outline
1. Abstract
- Parkinson’s disease (PD) affects about 1–2% of the population over 65 years of age and up to 3–5% of people 85 years of age and older. PD is a neurodegenerative disease characterized by a combination of motor and non-motor symptoms. NMS contribute to overall healthcare costs and have a profound impact on the quality of life of both patients and caregivers. Their improved management has been identified as a major unmet medical need. The nonmotor symptoms (NMS) of Parkinson’s disease (PD) are important factors for quality of life (QOL). Few studies on NMS have been conducted in Asian PD patients. According to the literature, non-motor symptoms (NMS) are detected in 70-100% of patients with PD [1].Such symptoms like sleep disturbances, gastrointestinal tract (GIT) and bladder dysfunction, fatigue, were identified and described by James Parkinson in 1817. In recent years, interest in NMS increased, due to studies proving their appearance at the premotor stage long before the development of motor manifestations, and accordingly, the possibilities based on this early diagnosis of PD.Some NMS can be considered as clinical markers for preclinical diagnosis of PD, as in the studies of Braak N. their appearance is proven long before motor disturbances. In this regard, they talk about the "premotor stage", which may be characterized by the appearance of such symptoms like anosmia, gastrointestinal dysfunction, pain manifestations, sleep disturbances [2]. The absence of specific symptoms makes clinical diagnosis PD at the "premotor" stage is almost impossible. Nevertheless, examination of patients with similar disorders using functional methods of neuroimaging and laboratory methods diagnosis, especially if they have relatives suffering from PD, is a promising way to identify PD as early as possible. Duration according to various sources, the preclinical stage of PD is from 3 to 10 years [3,4].It is especially important to note the role of primary care physicians in the early diagnosis of such “premotor symptoms”, and therefore in the early diagnosis of PD. Improvement diagnostic methods for NMS at the earliest stages diseases are also promising in terms of further expanding the capabilities of neuroprotective therapy.So currently being discussed the role of NMS as markers of risk groups for PD, and in their further use to assess and predict the development of the disease. It is distinguished 4 groups of NMS: vegetative manifestations, cognitive and mental symptoms, sleep disturbances. While the motor subtypes of PD long recognized and studied, recent clinical and neurobiological studies show the existence of separate, non-motor, subtypes of PD, and also suggest the possible presence of "phenotypes of NMS that dominate PD" mainly in patients at an early stage of PD [5].However, data on the structure and severity of NMS at various stages of PD and their relationship with motor impairment and disease duration are very controversial. Thus more a detailed study of these characteristics will contribute to the identification and study of non-motor phenotypes of the disease.It should be noted that 61% of patients do not tell their attending neurologist about problems such as apathy, sexual dysfunction, pain, sleep disturbances, not knowing about their possible connection with PD [6]. Hence, these symptoms, when not detected, continue to reduce the QOL of patients and can cause unreasonable hospitalization in therapeutic hospitals. As the disease progresses, non-motor manifestations, which can more strongly affect the quality of life (QOL) of patients than the classic motor symptoms of PD. Over the last years much attention has been paid to the assessment the impact of diseases on the quality of life of patients, since the concept of QOL is based on the concept of holistic approach to the patient, not only examining the patient through the prism of the main clinical manifestations, but also including various aspects of his condition as a person [7].Non-motor disorders in patients with PD, especially in the late stages of the disease, can lead to serious complications: strokes, pneumonia, intestinal obstruction, delay urination and hydronephrosis. Therefore, the study of NMS in PD is relevant and social significant problem.
2. The Aim of the Study
- To study the structure of the NMS, their frequency and clinical significance at different stages of PD; compare the severity of the NMS in PD with the severity of similar symptoms of natural aging; evaluate QOL patients with an assessment of the effect of non-motor and motor manifestations of the disease on this criterion.
3. Materials and Research Methods
- The study was conducted on the basis of the neurological department of the clinic MBRH (Multifunctional Bukhara Regional Hospital) in the period from September 2018 to May 2019. When performing the work, we used the data of medical history, medical documentation, complete neurological examination, instrumental examination and assessment by specialized scales of 40 patients with PD (25 men, 15 women). Motor severity disorders was assessed using the Unified Parkinson's Disease Rating Scale (UPDRS). Cognitive function was evaluated using Montreal Cognitive Assessment Scale (MoCA). Depression was assessed on the Beck’s Depression scale. To identify and evaluate expressions of NMS used special scales created by the European Parkinson's Disease Association: Non-motor symptoms questionnaire survey (NMSS) and NMS questionnaire. The assessment of QOL of patients was performed using PDQ26 questionnaire validated with respect to PD, in which a maximum of 100 points indicates very low QOL.
|
4. Results
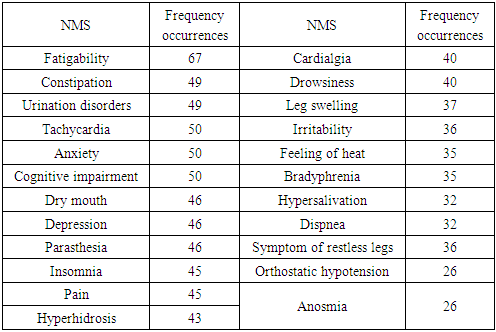
- In the sample we are analyzing the average age was 62.2 ± 8.8 years, stage by Hoehn and Yahr. The debut of the disease as observed at an average of 58.1 ± 9.7 years. The duration of the disease was from 0.5 to 15 years, the average duration of the disease is 5.1 ± 4.7 years.Analysis of the distribution of patients depending from the clinical form of PD showed significant the prevalence of the rigid-trembling form of the disease in the study sample (67% of cases).When evaluating cognitive functions, 54% of the subjects had less than 26 points on the MosA scale, the average score was 24.6 ± 3.4. The severity of cognitive dysfunction significantly correlates with the stage diseases (r = 0.28, p≤0.05), but the dependence of cognitive functions on motor disorders (r = 0.20) and disease duration (r = 0.06) statistically insignificant. Depression Testing Beck found: 34.2% had no depression patients mild depression in 30.1%; moderate depression in 6.9%; severe depression in 17.8%; severe depression (more than 30 points on a scale) in 11.0% of respondents. The average value of the level of depression (n = 40) is 15.2 ± 9.9 points. The correlation dependence of the severity of depression in points on the Beck scale from the stage (r = 0.35, p≤0.05), the duration of the disease (r = 0.36, p≤0.05), movement disorders on the 3rd part of the UPDRS scale (r = 0.33, p≤0.05). NMS were found by us in all patients in the study group. The most common which were: fatigue (67%); constipation, impaired urination (49%); anxiety, cognitive impairment, tachycardia (50%); dryness during mouth, depression, parasthesia (46%); insomnia (45%) (tab. 1). In the study, all patients had more than one NMS, and more than 50% patients had a combination of about 10 symptoms.When analyzing NMS, depending on the stage of the disease, it was found that the structure of these symptoms differs at different stages. Stage I PD is characterized by the predominance of fatigue, tachycardia, anxiety; at stage II more often detected fatigue, urination disorders, anxiety; symptoms of stage III: fatigue, disorders urination, constipation, cognitive impairment, dry mouth Stage IV: fatigue, orthostatic hypotension, insomnia, hyperhidrosis.
|
5. Discussion
- The indicators we analyze samples, such as average age, average disease duration, disease onset, are consistent with most studies.The predominance of the rigid-trembling form is also demonstrated in a large number of works [9]. Assessment of cognitive functions showed that more half of the patients (53%) had a cognitive decline of varying severity. In the analysis of this sample, an increase in cognitive impairment with an increase in the stage of the disease. A study showed the presence of depression in 65.8% of patients, while severe depression was noted in 11% of respondents.The severity of depression corelates with the progression of the disease, aggravation of motor impairment, duration of illness. On the one hand, an increase in motor manifestations enhances the severity of this symptom, but with another - the presence of depression can worsen motor dysfunction and significantly affect the social activity of patients, worsening QOL.It is established that, despite the non-specificity NMS, they are obligate signs of PD. All non-motor manifestations were revealed in all patients, in the vast majority patients (62%) had a combination of more than 10 different symptoms (e.g., hyperhidrosis, dryness in the mouth, constipation, impaired urination, tachycardia, anxiety, fatigue, drowsiness, impaired memory, parasthesia, pain), which was radically different from the control group. Structure and severity of NMS vary depending on stage of the disease. In the early stages of PD, more often symptoms such as fatigue and anxiety, while in the later stages vegetative symptoms come to the fore (constipation, hyperhidrosis, orthostatic hypotension and etc.). Nevertheless, any characteristic symptom complex of NMS disease at different stages we have not been identified. The most common symptom identified in our study is fatigue (67%). According to the literature, this indicator is 2 times higher frequency in the corresponding age population.Like many other NMS, fatigue may precede the onset of motor symptoms of the disease [10]. An analysis of the data showed that, despite the presence of similar symptoms in the structure of complaints control group (individuals with natural aging), the severity of NMS in the two groups is significantly different, with its undoubted predominance in patients with PD. In the study sample was not found the influence of gender, age on the severity of NMS, which coincides with studies of others authors [10]. As the disease progresses, its duration increases, it grows motor impairment increases and severity NMS, which significantly affects the QOL of patients. In this case, the effect of the severity of the complex NMS on QOL is more significant than the effect of motor symptoms. Considering an obvious increase in the average QOL of patients with an increase in the stage of PD, we can judge deterioration of QOL in the later stages of the disease according to compared to earlier.There remains a need to more clearly assess both the psychological distress and functional impact caused by NMS in PD. Investigations are underway to identify potential risk factors and predictors of specific NMS, and how various NMS cluster, as well as their underlying pathophysiology. Future studies could potentially seek to identify patient and caregiver characteristics that influence their perception of impact of NMS and look for modifiable factors. The effects of non-pharmacologic interventions, such as individual and couples psychotherapy, exercise, and meditation need to be assessed. In addition, a better understanding of the impact of various NMS can also help direct development of future pharmacologic treatments.
6. Conclusions
- Thus, non-motor disturbances are characterized by a wide variety of manifestations and combinations, and their structure varies significantly from early to late stage of PD. Availability of NMS is an obligate sign of PD. Although the structure non-motor manifestations of the disease is not specific, noteworthy combination most patients have more than ten different non-motor symptoms that do not occur with natural aging. NMS significantly affect QOL, in significantly disability of patients.It is necessary to evaluate the cognitive functions of patients with PD to prevent development of severe cognitive impairment. It is also important to pay attention to the state of the emotional sphere, especially depression, in order to limit the effect of this symptom on the social and motor activity of patients. The possibility of communication is discussed in the literature. NMS in PD with natural aging processes. Analysis of the obtained data showed the absence of dependence of the studied NMS on the age and gender of patients and a significant difference symptoms in the main and control groups, which confirms the available information that the NMS are a consequence of the neurodegenerative process inherent in PD.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML