E. Yu. Valiev, O. N. Nizov, A. D. Ismailov
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
This article is devoted to one of the actual issues of modern traumatology and angiosurgery - the possibility of performing primary reconstructive operations for complete and incomplete amputations, open and closed fractures and dislocations of the upper and lower extremities bones in conditions of impaired blood circulation. The authors presented the treatment results of 110 patients with open combined bone-vascular injuries of the upper and lower extremities for the period from 2015 to 2019 at the Republican Research Centre of Emergency Medicine. We managed to save the lives of 65 (69.1%) patients and to save the injured segments.Indications for performing primary reconstructive surgeries at open combined bone-vascular injuries of the extremities with circulatory disorders were, first of all, the stable general condition of the patient, as well as the safety of the injured segment. Such operations are possible only in conditions of stable hemodynamics, against the background of adequate pain relief and massive infusion therapy. When choosing a treatment tactic in the presence of combined injury, priority is given first to life-threatening injuries to internal organs and traumatic brain injury. Restoration of adequate blood circulation is the main condition for maintaining the damaged segment of the extremity and a smooth postoperative course.
Keywords:
Bone-vascular injury of the upper and lower extremities, Open fracture, Closed fracture, Dislocation, Complete amputation, Incomplete amputation, Osteosynthesis, Arterial anastomosis, Autovenous prosthetics
Cite this paper: E. Yu. Valiev, O. N. Nizov, A. D. Ismailov, Our Experience in the Treatment of Combined Bone-Vascular Injuries of the Extremities, American Journal of Medicine and Medical Sciences, Vol. 10 No. 8, 2020, pp. 539-546. doi: 10.5923/j.ajmms.20201008.01.
1. Introduction
Currently, the problem of treating open bone fractures of the lower extremities, complicated by injury of the great vessels is quite relevant. The creation of a large number of various kinds of private enterprises, non-compliance of safety regulations, as well as a significant increase of traffic accidents inevitably lead to both an increase in the total number of severe injuries of the upper and lower extremities, and to an increase of the injuries nature themselves.Currently, vascular injury at extremities bones fractures is noted in 0.6-10% of cases making up 4-5% at average [1-2]. Before the modern development of vascular surgery ligation of the injured vessel was the only treatment method. That treatment tactics was accompanied by a number of complications, one of which was a gangrene and, as a result, amputation of the extremity. Due to the rapid development of angio- and microsurgery, early timely diagnostics (pulse oximetry, MSCT-angiography, CDS) and, as a result, timely performing of reconstructive surgeries, the frequency of amputations has been significantly decreased. Nevertheless, despite the successes achieved, there is a high frequency of amputations (3-60%) and lethal outcomes (7.3-24.0%) [3-4]. If at open bone-vascular injuries, the diagnostics of vascular injury, as a rule, is not difficult, then during closed fractures and dislocations, the fact of vascular injury is sometimes ascertained belatedly. It often leads to irreversible consequences. According to some authors data, vascular damage in closed and open fractures more often occurs with fractures of the surgical neck of the shoulder, supracondylar fractures of the hip, femoral fractures in the lower third, metaphysical fractures of the tibia in the upper third, dislocations of the lower leg. So, a supracondylar fracture of the shoulder is accompanied by an arterial injury in 8%, a hip fracture in the lower third - in 11%, a dislocation of the lower leg - in 8%, an intra-articular fracture of the tibia - in 19% [5]. However, these statistic data mainly reflect damage options due to the indirect mechanism of injury (falling from a height or at the time of a car hit). At the direct mechanism of injury (damage on machines, with chopping object), combined damage of bones, blood vessels and nerves, as well as muscle-tendon structures can be at any level. The most severe are traction-crushing injuries characterized by multiple fractures and dislocations, the presence of extensive torn-crushed, often contaminated wounds, multiple ruptures and tears of muscle structures, multifocal injuries of blood vessels and nerve [3,6].In case of bone-vascular injuries, their absolute majority is accompanied by shock, blood loss and extremity ischemia which causes a large number of diagnostic and tactical errors both at the prehospital and hospital stages and is the cause of a significant number of postoperative complications. Severe combined injuries (injuries of the chest, abdomen, pelvis, traumatic brain injury), which occur in 12.5% of victims on average, complicate not only the diagnostics, but the choice of the optimal treatment tactics [1]. That is why the attitude of angiosurgeons and traumatologists towards reconstructive operations on the main vessels of the lower extremities is quite cautious, which is justified. The risk of complications after reconstructive surgeries on the main vessels is higher, the more extensive the injury of muscle and bone tissue. The mechanism of the lower extremities injuries often makes impossible to carry out reconstructive operations at auto, rail and mine explosive injuries [7-9].When performing reconstructive operations, one should not deny the fact that the presence of large muscle masses in the lower extremities increases the possibility of postoperative suppuration and the risk of “transplant toxicosis”, which poses a direct threat to the patient’s life. This causes the statement of R.O. Datiashvili about the inappropriateness of revascularizing operations in case of injuries proximal to the lower third of the thigh and upper third of the shoulder [6]. in such a situation, the operating surgeon faces a dilemma: performing reconstructive surgery or performing primary amputation of a segment for saving the patient's life. Moreover, the time to make a final decision is short. Most authors agree that the priority is always to preserve the patient's life. It is very difficult to develop a universal algorithm that takes into account all the main points of diagnosis and treatment. It is an individual approach in each individual case, taking into account the mechanism of injury, the nature of injuries, the presence of damage to internal organs, the degree of traumatic and hemorrhagic shock, the conditions for performing reconstructive surgeries are the basis for making the right decision [6,10].When performing reconstructive surgery on the extremities, first of all, the correct choice of the osteosynthesis method, the method of applying vascular anastomoses and also the closure of postoperative wounds is important. Conditions for simultaneous restoration of all damaged structures (muscles, tendons, nerves) are not always available. Nevertheless, there is still no consensus among some authors about the priority of osteosynthesis and vascular reconstruction. The majority of authors believe that osteosynthesis should be performed in the first place –it creates favorable conditions for the restoration of the vessel and reduces the likelihood of its injury and thrombosis [3,6,11]. In contrast, Sriussadaporn S. at closed combined injuries of the lower extremitiesarteries in 10 of 18 cases initially restored arterial perfusion and then he performed osteosynthesis. The authors of this article are of the opinion of Datiashvili R.O. [6] on the priority of performing fast and reliable osteosynthesis, ensuring the subsequent vascular stage of the surgery, taking into account the possibility of subsequent correction with extra-focal fixation devices.The issue of choosing a method for stabilizing bone fragments is relevant. Intramedullary osteosynthesis has advantages over the other ones, as it provides an optimal method of immobilizing a fracture to perform reconstruction of a damaged vessel, and also promotes care and rehabilitation [12-13,6]. The methods of external non-focal fixation of fractures by rod or spoke-rod devices have obvious advantages over spoke ones, since the resistance to the action of external forces is 2.5-5 times higher [11]. External fixation can be selected for extensive soft tissue injuries, wound contamination or multi-fragmented fracture [14].Intramedullary osteosynthesis is preferred for the humerus and femur fractures, and external fixation - for fractures of the lower leg bones. Thus, there is no consensus on the issue of fracture fixation. Apparently, the choice of method for fixing bone fragments should be individual, since it depends on many factors [4,10,8].The degree of the bone shortening during osteosynthesis, as the authors believe, should be determined, first of all, by the possibility of restoration of vessels “end to end”, and the possibility of closing the wound with local tissues. A degree of the leg shortening from 5 to 8 cm is considered acceptable. Nevertheless, the use of modern microsurgical technologies (autogenous prosthetics, flap grafting on microvascular anastomoses) makes it possible to preserve the segment, and the use of orthopedic techniques can subsequently restore its length and support function [6,15,9].When choosing a method for reconstruction of blood vessels, one should proceed, first of all, from the nature and amount of their injury. They seek to restore “end to end”, adhering to the rule “for at least two large veins on one artery” at complete amputations. In the case of incomplete amputations with adequate venous return, end-to-end anastomoses of arteries are also preferred, autovenous or autoarterial prosthetics of arteries are performed, if necessary [6,11,15,8-9].The results of restoration of blood circulation in the segments are evaluated primarily on the base of clinical data (color and local temperature, the appearance of retrograde blood flow, filling of veins, the appearance of a pulse on the periphery, capillary tests).As additional research methods, the most informative in emergency surgery are pulse oximetry, Color Doppler Scanning (CDS), angiography [16]. In the postoperative period, adequate drug therapy, aimed at replenishing the volume of circulating blood, reducing blood coagulation, stabilizing hemodynamic parameters, improving blood rheological properties and also preventing infection has a primary importance. Despite successful reconstructive surgeries on the extremities vessels and the use of complex treatment methods, with the late restoration of the main blood flow with severe ischemia, various complications are developed: gangrene, intoxication, infectious complications that threaten the patient’s life or negate the results of surgical treatment [6,1,15].Thus, a number of issues remain relevant:• Express-diagnostics of vascular injury at closed and open fractures in conditions of combined trauma in the presence of traumatic shock;• Determining the priority of surgical intervention for severe combined injuries with internal organs damage;• Definition of clear indications both to reconstructive surgeries and to primary amputations.Aim of the study is to show the need for simultaneous reconstruction surgeries in patients with combined bone-vascular injuries of the extremities.
2. Material and Methods
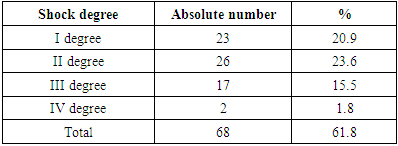
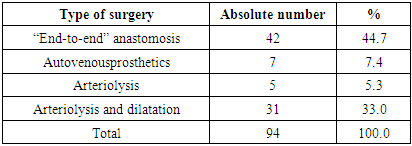
110 patients with open combined bone-vascular injuries of the upper and lower extremities were treated at the Republican Research Centre of Emergency Medicine for the period from 2015 to 2019. By the term of “bone-vascular lesions” we meant all open and closed lesions in which there were bone injuries (fractures, dislocations) and vascular injuries of various kinds. There were 57 adult men, 9 women, 44 children under 18 years old. 56 (50.9%) patients were at the age from 20 to 50 years, that is the most able-bodied. 101 (91.8%) patients were delivered within 1-6 hours after the injury (the time frame favorable for surgeries), 3 (2.7%) - within 6 to 24 hours, 6 (5.5%) - later than 1 day after the injury. 68 (61.8%) patients were delivered in a state of traumatic shock. 31 (28.2%) patients were delivered by relatives, 28 (25.5%) – by ambulance, 51 (46.4%) were transferred from other clinics. The distribution of patients according to the degree of shock is presented in Table 1.Table 1. The distribution of patients according to the traumatic shock degree
 |
| |
|
As it is seen from the table, shock of the I – II degree mostly prevailed (44.5%) and the reasons for which were bone-vascular isolated injuries of the upper and lower extremities. Shock of the III degree was more often observed in the presence of multiple injuries with the presence of extensive wounds of the thigh, lower leg and foot.The distribution of patients according to the injury mechanism is presented in Fig. 1. | Figure 1. The distribution of patients according to the injury mechanism |
In most cases (31%), injuries of the extremities were received as a result of the extremity getting into the rotating mechanisms of the machine. Injuries resulting from an accident (21%) were often combined with closed and open traumatic brain injuries of varying severity. In addition, in 8 (7.3%) cases there were closed injuries of the abdomen and chest cavity, in 2 (1.8%) cases - fractures of the pelvic bones, in 5 (4.5%) cases - traumatic brain injuries of various severity. A large percentage of bone-vascular injuries when falling from a height of growth (31%) is due to the frequency of these injuries in children. The distribution of patients according to the localization of injuries has been presented in Fig. 2. | Figure 2. The distribution of patients according to the localization of injuries |
As it can be seen in this figure, most of the injuries were localized in the shoulder (36%) and lower leg (21%). In order to analyze treatment methods and their results, patients were divided into 5 main groups according to the nature of the injuries (Fig. 3). | Figure 3. Distribution of patients into main groups |
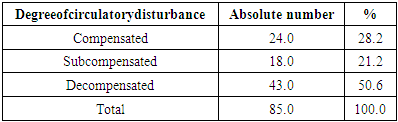
The majority of the examined patients (37%) had open fractures and dislocations with circulatory disorders, which mainly occurred at traction and crushing injuries. Complete traumatic amputations also had a traction character, which was accompanied by significant injury of the severed segments. According to the degree of circulatory disorders, patients with preserved extremities segments were distributed as follows (Tab. 2). Table 2. Distribution of patients by the degree of circulatory disturbance (patients with complete amputations were not included in this category)
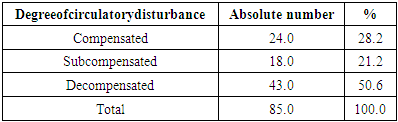 |
| |
|
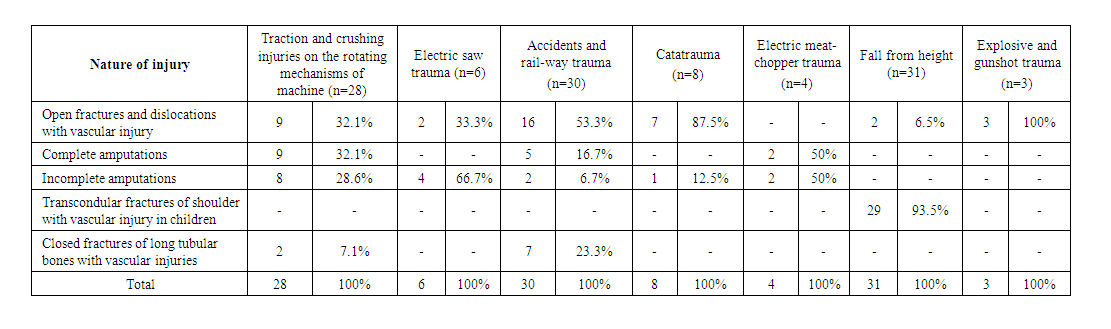
In table 3 we distributed patients according to the nature of the injury depending on the mechanism of injury. In our opinion, it has a fundamental importance.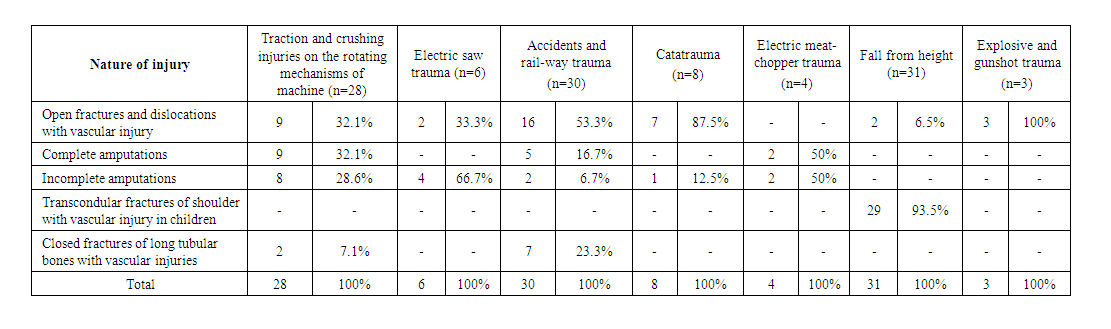 | Table 3. The distribution of patients according to the nature of the injury depending on the mechanism of trauma |
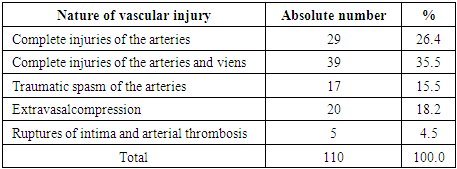
As it follows from this table, the largest number of complete and incomplete amputations (17) are traction-crushing injuries, as well as injuries sustained in electric meat chopper combining in itself traction, crushing and cutting mechanisms.The distribution of patients according to the nature of vascular damage is presented in Table 4.Table 4. The nature of vascular injury
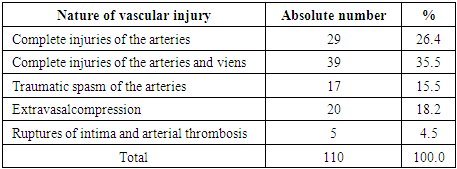 |
| |
|
Among the research methods, the main ones were clinical and biochemical blood and urine tests, as well as radiography which allowed to establish the exact location of the injury. Pulse-oximetry which allows to establish the initial degree of segment circulatory disturbance and the dynamics of its improvement was performed in 77 (70%) patients. Color duplex scanning (CDS) was performed in 15 (13.6%) cases when the condition of the patients allowed, during the first hours. It made possible to accurately determine the location of vascular injury. MSCT-angiography was performed in 7 (6.4%) patients.
3. Results and Discussion
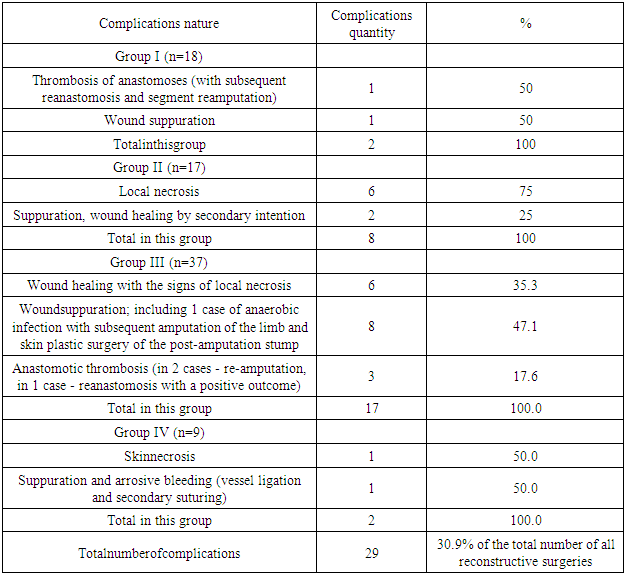
As it was mentioned above, we divided the patients into 5 main groups, depending on the nature of the injury with the aim of a comprehensive analysis.Group I included 18 (16.4%) patients with complete traumatic amputations of large segments. Complete amputations meant such injuries when the connection between the damaged segment and the extremity was either completely absent or maintained through soft-tissue bridges (including those containing tendons and nerves) that were not involved in the segment’s blood circulation. When segments were amputated, the injury of the vessels always had the character of a complete interruption. Moreover, if at the crushing mechanism of the injury, the damage of the vessel was localized, as a rule, within the wound, then, when the crush was combined with traction, it spread beyond it. The extent and degree of the intima injury was not always possible to visualize. Blood circulation was decompensated in all cases. In 3 cases complete amputations were combined with open and closed fractures of other segments, where there was also a violation of blood circulation. Soft tissue wounds were extensive, torn-bruised in nature, with extensive defects, crushing and multiple muscle ruptures.Group II included 17 (15.5%) patients with incomplete traumatic amputations of large segments. In incomplete amputations, in our cases, the connecting flaps contained only intact veins, which ensured venous outflow from the segment. Nerve injury also occurred in all cases. With traction amputations, the limb often remained only on crushed skin flaps and tendons, which was so called subtotal amputation by nature.Group III included 37 (33.6%) patients with open fractures and dislocations, accompanied by vascular injury, but not suitable for the category of “complete and incomplete amputations”. There was an injury of the muscle-tendon structures, often skin-soft tissue defects and nerve injury in these cases.Group IV included 9 (8.2%) patients with closed fractures of long tubular bones accompanied by vascular injuries. There was an injury of a significant muscle mass in these cases. Nerve injuries were not encountered or had a contusion character.Group V included 29 at the age of 4 -12 years with transcondylar fractures of the humerus accompanied by extravasal compression of the brachial artery in 20 cases and its complete injury in 9 cases.The nature of the performed operations is presented in Table 5.Table 5. The nature of performed surgeries
 |
| |
|
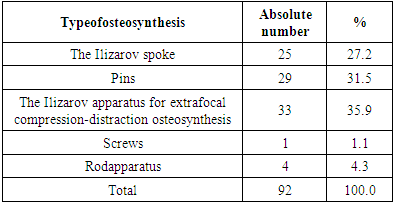
When performing osteosynthesis, we often had to resort the bones shortening in order to remove non-viable fragments, as well as to facilitate the reconstruction of the vessels and subsequent closure of the wound. The main methods of osteosynthesis are presented in table 6.Table 6. The main methods of osteosynthesis
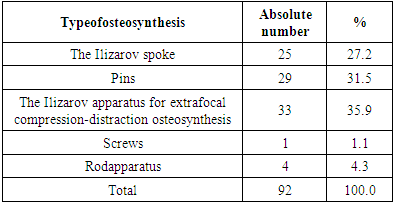 |
| |
|
As it can be seen from the tables, preference was given to intramedullary osteosynthesis during fixation of bone fragments, as the least traumatic, fastest and most reliable which allowed to save time for the subsequent performance of the vascular stage of surgeries. When applying vascular anastomoses, in most cases an “end-to-end” anastomosis was used - it made possible to reduce the time of ischemia. In this case, the bones shortening was carried out to such a length that it was possible to impose “end-to-end” vascular anastomoses, to close the wound with local tissues, if possible, and not significantly disrupt the length of the limb. Types of surgeries on vessels are presented in table 7.Table 7. Types of surgeries on vessels
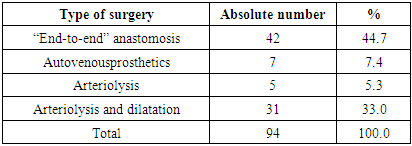 |
| |
|
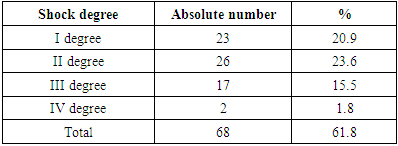
Autovenous prosthetics were performed in the presence of significant arterial defects. Great saphenous vein was used as a prosthesis in all cases. In the presence of traumatic arterial spasm, in the absence of antispasmodics effect (which often occurred at traumatic shock and unstable hemodynamics), periarterial sympathectomy with a Fogarty catheter dilatation was effective. During interposition with extravasal compression, arteriolysis was effective in the absence of artery injury signs - rupture of intima or complete interruption. Injuries of this nature required an economical resection of the artery ends followed by the application of an anastomosis. Surgeries on internal organs always preceded operations on limbs at severe combined injuries.In 3 (2.7%) cases, due to the extremely serious condition of patients (2 cases of accident and 1 catatrauma), a lethal outcome occurred in the first hours after admission. In total, reconstructive surgeries were performed in 94 (85.4%) cases. In the postoperative period, patients underwent drug therapy, including antibiotics, anticoagulants, antispasmodics, rheology-improving agents, as well as the prevention and treatment of reperfusion syndrome, hemo- and plasma transfusion. There were no postoperative complications in 65 (69.1%) cases of them: no repeated disturbance of blood circulation; wound healing was the first intention, there were no complications from osteosynthesis side. The structure of complications after reconstructive surgeries has been shown in Table 8.Table 8. Complications analysis after reconstructive surgeries
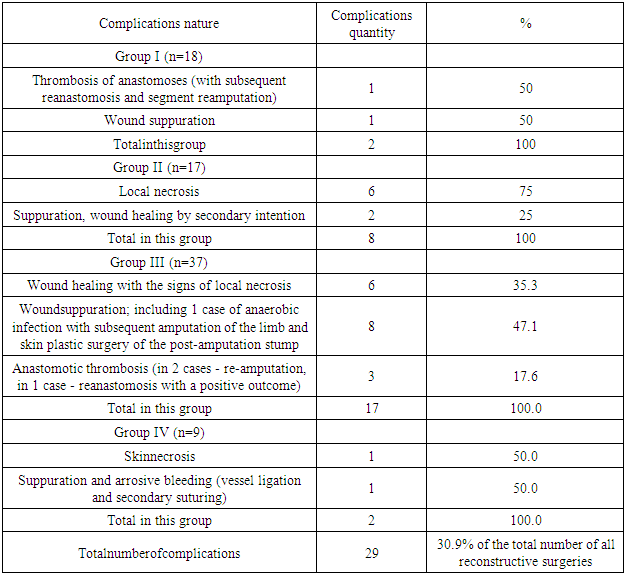 |
| |
|
Postoperative complications in all cases were developed within 2-7 days. Segment reamputation was performed in 4 (13.7% of all complications) cases. The causes of blood circulation decompensation in 3 cases were the development of secondary arterial thrombosis against the background of the periphery persistent spasm, as well as deep vein thrombosis, in 1 case - anaerobic infection. There were no postoperative complications in the Group V. There are some unresolved problems in the treatment of combined bone-vascular injuries of the extremities. First of all, the ambulance service still remains unsatisfactory. According to our data, the majority of patients, 28.2%, are delivered from the scene without proper medical care, in a state of traumatic and hemorrhagic shock. In 34.6% of cases, we had to deal with combined lesions: when, along with injuries of the lower extremities, there were closed and open craniocerebral injuries, closed injuries of the abdomen and chest. In such cases, priority was given to injuries representing a direct threat to life. In terms of diagnostics, preference was naturally given to fast-performing and non-invasive procedures.When choosing surgical treatment tactics, we proceeded primarily from the safety of the limb distal segment and the assessment of the appropriateness of reconstructive surgery. At complete and incomplete segment amputations, the volume of interventions was more extensive, since it was not only about osteosynthesis and restoration of arteries, but often veins, nerve trunks, tendons and muscles. In patients with fractures complicated by vascular injury, the aim of the operation, first of all, was to conduct reliable osteosynthesis and the application of an arterial anastomosis. One of the prior condition of osteosynthesis for successful revascularization was shortening of the bone in the segment and in the stump by a length sufficient to bring the ends of the vessels closer without tension. As for the osteosynthesis methods themselves, the spoke method of osteosynthesis is quickly feasible and slightly traumatic. But it did not always guarantee a sufficiently stable fixation, in comparison with the osseous plates and massive intramedullary pins. The last methods are more traumatic, they required more time to perform, which lengthened the terms of ischemia. In addition, they have a higher degree of risk in terms of the development of infectious wound complications. Thus, when there is a violation of the blood circulation of the segment, the most optimal is the preliminary fixation (with spokes or thin pins) of bone fragments, which is necessary for the stage of revascularization with subsequent immobilization of the limb or the application of an external fixation device after closing the wounds.In terms of revascularization, preference was given to “end-to-end” anastomoses, as the fastest, allowing to minimize ischemia time. At the same time, even despite the shortening of bone fragments, it was not always possible to bring the ends of the vessels closer together, which required the use of autovenous inserts. The attitude to this technique is also ambiguous. On the one hand, the use of free transplants in conditions of microbial contaminated wounds, and even with the implementation of two vascular anastomoses, has a high risk of thrombosis or arrosive bleeding. On the other hand, although it increased the duration of the operation, but after the restoration of adequate blood flow, there were no cases of irreversible trophic disorders in the segment and the inclusion syndrome was not observed. However, primary amputation with the formation of a stump was performed in 20 cases due to the significant destruction of the damaged segments, the presence of extensive soft tissue defects. In 4 more cases, despite thorough initial surgical treatment and restoration of adequate blood flow in the injured segment, re-amputation was performed due to the development of infectious complications. In our opinion, the reason for an inadequate assessment of the severity of the injury.
4. Conclusions
Indications for performing primary reconstructive surgeries for open combined bone-vascular injuries of the extremities with circulatory disorders are, first of all, the stable general condition of the patient, as well as the safety of the injured segment. Such surgeries are possible only in conditions of stable hemodynamics, against the background of adequate pain relief and massive infusion therapy. When choosing treatment tactics in the presence of a combined injury priority is given to life-threatening injuries of internal organs and TBI. The restoration of adequate blood circulation is the main condition for maintaining the injured segment of the limb and a smooth postoperative course.
References
| [1] | Cakir O, Subasi M, Erdem K, Eren N. Treatment of vascular injuries associated with limb fractures. Ann R CollSurg Engl. 2005 Sep; 87(5): 348-52. |
| [2] | Akhadov A.M. Features of angiosurgical care for gunshot wounds of the great vessels of the extremities in armed conflict. Abstract. dis. ... cand. med. sciences. Rostov n / a 2000; 25. |
| [3] | Fomin V.N. Treatment of injuries of the great vessels of the extremities in the conditions of the central district hospital. Herald of surgery 2008; 167 (6): 127-128. |
| [4] | Sultanov D. D., Usmanov N.U., Kurbanov A.A., Baratov A.K., Kurbanov N.R. Surgical tactics for traumatic injuries of the lower leg arteries. // Angiology and vascular surgery, 2003.-Volume 9, No. 2. P. 111-117. |
| [5] | DuduzinskyK.Yu. Arterial defect recovery in case of bone-arterial gunshot injuries of the extremities. Basicresearch. 2007; 8: 12. |
| [6] | Poyarkov V.D., Danilov V.A. Correction of blood circulation in the treatment of combined traumatic injuries of the limbs. BulVost. -Sib. Scientific Center of the SB RAMS 2007; 43: 151-151. |
| [7] | Abyshov N.S. Immediate and long-term results in traumatic injuries of arteries of the extremities. Angiol and vessel surg 2002; 8 (4): 103-110. |
| [8] | Cakir O, Subasi M, Erdem K, Eren N. Treatment of vascular injuries associated with limb fractures. Ann R CollSurg Engl. 2005 Sep; 87(5): 348-52. |
| [9] | Steinle A.V. Angiography for damage to the great vessels of the extremities (historical review). Sibmedjournal. 2008; 23 (1): 99-112. |
| [10] | Piatek S, Burger T, Halloul Z, Westphal T, Holmenschlager F, Winckler S. Arterial vascular injuries in fractures and dislocations. ZentralblChir. 2001 May; 126(5): 379-84. German. |
| [11] | Datiashvili R.O. Limb replantation. - Moscow, "Medicine". – 1991. - P.240. |
| [12] | Zhigunov A.K., Aslanov A.D., Kudryavtsev B.P. etc. Organizational diagnostic and therapeutic measures at the prehospital stage of accompanying victims with combined injuries in case of limb injuries. Disaster Med 2006; 1 -2: 34-36. |
| [13] | Afanasyev L.M., Agadzhanyan V.V., Yakushin O.A. To the question of organizing care for patients with complete, incomplete detachments and open combined damage to blood vessels, nerves, tendons of limbs. // VI Congress of Orthopedic Traumatologists of Uzbekistan - 2002. P. 11-13. |
| [14] | Zhigunov A.K. Surgical treatment of patients with combined vascular-bone lesions of the limbs. Abstract. dis. ... Doc. med. sciences. M 2007; 26. |
| [15] | Lemenev V.L., Mikhailov I.P., Isaev G.A. Treatment of patients with trauma of the main arteries of the lower extremities. // Angiology and Vascular Surgery, 2005. Volume 11, No. 3. P. 108-114. |
| [16] | Dadadzhanova F.Z. Surgical tactics for combined gunshot bone-vascular limb wounds. Abstract. dis. ... cand. med. sciences. Dushanbe 2000. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML