-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(7): 509-514
doi:10.5923/j.ajmms.20201007.14

Aspects of Early Diagnosis of Cardiac Disorders in Children with Type 1 Diabetes
Sadirkhodjaeva Azizakhon Alavitdinovna, Ashurova Dilfuza Tashpulatovna
Hematology of Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: Sadirkhodjaeva Azizakhon Alavitdinovna, Hematology of Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

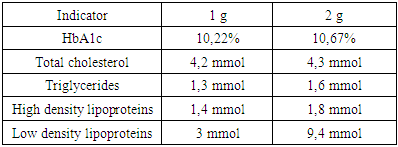
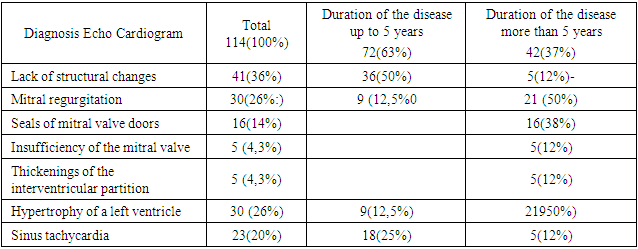
The current problem of children 's cardiology is the study of heart work change in children with type 1 diabetes mellitus (DM 1), as the development of specific heart damage is one of the causes of high mortality of diabetes patients. Heart failure develops in almost 80% of such patients. The main cause of death is cardiovascular complications, among which myocardiodystrophy most often leads to the development of heart failure and sudden heart death. Purpose. To determine the clinical value of the level of MV fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein in blood serum in children with type 1 diabetes mellitus and to assess the possibility of use in early diagnosis of cardiovascular complications. Materials and methods study. The total number of patients was 114 children with type 1 diabetes, aged between 4 and 18. We conducted laboratory and instrumental methods of research. Laboratory methods study general clinical (general blood and urine analysis, blood sugar level studies), biochemical (level of total blood protein, bilirubin, cholesterol, triglycerides, creatinine, urea, electrolytes, glycated hemoglobin), cardiology marker (MV B fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein). Conclusion. Thus, markers of cardiac complications in type 1 diabetes mellitus in children can be the MV of the creatine phosphokinase fraction, and the highly sensitive C fraction of the reactive protein, as these factors are reliably increased in the progression of cardiological disorders and can be used as a screening test at the level of the primary health care unit.
Keywords: Cardiac markers, Diabetes mellitus, Cardiovascular system, Complication
Cite this paper: Sadirkhodjaeva Azizakhon Alavitdinovna, Ashurova Dilfuza Tashpulatovna, Aspects of Early Diagnosis of Cardiac Disorders in Children with Type 1 Diabetes, American Journal of Medicine and Medical Sciences, Vol. 10 No. 7, 2020, pp. 509-514. doi: 10.5923/j.ajmms.20201007.14.
1. Introduction
- The current problem of children 's cardiology is the study of heart work change in children with type 1 diabetes mellitus (DM 1), as the development of specific heart damage is one of the causes of high mortality of diabetes patients. Heart failure develops in almost 80% of such patients. The main cause of death is cardiovascular complications, among which myocardiodystrophy most often leads to the development of heart failure and sudden cardiac death. [12,13]. Currently, the life expectancy of patients remains lower than the average population in the development of DM 1 in childhood [1]. Myocardiodystrophy most often leads to the development of heart failure, diabetic cardiac autonomous neuropathy plays a major role in the development of sudden cardiac death, arterial hypertension leads to the progression of macro- and microvascular complications of DM 1 [4,7]. Various terms ("diabetic cardiopathy," 1 diabetic cardiomyopathy, "diabetic heart", autonomous heart neuropathy, "cardiac autonomous neuropathy", diabetic heart microangiopathy, "specific diabetic heart microangiopathy", proper heart, "myocardiodystomy") are used to refer to the cardiovascular system lesion [2,4,7,9,10,13].Several pathogenetic mechanisms are involved in the development of cardiovascular disorders in DM 1, the main of which are the diffuse generalized pathological process affecting the whole microcirculation system - microangiopathy with disorders of heart muscle metabolism, changes in nervous regulation of the heart, development of changes within the framework of cardienal syndrome and endothelial dysfunction [6]. Diabetic cardiomyopathy is based on changes in cardiac vessels in the form of microangiopathies, which is accompanied by disorders of microcirculation with morphological and functional changes of myocardium. Microangiopathies are a feature of DM 1 and wear a generalized ha-racter [3]. The main mechanisms in the development of microangiopathies are the processes of pronounced non-enzymatic glycosylation of proteins, collagen, components of the clotting system, hemoglobin, etc., leading to the formation of irreversible substances in chemical reactions, called final product glycosylation [2,10]. An important role in the pathogenesis of diabetic cardiopathy is the activation of lipid peroxidation and the weakening of antioxidant protection, which leads to the accumulation of potentially toxic products of free fatty acid intermediate oxidation units within myocardiocytes, which have a detrimental effect on myocardial cells [8,10]. Recently, the development of microangiopathies in non-insulin dependent tissues in DM 1 patients is thought to have a genetic predisposition. This explains the fact that not all patients, even in the labile course of DM 1, develop microvascular complications. All the above factors are accompanied by changes in the tone and structure of the vessels of the microcirculatory channel, disruption of the rheological properties of the blood, reduction of the oxygen balance of tissues, disorders of vascular permeability and resistance. These pathogenetic mechanisms of cardiomyopathy formation in children with DM 1 cause myocardiocyte energy deficiency, which promotes development of functional and ultrastructural myocardial changes, being metabolic basis of cardiomyopathy [1,6].In the genesis of the occurrence of cardiovascular pathology in type 1 diabetes mellitus, along with the development of diabetic microangiopathy and metabolic disorders in the heart muscle, a certain value belongs to the imbalance of vegetative regulation of heart function - autonomous cardiovascular neuropathy. Diabetic autonomous cardiovascular neuropathy is characterized by disorders in the functional state of the cardiovascular system and is one of the main causes of circulatory insufficiency [5,7,8].One of the reasons for the high risk of cardiovascular complications in children with type 1 diabetes mellitus is the development of atherosclerotic process [1]. The development factors of atherosclerosis are dyslipidemia, AH, endothelial dysfunction and inflammation. In children and adolescents with DM 1, compared to peers without LED, higher levels of lipids are recorded, which are largely dependent on glycemic control. Hyperglycemia and dyslipedemia are also known as pro-inflammatory triggers of neurodegenerative processes [5,8].The desire to increase the duration and improve the quality of life of diabetes patients has brought to the fore the problem of prevention and treatment of its late complications, the number of which increases with the increase in the duration of the disease.Aim of the study was to determine the clinical value of the level of MV fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein in blood serum in children with type 1 diabetes mellitus and to assess the possibility of using cardiovascular complications in early diagnosis.
2. Materials and Methods
- In order to achieve this goal, children hospitalized in the children's departments of the Republican Specialized Scientific Practical Medical Center of Endocrinology in Tashkent were examined.The work is based on the results of clinical observations analysis in children with type 1 diabetes mellitus and the values of MV fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein in blood serum in these patients are investigated. The total number of patients who were studied was 114 children with type 1 diabetes aged between 4 and 18.Clinical diagnosis in children of type 1 diabetes mellitus was based on the collection of complaints of the patient (dry mouth, thirst, visual impairment), general complaints (fatigue, weakness, insomnia), the history of the disease - the age of diabetes mellitus, aggravated inheritance for diabetes mellitus. During an objective examination of the patient, attention was paid to the general condition of patients, physique, the ratio of height to weight, the condition of skin and mucous membranes, respiratory organs, blood circulation, blood pressure level and pulse rate, and the condition of abdominal organs was assessed.We conducted laboratory and instrumental methods of research. Laboratory methods study general clinical (general blood and urine analysis, blood sugar level studies), biochemical (level of total blood protein, bilirubin, cholesterol, triglycerides, creatinine, urea, electrolytes, glycated hemoglobin), cardiology marker (MV fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein).Methods of the statistical analysisStatistical processing of the results of the study was carried out using the program Statistica, and Microsoft Excel.Statistical analysis results could be unreliable (p > 0.1), reliable (p < 0.05), reliable with high degree of reliability (p < 0.01), reliable with high degree of reliability (p < 0.001).
3. Results and Discussion
- The results of the study of 114 children with type 1 diabetes mellitus, between the ages of 4 and 18, the average age of 12.8, showed that on admission most of the patients had subcompensation of diabetes mellitus and presented characteristic complaints of the main disease.
 | Figure 1. Distribution of patients by sex |
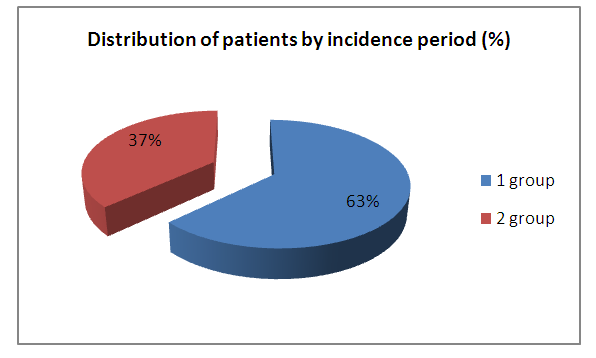 | Figure 2. Distribution of patients by incidence period |
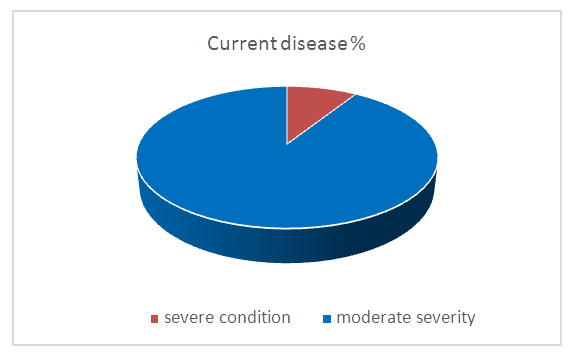 | Figure 3. Current disease |
 | Figure 4. Diabetes mellitus complications |
|
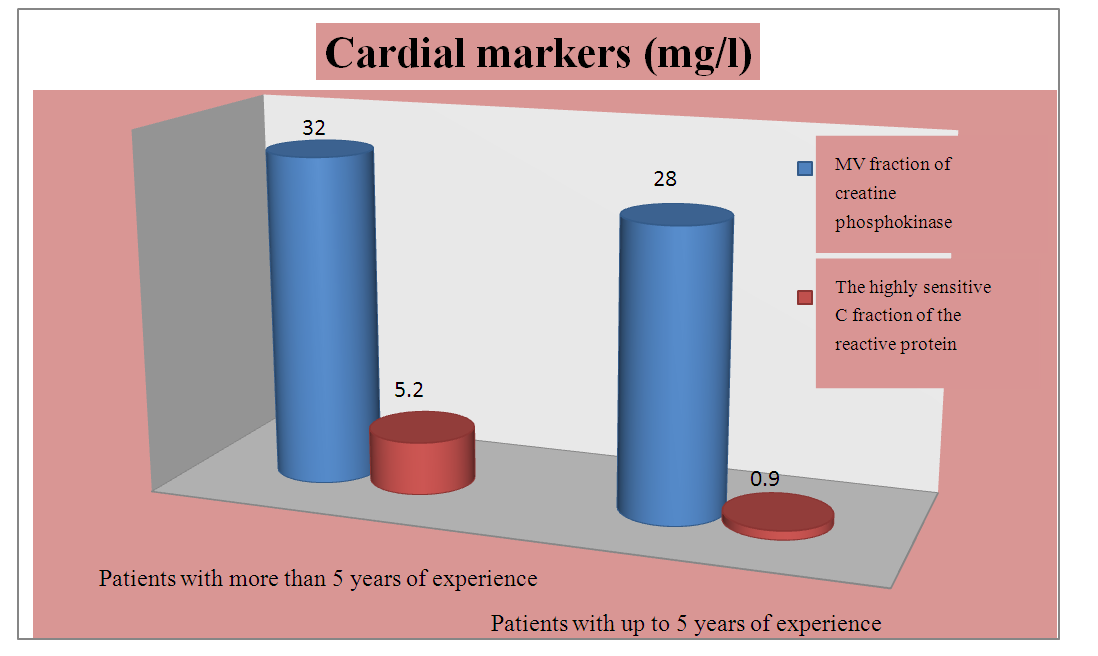 | Figure 5. Cardiac markers depending on seniority disease |
|
4. Conclusions
- 1. The MV fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein in blood serum in children with type 1 diabetes are correlated with the duration and severity of the disease.2. The index MV fraction of creatine phosphokinase and the highly sensitive C fraction of the reactive protein in blood serum in children with type 1 diabetes mellitus can be used as an additional diagnostic criterion in the early stages of cardiovascular complications of diabetes mellitus.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML