Mavlyanova Zilola Farkhadovna
Candidate of Medical Sciences, Associate Professor, Head of the Department of Medical Rehabilitation, Physiotherapy and Sports Medicine, Samarkand State Medical Institute, Republic of Uzbekistan
Correspondence to: Mavlyanova Zilola Farkhadovna, Candidate of Medical Sciences, Associate Professor, Head of the Department of Medical Rehabilitation, Physiotherapy and Sports Medicine, Samarkand State Medical Institute, Republic of Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Relevance. In children with cerebral palsy, assessing protein-energy malnutrition is not an easy task. Since the violation of the growth and development of this category of children has a multifactorial genesis, the approach to solving the issues of evaluating the nutritional status in these patients should be comprehensive. Only a comprehensive solution, taking into account clinical, neurological and anthropometric indicators, laboratory markers, as well as knowledge of the characteristics of physical development, actual nutrition, body composition in children with cerebral palsy will help reflect the real state of the nutritional status of the patient. The aim of the study was to assess the nutritional status and study the features of nutritional history in various forms of cerebral palsy. Material and research methods. The article presents the data on assessing the nutritional status and nutritional history of 65 patients with cerebral palsy from 3 to 15 years old, who made up the main group and divided into 5 subgroups depending on the form of the disease. The control group consisted of 30 healthy children, comparable in gender and age to the main group. Assessment of nutritional status was carried out on the basis of determining the weight and height of the child, the circumference of the shoulder, measuring the thickness of the skin-fat fold over the triceps, determining the absolute number of blood lymphocytes and albumin content. Results and discussion. In 63.1% of children with cerebral palsy, oral-motor dysfunction of varying severity was found, the most pronounced in the group of patients with tetraparesis (88.8%), and problems with food intake occurred in 78.7% of patients in the main group. As a result of nutritional problems in 80% of patients with cerebral palsy using the Billbreri-Cohen method, protein-energy insufficiency of varying severity was detected. Findings. The determining disorders in nutritional status in patients with cerebral palsy are additional disorders in the functioning of the body due to severe difficulties in eating directly related to a violation of nervous regulation, the main causes of which are damage to the brain centers, as well as a violation of the swallowing and chewing functions, as well as the lack of active movements, which, in turn, leads to a mismatch of eating habits.
Keywords:
Cerebral palsy, Nutritional status, Children, Protein-energy deficiency, Nutritional history, Anthropometry
Cite this paper: Mavlyanova Zilola Farkhadovna, Cerebral Palsy as a Nutritional Problem, American Journal of Medicine and Medical Sciences, Vol. 10 No. 7, 2020, pp. 487-493. doi: 10.5923/j.ajmms.20201007.11.
1. Relevance
Cerebral palsy refers to a group of stable disorders in the development of motor skills and maintaining posture, which lead to motor defects caused by non-progressive damage and/or anomaly of the developing brain in the fetus or newborn [2,5,8]. According to the World Health Organization, cerebral palsy is the main cause of childhood neurological disability in the world; its frequency in the world is 3-4 cases per 1000 newborns [10]. Recently, the number of children with cerebral palsy has increased in the world by 14% [6], amounting to 17 million patients [1,4,5]. With an increase in the number of children diagnosed with cerebral palsy, the desire of medical specialists of various fields and parents to improve their quality of life accordingly increases [3].Patients with cerebral palsy constitute a risk group for nutritional deficiency. Problems with food intake and impaired assimilation of nutrients in cerebral palsy over the past 50 years have been repeatedly reported in the works of researchers from various countries [7]. In this connection, the problem of competent assessment of nutritional status and correction of its disorders in children with neurological diseases, in particular with cerebral palsy, has been given special attention in recent years. So, experts of the European Society of Pediatric Gastroenterologists, Hepatologists and Nutritionists (ESPGHAN) in 2017 published “Clinical Recommendations for the Assessment and Treatment of Gastrointestinal and Nutritional Complications in Children with Neurological Disorders” [8].Detecting more than half of children with cerebral palsy, nutritional status disorders are manifested in them in the form of varying degrees of weight deficiency, growth retardation, osteopenia (more than 70%), and obesity is diagnosed somewhat less frequently (10-15%) [5]. The main reason for the rapid progression of protein-energy deficiency in children with cerebral palsy, along with muscle spasticity or severe atony, hyperkinesis, problems with chewing and swallowing food, pseudobulbar or bulbar syndromes, gastroesophageal reflux disease, is reduced physical activity. Since a sick child does not have enough strength for physical activity due to nutritional insufficiency, physical rehabilitation/habilitation performed by him becomes ineffective [9,10], and helps to identify nutritional disorders in children with cerebral palsy and to conduct timely correction comprehensive assessment of nutritional status [5].According to the definition of a number of authors, nutritional status is defined as the state of the organism, its functions and structure, formed under the influence of qualitative and quantitative characteristics of actual nutrition, as well as acquired or genetically determined characteristics of metabolism, absorption, digestion and excretion of nutrients [7].Having recognized the fact that cerebral palsy cannot be cured, it must be accepted that a comprehensive approach and daily efforts are required for the rehabilitation/habilitation of a child with cerebral palsy. A significant role in this complex is played by balanced and rational nutrition. The quality of life and further socialization largely depend on what the child eats and how the feeding of the child with cerebral palsy occurs. In connection with the foregoing, the search for new, more effective methods of rehabilitation/habilitation of patients with cerebral palsy, providing the principles of comprehensiveness, taking into account the program of nutritional support, is justified, quite justified and relevant.Objective: To evaluate the nutritional status and study the features of nutritional history in various forms of cerebral palsy.
2. Material and Research Methods
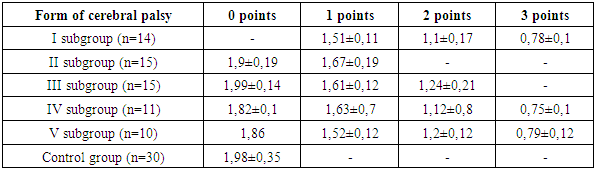
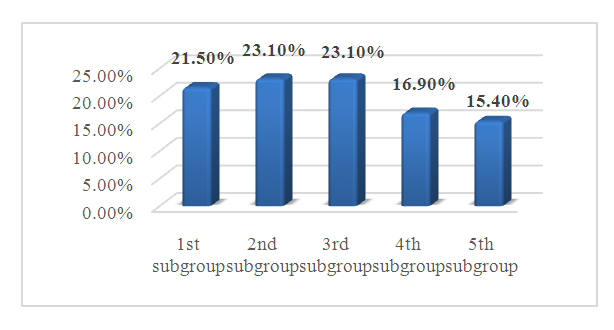
We examined 95 children aged 3 to 15 years, divided into two groups: the main group consisted of patients diagnosed with cerebral palsy (n = 65), the control group consisted of 30 healthy children who were observed in family clinics at the place of residence. The observation groups were comparable by age and gender. The age distribution of children in the observation groups is shown in Figure 1. In the age group of the main group, children aged 7–9 years prevailed - 30 people (46.1%); from 3 to 6 years old - 15 people (23.1%), 10-15 years old - 20 patients (30.8%). While in the control group the distribution of children by age was as follows: 3-6 years old - 20%, 7-9 years old - 40% and 10-15 years old - 40%.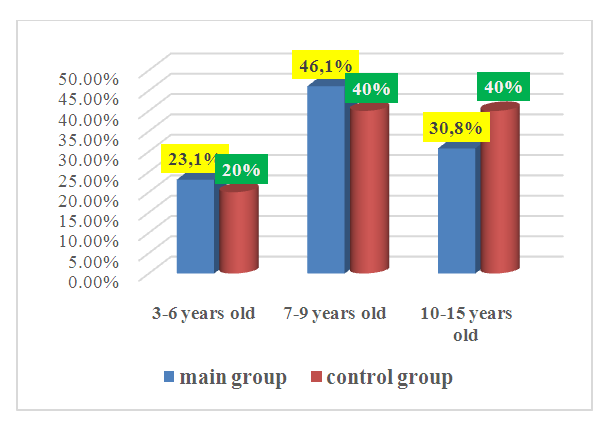 | Figure 1. Age structure of the examined children |
The examination plan for children in both groups included an assessment of nutritional status based on a study of the following indicators: weight and height of the child, shoulder circumference, measurement of the thickness of the skin-fat fold over the triceps, determination of the absolute number of blood lymphocytes and the content of albumin. Along with the assessment of the medical history, in all cases, a deep assessment and analysis of the nutritional history was carried out.Depending on the form of cerebral palsy (Figure 2), the children of the main group were divided into five subgroups on the basis of the International Classification of Cerebral Palsy, as the most used in the scientific literature [10]. 67.7% (44 observations) of all cases of cerebral palsy were spastic forms represented by 3 subgroups: tetraparesis (I subgroup) - 14 patients (21.5%); spastic diplegia (II subgroup) - 15 cases (23.1%); unilateral spastic hemiparetic form was diagnosed in 15 patients (III subgroup, 23.1%). Subgroup IV included patients with a dyskinetic form of the disease (11 cases, 16.9%). The Vth subgroup included 10 patients (15.4%) with varying degrees of severity of static and dynamic ataxia.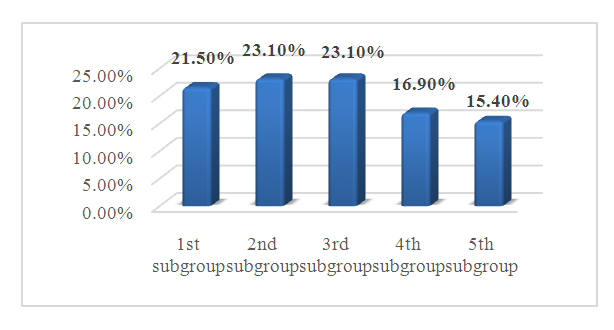 | Figure 2. Distribution of patients with cerebral palsy into subgroups depending on the form of the disease |
3. Results and Discussion
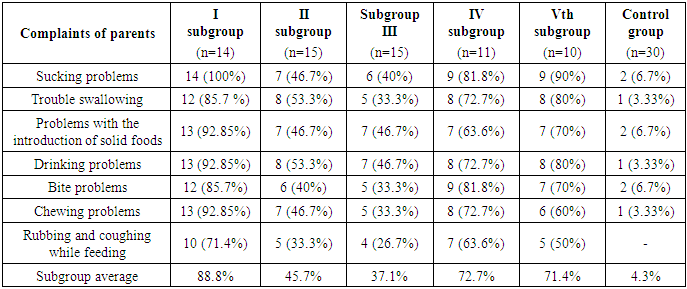
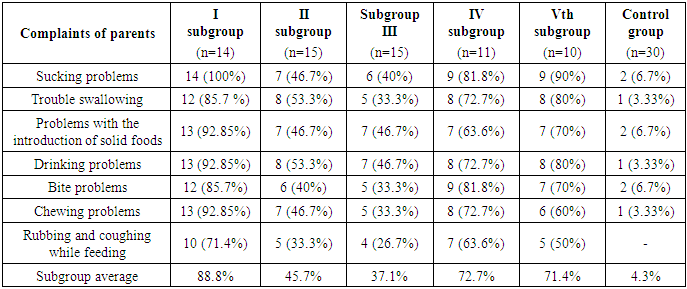
When analyzing the nutritional history of the examined patients with cerebral palsy, the following results are obtained, which are presented in table 1. When examining the complaints of parents about difficulties encountered during feeding of this category of children, it was found that from the moment of birth, almost all patients of the main group had problems with feeding.Table 1. The severity of oral motor dysfunction in the examined children
 |
| |
|
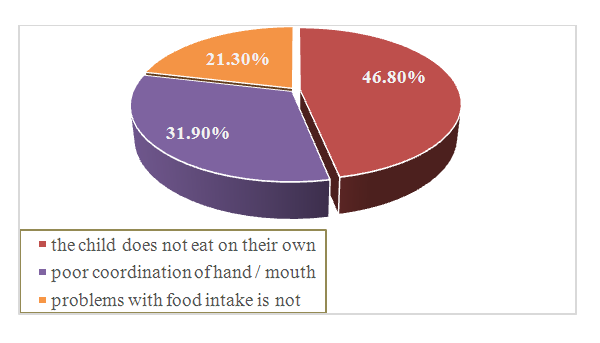
In general, in children with cerebral palsy, oral motor dysfunction of varying severity was observed in 63.1% of cases (n = 41), while in children of the control group on average in only 4.3% of cases. The most pronounced oral-motor dysfunction was observed in the group of patients with tetraparesis (on average in 88.8% of children), while the most frequent symptoms were problems with sucking (100% of the examined were noted already from the first days of life), later parents paid attention problems with the introduction of complementary foods, including solid foods, and chewing, as well as difficulties with drinking (up to 92.85%). Less pronounced than in the I -th subgroup, features oral-motor dysfunction observed in IY -th and Y-th subgroup of the examined - 72.7% and 71.4%, respectively.To the questions “Does the child have poor hand/mouth coordination leading to food loss” or “The child does not eat on his own”, the parents of the children of the main group (the analysis was conducted among children of the age category over 5 years old, n =47) in 22 (46.8%) cases they emphasized that the child does not eat on his own; 15 (31.9%) had poor hand/mouth coordination leading to food loss; and in 10 (21.3%) cases, the child did not have problems with food intake. Thus, problems with food intake occurred in 78.7% of patients in the main group (Figure 3). At the same time, 32 (68.1%) of the examined children had a violation of the natural regulation of nutrition due to communicative difficulties, since the patient could not clearly let know about his hunger, satiety, and also taste preferences.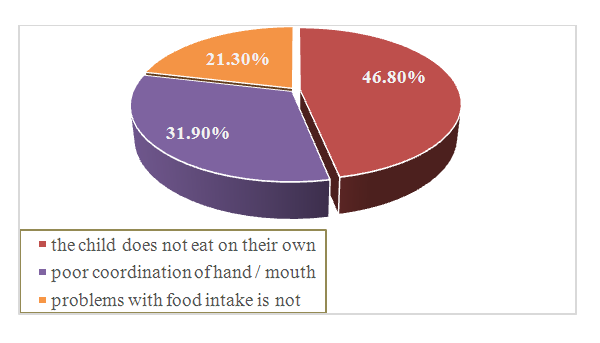 | Figure 3. Analysis of problems with food intake in patients with cerebral palsy |
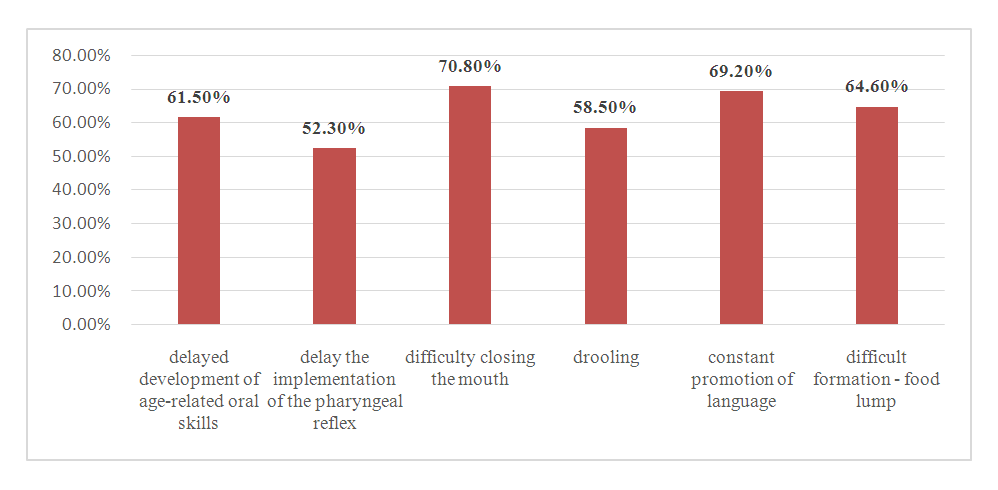
The results of the study of oral motor function (n = 65) in children with cerebral palsy indicated a delay in the development of age-related oral skills (40; 61.5%); delayed swallowing reflex, which is the most common cause of aspiration (34; 52.3%); difficulty closing the mouth (46; 70.8%); salivation (38; 58.5%); constant tongue extension causing food leakage (45; 69.2%); difficult formation of a food lump due to poor coordination of voluntary movements of the muscles of the tongue (42; 64.6%) (Figure 4).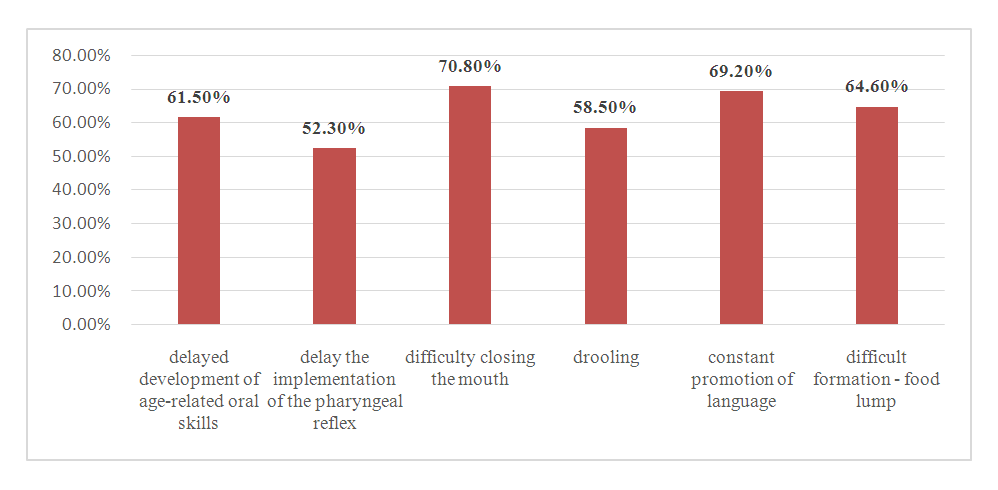 | Figure 4. Commonly identified signs of oral motor dysfunction in children with cerebral palsy |
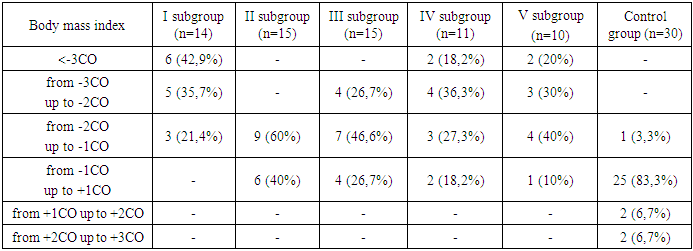
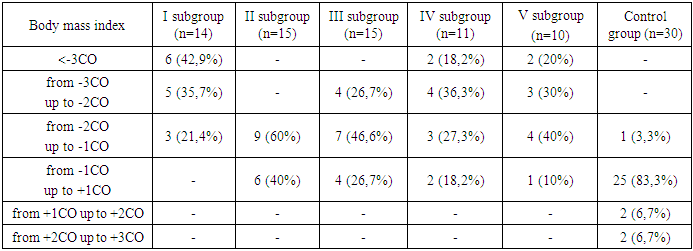
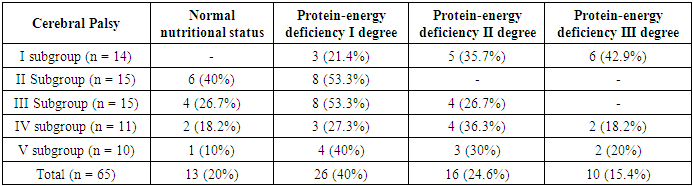
To assess the protein-energy status in both observation groups, the Bilbreri-Cohen method was used, which was proposed for the first time to evaluate protein-energy insufficiency in chronic renal failure (Bilbery G.L., 1989). The Bilbreri-Cohen method includes the determination of the following indicators:1) subjective global assessment,2) determination of body mass index,3) the thickness of the skin-fat fold above the triceps,4) the circumference of the muscles of the shoulder,5) serum albumin concentration,6) the absolute number of lymphocytes in the peripheral blood.In the absence of deviations from the age norm, the indicator from the given set was evaluated at 0 points; for mild, moderate and severe changes, the indicator was assigned from 1 to 3 points. The total score in six parameters of 0-1 points was interpreted as a normal state of nutrition, 2-6 points - a mild degree of protein-energy insufficiency, 7-12 points - a protein-energy insufficiency of moderate severity, 13-18 points - a severe degree of protein-energy insufficiency.The subjective global assessment included an analysis of 4 parameters: weight loss; anorexia; loss of subcutaneous fat; muscle loss. Each of their 4 parameters during the history taking and physical examination was evaluated from 0 to 7 points. The complex index of subjective global assessment was the result of the arithmetic addition of 4 numbers. Based on the subjective global assessment index, the degree of protein-energy malnutrition was assessed: absence of malnutrition (1-6) - 0 points; mild malnutrition (7-13) - 1 point; moderate reduction in nutrition (14-20) - 2 points; marked reduction in nutrition (21 and more) - 3 points.Along with this, an assessment was made of the body mass index by Quetelet (Yuryeva V.V., 2009): Body mass index = mass (kg)/[height (m)]2. The World Health Organization (WHO) recommends eating malnutrition in adolescents and adults if the body mass index is less than 18.5 kg/m2. The percentiles of the body mass index were calculated using the WHO Anthro (for children under 5 years old) and WHO Anthro plus (for children over 5 years old) programs and in accordance with the standards developed by the World Health Organization. Body mass index was estimated by the following standard deviations: -3CO, -2CO, -1CO, 0 (median), + 1CO, + 2CO, + 3CO. Normal indicators of physical development were detected only in 13 (20%) patients with cerebral palsy and in 25 (83.3%) children in the control group. The body mass index in these children relative to age corresponded to the norm and was in the range of -1CO and + 1CO. A severe degree of protein-energy malnutrition, when the child’s body mass index was in the area outside the -3CO curve, was diagnosed in 10 (15.4%) children with cerebral palsy in 3 subgroups: spastic tetraparesis - 6 patients (42.9%), dyskinetic and atactic form in 2 patients (18.2% and 20%, respectively). If the indicator of the child was in the region between -3CO and -2CO, then this child was regarded as very thin and this condition was regarded as a protein-energy insufficiency of moderate severity. This condition was observed in 16 (24.6%) patients with cerebral palsy in all groups, regardless of its form. In those cases when the body mass index was in the range between -2CO and -1CO, the child was considered thin, and his condition was assessed as a mild protein-energy insufficiency: this was noted in 40% of cases (26 observations) in children of the main group, and only one child in the control group. The body mass index, which was between + 1CO and + 2CO (the child’s diet is moderately elevated) and between + 2CO and + 3CO (the diet is elevated) was observed in 4 children in the control group, 6.7% each (table 2). Table 2. Comparative characteristics of body mass index of children of the main and control groups
 |
| |
|
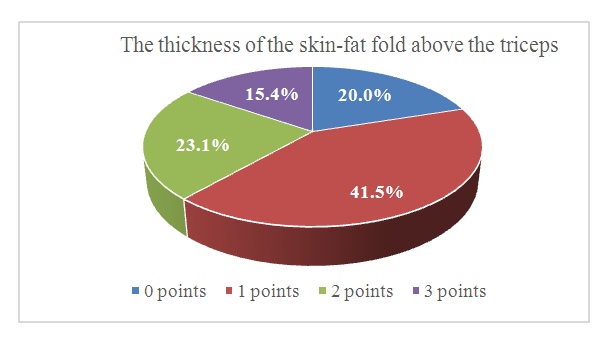
In general, values located below -2CO and to the -3CO curve, above + 2CO and to the + 3CO curve were considered low and high, requiring attention and appropriate decisions to prevent wasting and obesity. Indicators below the -3CO curve were "abnormal."After calculating the body mass index, a nutritional assessment was carried out: an absence of eating disorders (26th - 75th percentile) - 0 points; slight malnutrition (25th - 10th percentile) - 1 point, a moderate decrease in nutrition (9th - 5th percentile) - 2 points, a pronounced decrease in nutrition (below the 5th percentile) - 3 points. The differences in body mass index were 12.2 ± 0.22 kg/m2 in the main group and 19 ± 0.45 kg/m2 in the control group of children.The thickness of the skin-fat fold above the triceps, the circumference of the shoulder and the circumference of the muscles of the shoulder are correlated with high accuracy with the general peripheral reserves of protein and body fat reserves. The thickness of the skin-fat fold above the triceps (mm) was measured at the level of the middle third of the shoulder with an electronic caliper according to the standard method. The results were then evaluated by percentile tables: absence of malnutrition (26th - 75th percentile) - 0 points; mild malnutrition (25th - 10th percentile) - 1 point; moderate reduction in nutrition (9th - 5th percentile) - 2 points; marked reduction in nutrition (below 5 percentile) - 3 points. As a result of the interpretation of the obtained data, it was found that the absence of eating disorders was observed only in 20% (13 cases) with cerebral palsy and in 96.7% of cases in the control group. Mild malnutrition (25th - 10th percentile) was diagnosed in 41.5% of observations of the main group. Undoubtedly, the prevalence of moderate and severe malnutrition in children with cerebral palsy is interesting (23.1% and 15.4%, respectively) (Figure 5).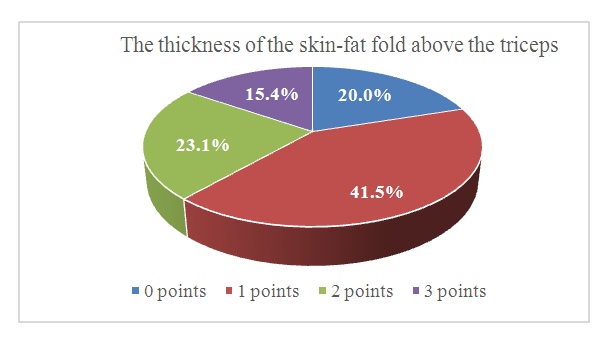 | Figure 5. Eating disorders in children with cerebral palsy according to the results of measuring the thickness of the skin-fat fold above the triceps |
Measurement of the circumference of the shoulder (mm) was carried out with a standard centimeter tape at the level of the middle third of the shoulder. The indicator of the circumference of the shoulder muscles (mm) was calculated by the formula: Shoulder muscle circumference = shoulder circumference - 0.314×thickness of the skin-fat fold over the triceps. Then the indicator of the circumference of the shoulder muscles was also interpreted according to percentile tables as follows: absence of malnutrition (26th - 75th percentile) - 0 points; mild malnutrition (25th - 10th percentile) - 1 point; moderate reduction in nutrition (9th - 5th percentile) - 2 points; marked reduction in nutrition (below the 5th percentile) - 3 points (figure 6). The average score for the studied parameter was 0 points in the control group and 1.4 ± 0.21 points in the group of children with cerebral palsy (p<0.05). The most pronounced malnutrition was noted in the group of children with spastic tetraparesis - 2.21 ± 0.11 points, the prevalence of a mild degree of violation in the group of patients with spastic diplegia - 0.6 ± 0.25 points and unilateral spastic hemiparesis - 1.01 ± 0.12 points. | Figure 6. The diagram of the circumference of the shoulder muscles in children of the main and control groups |
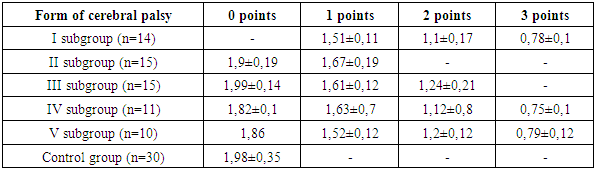
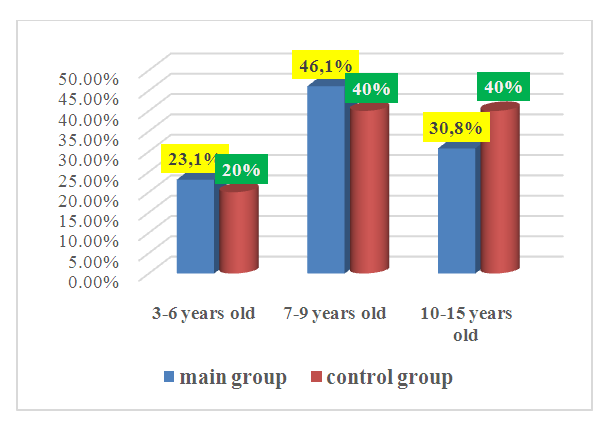
The simplest method for assessing the state of the immune system, which directly and directly depends on protein-energy capabilities, and allowing a comprehensive assessment of trophic disorders, is to calculate the absolute number of blood lymphocytes. The calculation of the absolute number of lymphocytes was carried out according to the formula Absolute number of lymphocytes = lymphocytes (%)×number of leukocytes (109/l)/100. The results were interpreted as follows: no malnutrition (1.8×109/l) - 0 points; mild malnutrition (1.79-1.5×109/l) - 1 point; moderate reduction in nutrition (1.49-0.9×109/l) - 2 points; a marked reduction in nutrition (below 0.9×109/l) - 3 points.When analyzing this parameter for assessing protein-energy deficiency, the following results were obtained, shown in table 3. The absolute number of lymphocytes in the blood in children of the control group was 1.98 ± 0.35 × 109/l, which is significantly higher than in children of the main group with cerebral palsy - 1.21 ± 0.16 × 109/l (p<0.05).Table 3. Evaluation of protein-energy capabilities depending on the level of the absolute number of lymphocytes (× 109/l)
 |
| |
|
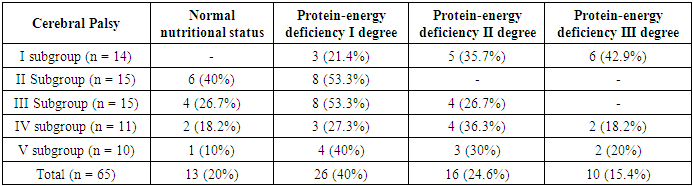
Serum albumin, being the main marker of protein status, was evaluated as follows: mild malnutrition (35-30 g/l) -1 point; moderate reduction in nutrition (30-25 g/l) - 2 points; marked reduction in nutrition (below 25 g/l) -3 points. If the average serum albumin content in children of the control group was 38 ± 0.78 g / l, then in patients of the main group with cerebral palsy, this indicator was significantly lower and amounted to 28 ± 0.23 g / l (p<0, 05).As a result of the systematization of indicators reflecting the main positions of nutritional status: subjective data on the state of nutrition (nutritional history, subjective global assessment), anthropometric indicators (body mass index, thickness of the skin-fat fold over the triceps, circumference of the muscles of the shoulder), the assessment of blood albumin, the presence of immunodeficiency (the absolute number of lymphocytes) the optimal option for assessing the degree of protein-energy deficiency in children with cerebral palsy has been formed.And since the severity of oral motor dysfunction correlates with the severity of the disease and the delayed motor development during the study, it was found that children with severe motor impairment are characterized by severe forms of protein-energy deficiency. In general, 80% of the examined children with cerebral palsy had some degree of protein-energy deficiency resulting from nutrition problems (table 4).Table 4. The relationship of the degree of protein-energy deficiency with the severity of cerebral palsy/
 |
| |
|
4. Findings
1. To determine the degree of nutritional deficiency in children with cerebral palsy, a comprehensive study should be carried out, including the determination of not only clinical and neurological parameters, but also anthropometric, laboratory parameters using a total assessment of the degree of protein-energy insufficiency.2. Evaluation of anthropometric indicators in children with cerebral palsy is an important tool for diagnosing malnutrition.3. The causes of nutritional deficiency are due to a number of factors directly related to impaired nervous regulation, the main causes of which are damage to the brain centers, as well as impaired swallowing and chewing functions in this category of patients. Along with this, there is also a lack of active movements, which, in turn, leads to a discrepancy in eating habits.4. In case of cerebral palsy, careful monitoring of nutritional status, development of a diet with the appointment of nutritional support according to indications and its mandatory correction in the dynamics of observation, taking into account the age, nature of the underlying disease, the presence of concomitant pathology, and the volume and intensity of rehabilitation measures, are necessary.
References
| [1] | Araujo L.A., Silva L.R. Anthropometric assessment of patients with cerebral palsy, which curves, are more appropriate // Journal Pediatr (Rio J), 2013; 89(3). P. 307-314. |
| [2] | Arrowsmith F.E. Nutritional assessment of children with quadriplegic cerebral palsy // A thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy Discipline of Paediatrics & Child Health Faculty of Medicine // The University of Sydney, June 2006; 314 P. |
| [3] | Gmelig Meyling C. et al. Effects of postural management on hip migration in children with cerebral palsy: A systematic review //Pediatric Physical Therapy. – 2018. – Т. 30. – №. 2. – С. 82-91. |
| [4] | Jihua Zhang, Caiyun Ma, Guanghui Liu, Qing Shang, Jingjie Li, Chao Xu. The Accommodation Roles of Arginine Palsy Infants with Muscle Hypotonia // Life Science Journal, 2014; 11(6). Р. 698-703. |
| [5] | Erasmus C.E., van Hulst K., Rotteveel J.J., Willemsen M.A., Jongerius P.H. Clinical practice: swallowing problems in cerebral palsy // Eur J. Pediatr, 2012 Marсh; 171(3). P. 409-14. doi: 10.1007/s00431-011-y. |
| [6] | Robinson J. D., Prochaska J. D., Yngve D. A. Pre-surgery evaluations by telephone decrease travel and cost for families of children with cerebral palsy //SAGE open medicine. – 2017. – Т. 5. – С. 2050312117720046. |
| [7] | Romano C., van Wynckel M., Hulst J., Broekaert I., Bronsky J., Dall’Oglio L. et al. European Society for Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for the Evaluation and Treatment of Gastrointestinal and Nutritional Complications in Children With Neurological Impairment. J Pediatr Gastroenterol Nutr 2017; 65: 242-264. DOI: 10.1097/MPG.0000000000001646. |
| [8] | Shore B. J. et al. Measuring the Reliability and Construct Validity of the Pediatric Evaluation of Disability Inventory–Computer Adaptive Test (PEDI-CAT) in Children With Cerebral Palsy //Archives of physical medicine and rehabilitation. – 2019. – Т. 100. – №. 1. – С. 45-51. |
| [9] | Whitney D. G. et al. Bone marrow fat physiology in relation to skeletal metabolism and cardiometabolic disease risk in children with cerebral palsy //American journal of physical medicine & rehabilitation. – 2018. – Т. 97. – №. 12. – С. 911. |
| [10] | Willerslev‐Olsen M. et al. Impaired muscle growth precedes development of increased stiffness of the triceps surae musculotendinous unit in children with cerebral palsy //Developmental Medicine & Child Neurology. – 2018. – Т. 60. – №. 7. – С. 672-679. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML