Khamdamov Bakhtiyor Zarifovich
Bukhara State Medical Institute Named after Abu Ali Ibn Sino, Uzbekistan
Correspondence to: Khamdamov Bakhtiyor Zarifovich, Bukhara State Medical Institute Named after Abu Ali Ibn Sino, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Comparative characteristics of the parameters of the immune system of T-and B-lymphocytes showed the presence of an imbalance and tension in the immune system of patients with diabetic foot syndrome with signs of critical lower limb ischemia, which indicates the development of secondary immunodeficiency and the occurrence of gross immunological rearrangements reflected in the significant activity of the Pro-inflammatory cytokine IL-17A, which is of great value as a test for early diagnosis of complications during the wound process and the inevitable probability of organ dysfunction.
Keywords:
Immunocytokine status, Diabetic foot syndrome, Critical ischemia, Diabetes mellitus
Cite this paper: Khamdamov Bakhtiyor Zarifovich, Indicators of Immunocytokine Status in Purulent-Necrotic Lesions of the Lower Extremities in Patients with Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 10 No. 7, 2020, pp. 473-478. doi: 10.5923/j.ajmms.20201007.08.
1. Introduction
Treatment of patients with purulent-necrotic forms of diabetic foot syndrome (DFS) is one of the most difficult tasks for specialists dealing with this problem, which is confirmed by the low effectiveness of most methods of conservative and surgical treatment of this pathology [10,12,13]. Unfortunately, in practice we have to face the fact that the main causes of purulent-necrotic complications are severe microcirculatory disorders of the limb and, as a result, the development of critical lower limb ischemia (CLLI) [6,14].The steady progression of atherosclerotic artery damage in diabetes mellitus leads to severe critical ischemia in 25-30% of elderly and senile patients [9,15]. The resulting pathogenetic picture in DFS against the background of CLLI and increasing metabolic imbalance inevitably leads to immunological shifts in the form of a secondary immunodeficiency condition, in which even a minor purulent-necrotic process on the foot can acquire the character of a rapidly progressive infectious focus, often being the main reasons for the use of radical surgical methods up to performing forced high amputations of the lower extremities to save the patient's life [1,2,3,4,5,7,8,11,16].All of the above indicates the feasibility of conducting research aimed at studying and evaluating the immune system in patients with DFS with critical lower limb ischemia, in order to predict the development of early complications both during the wound process and in the development of organ dysfunction.
2. Purpose of Research
Comparative assessment of the immune system indicators of patients with diabetic foot syndrome signs of critical lower limb ischemia.
3. Materials and Methods
The results of studies of two groups of patients are analyzed. The first control group consisted of 30 healthy persons, second 412 patients with diabetic foot syndrome with critical ischemia of lower extremities, treated in the Department of purulent surgery of Bukhara regional diversified medical center from 2009 to 2019. Of these, 283 (68.7%) were male and 129 (31.3%) were female. The age of the patients varied from 38 to 85 years. The gender and age composition of the control group was identical with the patients of the main group.For immunological parameters, blood was collected from the ulnar vein in a centrifuge tube treated with 5.0 ml of heparin. The count of leukocytes and lymphocytes was carried out in the camera Goryaeva with paint Zadorozhniy S. I. and Dozmorov I. M. (1987). Mononuclear cells from peripheral blood were obtained by isolation on a density gradient of ficoll-verografin with a density of 1.077 g / l according to Boyum (1968).The assessment of the state of the immune system of the body of patients and healthy was carried out by the expression of CD - differentiation and activation antigens. The following markers of immune competent cells were determined: CD3+ -, CD4+ -, CD8+ -, CD16+ -, CD20+ -, CD23+ -, CD38+ -, and CD25+ -, CD95+ - lymphocytes. CD receptor expression was performed in the rosette formation reaction using monoclonal antibodies of the LT series produced by Sorbent LLC (RF) using the method of Garib F. Y. et al. (1995).Determination of serum concentrations of the examined immune globulins of the main three classes M, A and G was performed by radial immune diffusion according to Mancini (1963). Interleukins (cytokines) were determined in the blood serum of the subjects by solid-phase enzyme immunoassay (ELISA). To implement this variant, two monoclonal antibodies with different etiotropic specificity to interleukins - 10 and 17A were used. One of them is immobilized on the inner surface of the tablet wells, the second is conjugated with peroxidase. At the first stage of the analysis, contained in the calibration and test samples, binding was performed with antibodies immobilized on the inner surface of the wells. At the second stage of analysis, the immobilized interleukin interacted with the conjugate of the second antibodies - peroxidase. The amount of conjugate bound was directly proportional to the amount of interleukin in the test sample. During incubation with the substrate mixture, the solution was colored in the wells. The degree of color was directly proportional to the number of bound labeled antibodies. After measuring the optical density of the solution in the wells, the concentration of interleukin in the determined samples was calculated based on the calibration curve. The test kit "Cytokine" (Saint Petersburg, Russia) was used.The research results were processed using the generally accepted method of variation statistics. A package of programs for biomedical research was used. The principles of evidence-based medicine were used in the organization and conduct of research.
4. Results of the Study
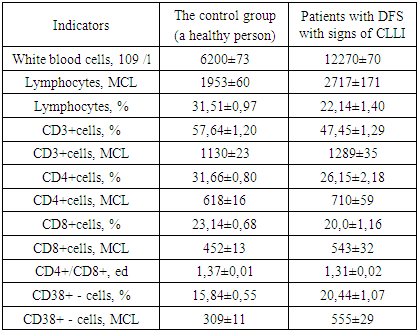
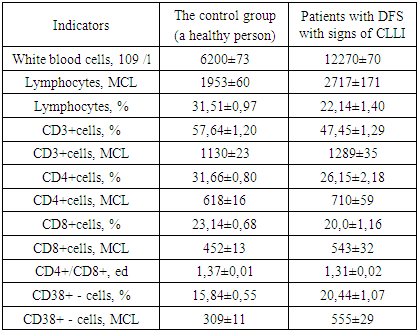
The results showed that if a 2.0-fold increase in the number of white blood cells in patients with diabetic foot syndrome with signs of critical lower limb ischemia (12270±70x109/l) compared to healthy individuals (6200±73x109/l) was a manifestation of the inflammatory process in the body, then a decrease in the relative and absolute number of lymphocytes (22.14±1.40% and 2717±171 MCL, respectively) indicated a decrease in the body resistance of these patients (table 1).Table 1. Comparative indicators of cellular immunity of patients diabetic foot syndrome signs of critical lower limb ischemia and healthy individuals, М±m
 |
| |
|
The study of the relative and absolute number of lymphocytes that carry CD3+ differentiating markers (T-lymphocytes) on their surface showed that they changed in different directions in relation to the control data. If the relative number of CD3+cells is 1.2 times significantly reduced in relation to healthy data (respectively 57.64± 1.20% vs. 47.45±1.29%, P<0.05 ), then the absolute number of these cells were significantly increased in relation to the norm by 1.1 times (respectively 1289±35 µl vs. 1130±23 µl). That is, patients with diabetic foot syndrome with signs of critical lower limb ischemia were found to have T-immunodeficiency.Next, we studied the main subpopulations of T-lymphocytes - T-helpers/inducers (CD4+cells) and T-suppressors/cytotoxic lymphocytes (CD8+cells). The trend and direction of changes in the relative and absolute number of these subpopulations were the same as in CD3+lymphocytes, but with different intensity. The deficit of the relative number of CD4+cells in patients was 1.2-fold in relation to this parameter in healthy individuals - respectively 26.15±2.18% vs. 31.66±0.80% (P<0.05), but the deficit of CD8+cells was little noticeable-the decrease was 1.1 times (respectively 20.0±1.16% vs. 23.14±0.68%, P<0.05). In both cases, the absolute values, as in CD3+lymphocytes, were significantly higher than the control values (P<0.05). Against this background, the immunoregulatory index (CD4+ / CD8+) was also significantly reduced in patients in relation to the norm - 1.31±0.02 units, respectively, versus 1.37±0.01 units. (P<0.05).A comparative study of the relative and absolute number of T-lymphocytes (CD3+cells) and their regulatory subpopulations - t-helpers/inducers (CD4+cells) and T-suppressors/cytotoxic lymphocytes (CD8+cells) showed that in patients with DFS signs of CLLI, the parameters changed with the same tendency and different directions. The absolute numbers of all cells in patients were significantly increased, but the relative values were significantly reduced in relation to the data of healthy individuals.Given the fact that in clinical immunology, the activity of the immune system is evaluated by the functional States of immune competent cells examined, the relative number of cells indicates the true state of the immune status. Based on this, we found that the studied DFS patients show signs of CLLI T - immunodeficiency.It is known that the CD38 + - marker is found on the surface of many immune cells and is involved in the processes of cell death, apoptosis, and others. CD38+ - participates in the regulation of metabolism and in the pathogenesis of aging and inflammation. With this in mind, we considered it appropriate to identify lymphocytes that carry the CD38+-marker on their surface.The obtained results showed that the relative number of CD38+lymphocytes, in contrast to T-lymphocytes and their subpopulations, increased in relation to normal values by 1.3 times - respectively 20.44±1.07% vs. 15.84±0.55% (P<0.05). Identical indicators were obtained in the analysis of absolute values of these lymphocytes, where the difference between the data of patients and healthy individuals was 1.8-fold in favor of patients with diabetic foot syndrome with CLLI-respectively 555±29 MCL versus 309±11 MCL (P<0.001).Thus, it was found that the relative and absolute number of CD38 + lymphocytes in DFS patients with CLLI was significantly increased by 1.3 and 1.8 times in relation to the standard values. This fact indicates that, in contrast to T-lymphocytes and their subpopulations, the functional activity of CD38+lymphocytes increases, as evidenced by an increase in their number. If we consider that CD38 + lymphocytes are involved in the aging process and inflammation associated with the patients we studied, then to study the immune status of these patients, it is recommended to include this parameter (CD38+cells) as an additional, highly informative criterion of the state of the immune status in older patients (elderly and senile).At the next stage of research, we studied the parameters of the b-system of lymphocytes, the results of which are shown in table 2.Table 2. Comparative indicators of the b-system of lymphocytes and humoral immunity in patients with diabetic foot syndrome with signs of critical lower limb ischemia and healthy individuals, М±m
 |
| |
|
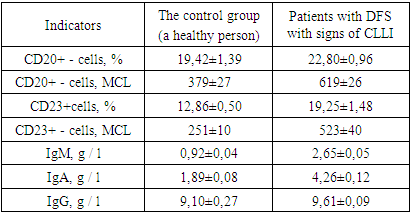
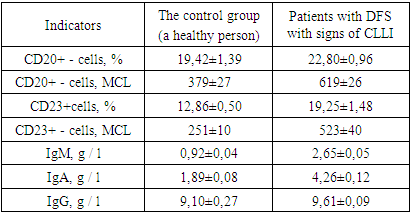
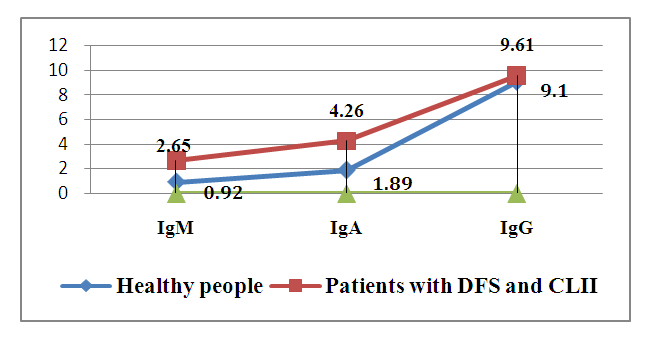
The results obtained show that, in contrast To the t-system of lymphocytes, the relative and absolute number of B-lymphocytes (CD20+cells) in patients was significantly higher than in healthy individuals, respectively, by an average of 1.2 and 1.6 times (P<0.05) - 22.80±0.96% and 619±26 µl in patients, compared to 19.42±1.39% and 379±27 µl in healthy individuals.Almost the same results, but with greater intensity, were observed for the content of cd23+lymphocytes in the peripheral blood of patients, the relative and absolute content of WHICH were significantly higher than the same parameters of healthy individuals (P<0.001) - respectively, on average 19.25±1.48% vs. 12.86±0.50% (a difference of 1.5 times, P<0.001) and on average 523±40 µl vs. 251±10 µl (a difference of 2.1 times, P<0.001). Indicators of humoral immunity (immune globulins of classes M, A and G-IDM, IDA and IgG) had the same tendency and direction of changes in the examined patients as CD20+ and CD23+cells. The concentration of all studied serum immune globulins in patients was increased in relation to the control data, only with different intensity (figure.1).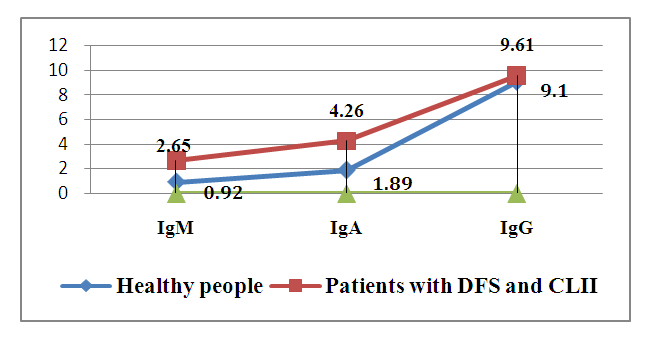 | Figure 1. Comparative parameters of the content of the main classes of immune globulins in the blood serum of patients with DFS with signs of CLLI and healthy individuals, g / l |
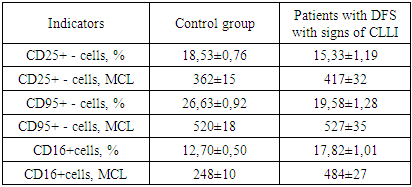
If the indicators of IDM in patients were increased in relation to the data of healthy individuals by an average of 2.9 times (respectively 2.65±0.05 g / l vs. 0.92±0.04 g/l, P<0.001), then almost the same trend was observed in the blood serum of patients and healthy IDA, the difference was 2.3 times - respectively 4.26±0.12 g/l vs. 1.89±0.08 g / l (P<0.001). The intensity of differences between the content of IgG in the peripheral blood of the examined patients and healthy individuals was relatively low - on average, 1.1 times increased in patients compared to healthy ones-respectively 9.61±0.09 g / l versus 9.10±0.27 g / l (P<0.05).Thus, the study and evaluation of the parameters of the b-system of lymphocytes and humoral immunity in patients with DFS signs of CLLI in comparison with the data of healthy individuals showed that the relative and absolute content of CD20+ and CD23+cells were significantly increased in patients on average by 1.2 - 2.1 times in relation to the control. The same trend and direction of changes were observed in the comparative analysis of the content of IDM, IDA and IgG in the blood serum of the examined patients. The largest increase was in IDM, where the difference from healthy patients was 2.9 times (P<0.001), and the smallest increase in IgG, where the difference from control data was 1.1 times (P<0.05).Comparative characteristics of the parameters of the immune system T - and B-system of lymphocytes showed that in the examined patients with DFS signs of CLLI, these indicators changed in the opposite direction - a decrease in the content of T-lymphocytes and an increase in the concentration of B-lymphocytes. This indicates the following patterns identified by us: first, the studied patients have an imbalance of t - and B-lymphocyte indices; second, this imbalance indicates the presence of tension in the immune system of patients; third, a decrease in one component of the body's immune system causes an increase in another component of the immune system, which complement each other's functions.At the next stage of the research, the expression of certain activation markers on the surface of peripheral blood lymphocytes of the studied patients with DFS signs of CLLI and healthy individuals was analyzed in comparison. In the studies, the expression of a marker of early activation of lymphocytes, CD25+cells, was evaluated, and the readiness of cells for apoptosis was assessed based on the determination of the content of CD95+cells expression (table 3).Table 3. Comparative parameters of lymphocytes with a marker of activation and apoptosis, natural killers in patients with DFS signs of CLLI and healthy individuals, М±m
 |
| |
|
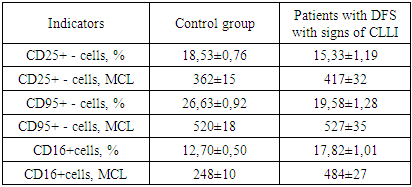
The results showed that the markers of CD25+-cell lymphocytes were significantly reduced in the examined patients compared with the data of healthy individuals, respectively, on average 15.33±1.19% versus 18.53±0.76% (P<0.05). The resulting 1.2-fold difference indicates an increase in the content of lymphocytes with markers of early activation (CD25+cells), the same picture was observed when evaluating CD95+cells responsible for the readiness of cells for apoptosis-respectively, on average 19.58±1.28% versus 26.63±0.92% (a difference of 1.4 times, p<0.05).It is known that natural killer cells (NK cells) contain the CD16+ marker on their surface and are responsible for detecting and destroying tumor cells. Activation of these CD16+cells indicated the presence of tension in the immune system.Studies have found that, as well as lymphocytes with markers of activation of lymphocytes with readiness for apoptosis of cells (CD25+ and CD95+cells) and CD16+lymphocytes were characterized by increased functional activity, that is, their content was significantly increased in relation to normal values - respectively, on average 17.82±1.01% vs. 12.70±0.50% (a difference of 1.4 times, P<0.05).Thus, the study of lymphocytes with markers of early activation (CD25+cells) and cell readiness for apoptosis (CD95+cells), as well as natural killer cells (CD16+cells) in patients with DFS signs of CLLI in comparison with healthy people showed that the content of all the studied cells was significantly increased. This fact indicates that all lymphocytes are activated and the immune system is strained.Us for early diagnosis, monitoring, and prediction of disease outcome has been studied the content of some Pro - and anti-inflammatory cytokines to evaluate the immune status in patients with DFS signs of CLLI. At the same time, two cytokines were identified – the Pro-inflammatory cytokine IL-17A and the anti-inflammatory cytokine IL-10, the results of which are shown in table 4.Table 4. Comparative content of Pro - and anti-inflammatory cytokines in patients with diabetic foot syndrome with signs of critical lower limb ischemia and healthy individuals, М±m
 |
| |
|
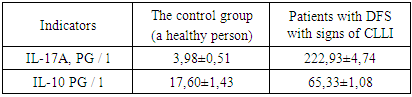
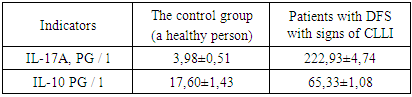
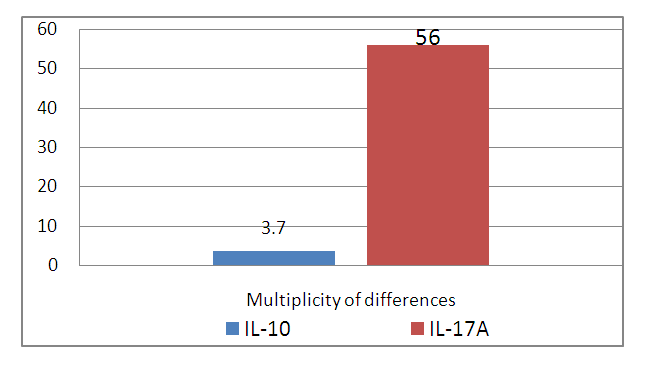
Studies have found that the content of IL-17A in the blood serum of healthy individuals averaged 3.98±0.51 PG/l, and in patients with DFS with signs of CLLI, this parameter increased 56.0 times and averaged 222.93±4.74 PG/l (P<0.001).The serum content of Il-10 anti-inflammatory cytokine in the examined patients and healthy patients tended to increase by 3.7 times-respectively, on average 65.33±1.08 PG/l 17.60±1.43 PG / l (P<0.001).It can be seen that both cytokines (IL-17A and IL-10) were significantly increased in patients in relation to the standard values. This fact confirms that the surveyed patients, the inflammatory process has been developed strongly associated with a sufficient number of pathogens in the infected focus and the presence of signs of critical ischemia and development of patients with systemic inflammatory response syndrome (Sirs), which in our opinion, aggravates the pathological process, the inflammatory process, in turn, lead to worsening of the signs of critical ischemia. Thus, there is a vicious circle with the mutual aggravation of inflammation and critical ischemia.At the same time, attention is drawn to the high multiplicity of the difference between the compared groups of sick and healthy individuals (figure.2). 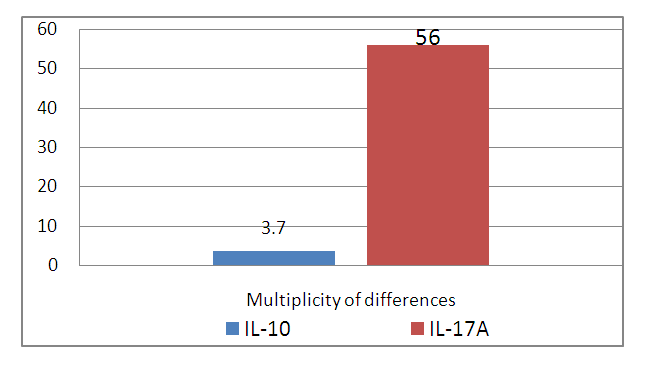 | Figure 2. Multiplicity of differences between IL-17A and IL-10 between patients with DFS signs of CLLI and healthy individuals |
Thus, a comparative analysis of the cytokine status in patients with DFS signs of CLLI and healthy individuals showed that both studied cytokines (IL-17A and IL-10) were significantly increased in patients in relation to control data, and the trend and direction of changes were the same in the studied indicators. The difference was significant in the intensity of changes, where the Pro-inflammatory cytokine IL-17A was increased by an average of 56.0 times (cytokine storm), and the anti-inflammatory cytokine IL-10 by an average of 3.7 times compared to normal values. From the above, it follows that the activity of Pro-inflammatory cytokine in patients is an order of magnitude greater than anti-inflammatory cytokine. Due to the dramatic changes in the blood serum content of patients, it can be suggested that the determination of IL-17A is of great diagnostic value as an additional test for early diagnosis of complications in patients with DFS with signs of CLLI.
5. Conclusions
1. the Study of the relative and absolute number of CD3 + cells and their regulatory subpopulations of CD4+ and CD8+cells showed that in patients with diabetic foot syndrome with critical lower limb ischemia, these parameters changed with the same tendency and different directions, while the absolute number of cells was increased, and the relative significantly reduced relative to the control.2. the Relative and absolute number of CD38+lymphocytes in patients with diabetic foot syndrome with critical lower limb ischemia were significantly increased by 1.3 and 1.8 times in relation to normal values, which indicates the functional activity of CD38+lymphocytes.3. it was Found that the relative and absolute content of CD20+ and CD23+ cells significantly increased in patients by an average of 1.2-2.1 times in relation to the control.4. The trend and direction of changes to increase is observed when analyzing the content of IDM, IDA and IgG in blood serum, while the greatest increase is subject to IDM, where their difference from healthy ones is 2.9 times.5. Comparative characteristics of the parameters of the immune system T - and B-system of lymphocytes showed that in the examined patients with diabetic foot syndrome with critical lower limb ischemia, these indicators changed in opposite directions - a decrease in the content of T-lymphocytes and an increase in the concentration of B-lymphocytes.6. in the course of research, the following patterns were identified: patients have an imbalance, indicators of T-and B-lymphocytes; which indicates the presence of tension in the immune system of patients, while a decrease in one component of the body's immune system causes an increase in another component of the immune system, which complement each other's functions;7. the Study of lymphocytes with markers of early activation (CD25+cells) and cell readiness for apoptosis (CD95+cells), as well as natural killer cells (CD16+cells) in patients with diabetic foot syndrome with critical lower limb ischemia in comparison with healthy people showed that the content of all the studied cells was significantly increased in patients. This fact indicates the development of a systemic inflammatory reaction syndrome.8. Comparative analysis of cytokine status in patients with diabetic foot syndrome with critical lower limb ischemia and healthy individuals showed that IL-17A and IL-10 were significantly increased in relation to control data.9. the Trend and direction of changes in the content of IL-17A and IL-10 were the same for the studied indicators. The difference was significant for intensity change, where the proinflammatory cytokine IL-17A were increased on average at 56.0 times, and anti-inflammatory cytokine IL-10 in average 3.7 times compared to normal values, which meant that the activity of Pro-inflammatory cytokine in patients more than anti-inflammatory cytokine.10. Determination of IL-17A is of great diagnostic value and is recommended as an additional test for early diagnosis of complications in the form of systemic inflammatory reaction syndrome and organ dysfunction in patients with diabetic foot syndrome with critical limb ischemia.
References
| [1] | Akhmedov R. M., Khamdamov B. Z., Khamdamov I. B. Assessment of methods of amputation at the level of the lower leg in severe forms of diabetic foot syndrome //Problems of biology and medicine. - Samarkand, 2019. №4 (113). –Pp. 29-32. |
| [2] | Vdovich O. V., Potrokhova E. A. Prospects for diagnostic research of interleukin 17 in rheumatoid arthritis //Questions of diagnostics in Pediatrics-2013. - №4. - P. 24-27. |
| [3] | Garib F. Y. Mechanisms of interactions of pathogenic bacteria with innate immune responses of the host //Educational and methodological guide. - Moscow, 2012. - 44C. |
| [4] | Kosaev D. V., Akhmedova L. M., Gadzhieva G. K. Monitoring of immunological indicators in patients with critical lower limb ischemia in complex treatment with laser therapy / / laser medicine.-2010. - vol. 14, no. 1. - P. 4-7 |
| [5] | Kulikova A. N. the Role of inflammation in atherogenesis in diabetes mellitus//Cytokines and inflammation.-2007. - Vol. 6, No. 3. - P. 14-19. |
| [6] | Lazarenko V. A., Nikolaev S. B., Bystrova N. A., Konoplya A. I. Correction of immunometabolic disorders in patients with critical lower limb ischemia of atherosclerotic Genesis / / Kursk scientific and practical Bulletin "Man and his health", 2010, no. 2. - Pp. 78-83. |
| [7] | Nuraliev N. A., Rakhmonova R. S., Ismailov B. A. Immunology. Volume of Lectures. - Toshkent 2010. -58 b. |
| [8] | Shilova L. N., Panshina N. N., Chernov A. S., Trubenko Yu. a., Khortieva S. S., Morozova T. A., Panshin N. G. Immunopathological significance of interleukin -17 in psoriatic arthritis //Modern problems of science and obrazovaniya. -2015. - # 6. |
| [9] | Proshin A.V. State of the immune status and dynamics of the wound process in patients with complicated forms of diabetic foot syndrome//Bulletin Of The Novgorod State University, -2012. - No. 67. - P. 74-77. |
| [10] | Alhaik, Sari, Huda A. Anshasi, Ja’far Alkhawaldeh, Kim Lam Soh, and Aseel Mazen Naji. 2019. “An Assessment of Self-Care Knowledge among Patients with Diabetes Mellitus.” Diabetes and Metabolic Syndrome: Clinical Research and Reviews. https://doi.org/10.1016/j.dsx.2018.10.010. |
| [11] | Choe, Sung Sik, Jin Young Huh, In Jae Hwang, Jong In Kim, and Jae Bum Kim. 2016. “Adipose Tissue Remodeling: Its Role in Energy Metabolism and Metabolic Disorders.” Frontiers in Endocrinology. https://doi.org/10.3389/fendo.2016.00030. |
| [12] | Hlinkova, Edita, Jana Nemcova, and Katarína Ziakova. 2017. “Educational Assessment of Diabetics Requiring Vascular Surgery.” Central European Journal of Nursing and Midwifery. https://doi.org/10.15452/CEJNM.2017.08.0023. |
| [13] | Kress, S, H Anderten, A Borck, G Freckmann, L Heinemann, U Holzmueller, B Kulzer, et al. 2017. “Preulcerous Risk Situation in Diabetic Foot Syndrome - Proposal for a Simple Ulcer Prevention Scoring System.” DIABETES STOFFWECHSEL UND HERZ. |
| [14] | Khamdamov B.Z., N.A. Nuraliev. Pathogenetic approach in complex treatment of diabetic foot syndrome with critical lower limb ischemia. //American Journal of Medicine and Medical Sciences, 2020 10 (1) 17-24. DOI: 10.5923/j.20201001.05. |
| [15] | Świątoniowska, Natalia, Mariusz Chabowski, and Beata Jankowska-Polańska. 2020. “Quality of Foot Care Among Patients With Diabetes: A Study Using a Polish Version of the Diabetes Foot Disease and Foot Care Questionnaire.” Journal of Foot and Ankle Surgery. https://doi.org/10.1053/j.jfas.2019.07.020. |
| [16] | Toliver-Kinsky, Tracy, Makiko Kobayashi, Fujio Suzuki, and Edward R. Sherwood. 2018. “The Systemic Inflammatory Response Syndrome.” In Total Burn Care: Fifth Edition. https://doi.org/10.1016/B978-0-323-47661-4.00019. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML