Akilov Kh. A. , Primov F. Sh. , Khidoyatov Dj. S.
Сenter for the development of professional qualifications of health workers, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Objective: to compare laparoscopic and open appendectomy in acute complicated appendicitis in pediatric population. Material and methods. The study included 250 children with acute complicated appendicitis, operated from December 2012 to August 2019 (164 laparoscopic, 60 open and 26 converting appendectomies). Most patients were 13-17 years old (101 cases, 40.4%). Perforated appendicitis was most often detected (47.6% of cases, 119 out of 250). In prevalence, in most cases there was spilled appendicular peritonitis (40.5%). Results. A significantly low incidence of early complications was revealed in the group of laparoscopic appendectomies (15.2% versus 56.7%; p<0.001), both specific (7.9% versus 40%) and general (7.3% versus 15%). There was a slight difference in relation to the average operative time in favor of laparotomy (p> 0.05), however, the hospital stay was reduced by 5.4 days with laparoscopy (9.3±2.6 versus 14.9±3.2 days, p<0.05) compared with similar indicators in the open appendectomy group. In the second period of the study (2016-2019), compared with the first (2012-2015), it was possible to increase the incidence of good long-term outcomes from 57.7% to 78.3% and reduce the frequency of bad outcomes from 9.2% to 2.5%. Conclusion. Improvement of tactical and technical approaches and the active introduction of endovisual technologies in the surgery of acute complicated appendicitis in children made it possible significantly reduce the frequency of postoperative specific and general complications, and significantly increase the incidence of good long-term outcomes.
Keywords:
Pediatric surgery, Acute complicated appendicitis, Appendicular peritonitis, Laparotomy and laparoscopy
Cite this paper: Akilov Kh. A. , Primov F. Sh. , Khidoyatov Dj. S. , Laparoscopic Versus Open Appendectomy in Pediatric Patients with Complicated Appendicitis, American Journal of Medicine and Medical Sciences, Vol. 10 No. 7, 2020, pp. 448-452. doi: 10.5923/j.ajmms.20201007.02.
1. Introduction
Acute appendicitis is the most common surgical emergency in pediatric surgery with a peak incidence in early adolescence [1-4]. According to the latest data, the incidence of appendicitis is ~ 90/100.000 [5,6]. To date, the incidence of acute appendicitis among preschoolers has decreased to 1.1/10000 (from 2 to 9% of children with acute appendicitis), to 6.8/10000 in children aged 5-9 years and up to 19.3/10000 in children at the age of 10-14 years and prevails in boys (55-60%) [1,7]. The proportion of perforated appendicitis varies widely from 15 to 50% [8,9].Diagnosis of acute appendicitis in children is difficult, which is explained by the non-specificity of symptoms and the atypical manifestations of the disease, the partial coincidence of symptoms with many other common pathologies in children, as well as the child’s inability to express complaints and difficulties in examining the abdominal cavity in this age group [10,11]. A complicated course is diagnosed in 30% of pediatric patients (under 16 years old) with acute appendicitis who are in hospital treatment and is a particularly resource-intensive state [12,13]. Literature data indicate that children with complicated appendicitis have a longer stay, a higher cost of hospitalization and a higher risk of subsequent visits to the hospital compared to children with uncomplicated course.The analysis and comparative assessment of the surgical interventions results in acute appendicitis and its complications in pediatric patients is one of the leading factors in evaluating a particular surgical treatment method. These methods determining the feasibility of widespread introduction of new endovisual technologies in pediatric abdominal surgery, developing and implementing patient management algorithms in perioperative period, which ultimately leads to a sharp decrease in the number of adverse outcomes.This study aims to compare laparoscopic and open appendectomy in a pediatric population.
2. Material and Methods
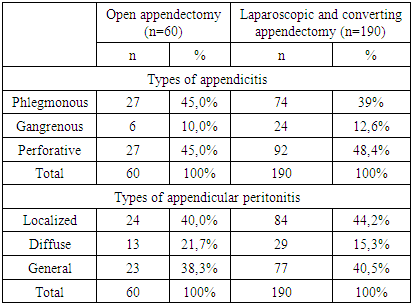
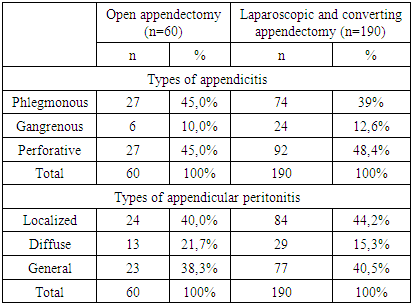
From December 2012 to August 2019, 250 patients (164 laparoscopic appendectomies (LA), 60 open appendectomies and 26 conversion appendectomies (KA)) were performed in the Pediatric Surgery Department with acute appendicitis. Most patients were 13-17 years old (101 cases, 40.4%). Children under 3 years old were 16 (6.4%), 4-7 years old - 61 (24.4%) and 8-12 years old - 72 (28.8%). Most patients were boys - 171 (68.4%).The most common perforated appendicitis was found both in the LA group (48.4% of cases, 92 out of 190) and in the OA group (45.0%; 27 out of 60). In prevalence, in most cases, there was diffuse appendicular peritonitis, 40.5% and 38.3% in the LA and OA groups, respectively (table 1).Table 1. Characteristics of the compared groups with types of appendicitis and the prevalence of peritonitis
 |
| |
|
3. Results and Discussion
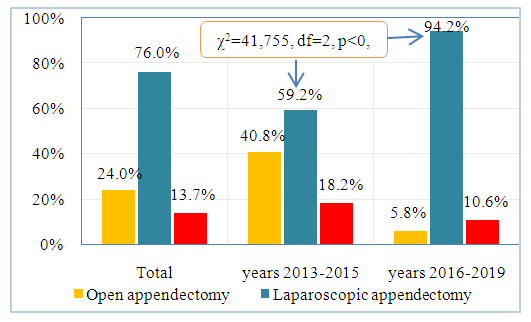
The total endovisual surgical activity in the first period (December 2012-December 2015) was 59.2%, and in the second period (January 2016-August 2019) – 94.2%, which was significantly higher (χ2=41.75, df=2, p<0.001). The overall conversion rate was 13.7%.If we consider the conversion rate over time, the majority of open access conversions occurred in the first 3 years of the analyzed period, when the rate was 18.2% (14 out of 77 cases), while over the past 3 years conversion work was carried out in 12 of 113 cases (10.6%) (Fig. 1).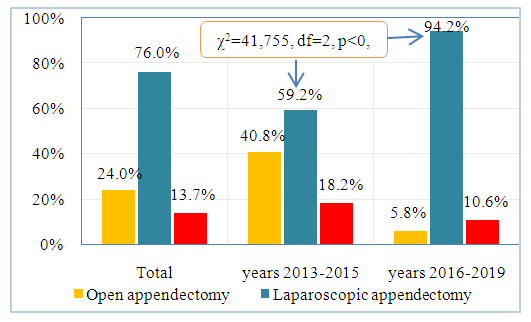 | Figure 1. Indicators of surgical activity in comparison groups |
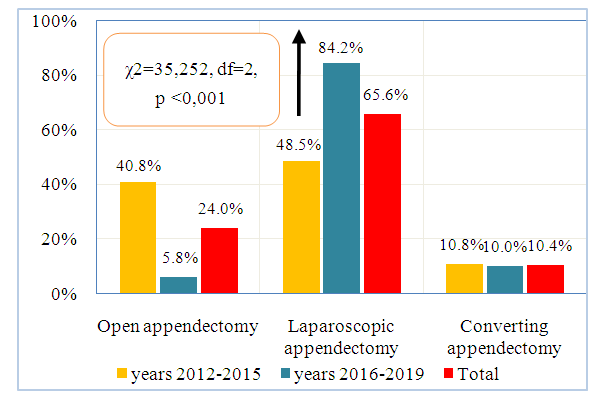
The distribution of patients by the final type of surgical treatment is presented in Fig. 2. So, it is clear that in the comparison group open operations were performed in 53 (40.8%) cases, while the proportion of completed laparoscopic appendectomies was 48.5% (63 out of 130), in 14 (10.8%) cases the operation ended with conversion. 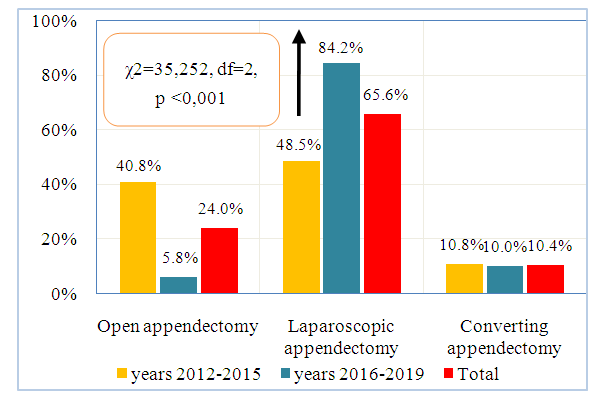 | Figure 2. The distribution of patients by the final type of treatment |
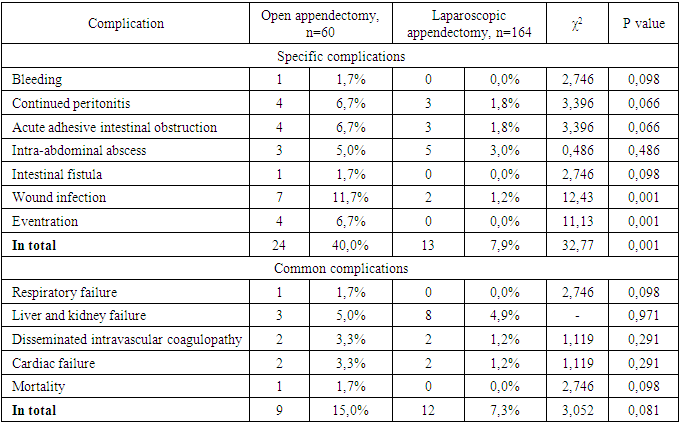
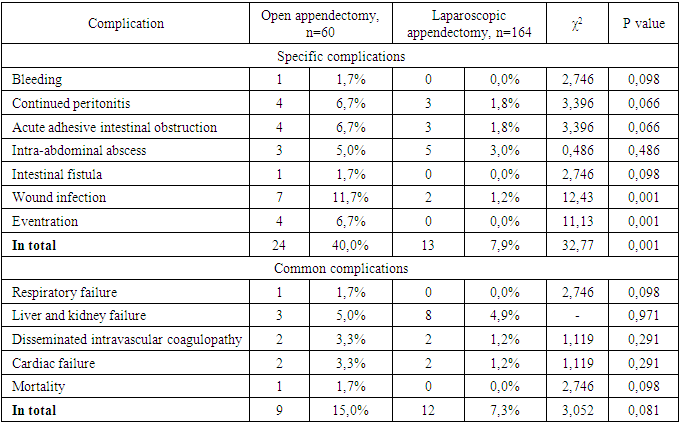
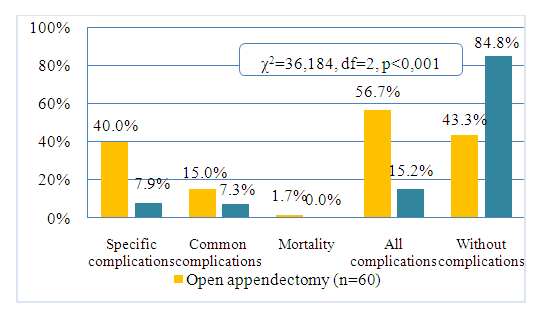
With the accumulation of experience and improvement of technology, the frequency of use of laparoscopy has significantly increased. So, in the main group, the share of completed laparoscopic interventions accounted for 84.2% (101 of 120), and conversions - 10.0% (12 of 120) cases (χ2=35.252, df=2, p<0.001). Open operations were performed in only 7 cases, which amounted to 5.8%.The introduction and active use of the laparoscopic surgical techniques for acute complicated appendicitis in children helped to reduce the frequency of both specific - from 40% in OA to 7.9% in LA (χ2=32.7, p=0.001), and general postoperative complications - with 15.0% to 7.3% (Table 2). So, in the OA, wound infection was significantly less frequently observed (1.2% versus 11.7% of cases, χ2=12.43, p <0.001) and, accordingly, eventration (0.0% versus 6.7% of cases, χ2=11.13, p <0.001). The effectiveness of the laparoscopic technique is convincingly demonstrated by criteria such as a significant decrease in cases of ongoing peritonitis by 4.9% (from 6.7% to 1.8%, p=0.066) and early adhesive intestinal obstruction by 4.9% (from 6.7% to 1.8%, p=0.066) in children after LA. In addition, in this group of patients there was a slight decrease in the frequency of postoperative intra-abdominal abscesses (from 5.0 to 3.0%, p=0.486) and there were no cases of intra-abdominal and gastrointestinal bleeding. Table 2. The frequency and nature of postoperative complications after OA and LA
 |
| |
|
A significantly lower incidence of early complications was revealed in the LA group than in the OA group (15.2% versus 56.7%; χ2=36.18, df=2, p<0.001), both specific (7.9% versus 40%), and general (7.3% versus 15%) (Fig. 3).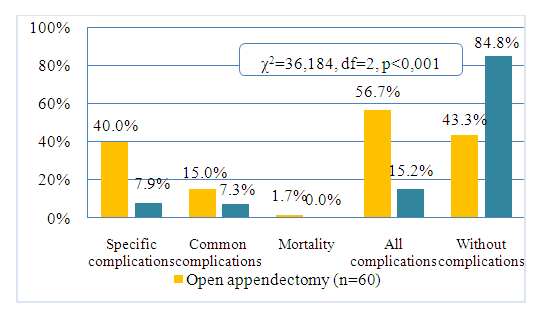 | Figure 3. Early outcomes after acute complicated appendicitis surgery in pediatric patients |
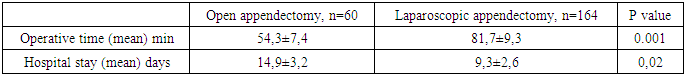
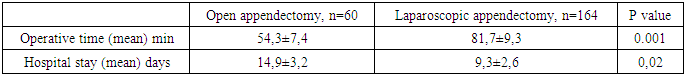
A significant decrease in the frequency of intra-abdominal complications, naturally, had a positive effect on the frequency of repeated laparoscopy and relaparotomy. If in the group of patients after LA the number of patients who underwent repeated surgical interventions was 3.6% (8 of 164), then in children after OA this indicator reached 8.3% (5 of 60) cases (χ2=7.37, p=0.007).Against the background of a significant decrease in the frequency of specific and general postoperative complications in the group of children after LA, we observed a decrease in the rate of postoperative mortality from 1.7% to 0.0% (χ2=2.74, p=0.098).There was a slight difference in relation to the average operative time in favor of laparotomy (p>0.05), however, the hospital stay was reduced by 5.4 days (9.3±2.6 in case of LA versus 14.9±3.2 days in OA, p<0.05) compared with similar parameters in the group of OA (Table 3).Table 3. The operative time and the hospital stay in the comparison groups
 |
| |
|
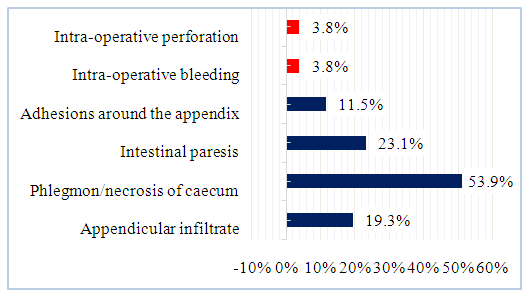
We separately considered the results of CA (n=26). So, the immediate causes of CA are presented in fig. 4. It is seen that pathological changes in the abdominal cavity identified during laparoscopic revision, which caused significant technical difficulties when performing the operation with a minimally invasive method, are most often noted. Thus, in 23.1% (6 of 26) cases, pronounced gastrointestinal paresis was observed, in 19.3% (5 of 26) - dense appendicular infiltrate with abscess formation, in 3 patients (11.5%) - adhesions around the appendix , and most often the cause of CA was phlegmon/necrosis of the cecum, leading to diffuse peritonitis - 53.9% (14 of 26).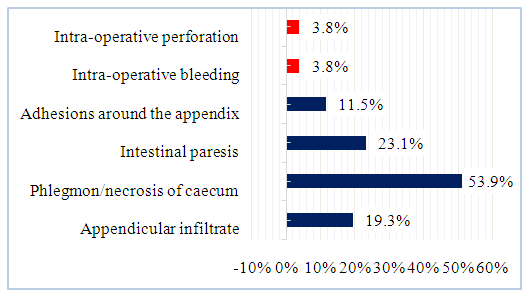 | Figure 4. The immediate causes of the converting appendectomy |
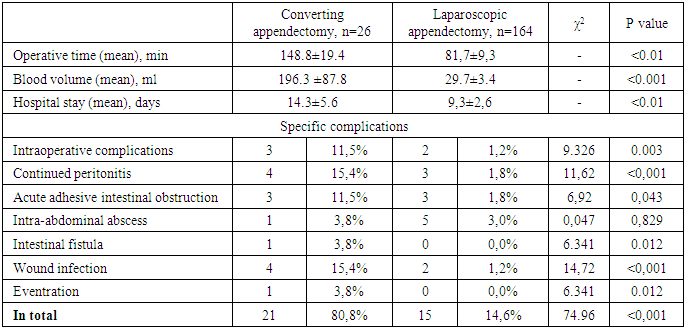
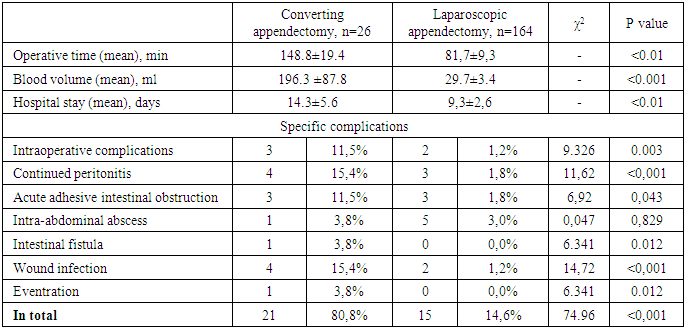
In 3 patients (11.4%) there were intraoperative complications that could not be managed by the endosurgical method: bleeding during excretion of the appendix (1 case, 3.8%), perforation of the appendix at the base (1 case, 3.8%).A comparative assessment of the short-term outcomes and postoperative complications after LA and CA are summarized in table 4. Such indicators as the duration of surgery, and/or blood loss, hospital days had a statistically significant difference, which once again emphasizes the importance of determining preoperative conversion predictors in reducing “negative” LA. Thus, attempts to complete the operation with laparoscopic access, even in cases with severe adhesion or inflamed pathological appendix, resulted in twice as long interventions in CA as in LA (81.7±9.3 min for LA versus 148.8±19.4 min for CA; p< 0.01). Patients after CA had a greater volume of intraoperative blood loss than with LA (29.7±3.4 ml for LA versus 196.3±87.8 ml for CA; p<0.01).Table 4. The frequency and nature of postoperative complications in the CA and LA
 |
| |
|
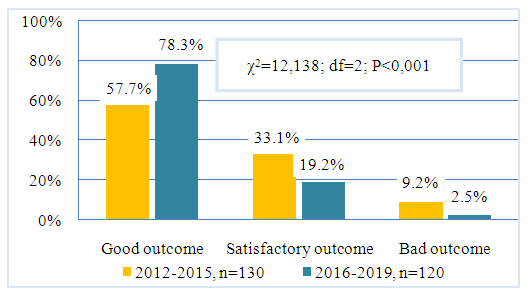
An untimely transition to OA led to intraoperative complications in 3 cases, which also affected the incidence of ongoing peritonitis (1.8% in LA versus 15.4% in CA, χ2=11.62, p<0.001), acute adhesive intestinal obstruction (1.8% against 11.5%, χ2=6.92, p=0.043) and repeated interventions (11.5%). The expansion of operative access also influenced the development of suppuration of postoperative wounds (15.4% for CA compared with 1.2% for LA, χ2=14.72, p<0.001). The overall incidence of specific perioperative complications was higher with CA than with LA (80.8% for CA versus 14.6% for LA; χ2=74.96, p<0.001). In both groups, no fatal outcomes were noted. Patients in the LA group were discharged earlier (9.3±2.6 days for LA versus 14.3±5.6 days for CA; p<0.01).An analysis and comparative evaluation of the long-term results of surgical treatment was carried out in two periods of the study: the main group - the period from December 2012 to December 2015, the comparison group - the period from January 2016 to August 2019.A good outcome was defined as a complete cure for the underlying disease, subject to standard standards for the length of hospital stay. In instrumental studies - the absence of a visible pathology.A satisfactory outcome was determined when treating the underlying disease with the presence of postoperative complications, when standard standards for the duration of the patient’s stay in the clinic were exceeded. In instrumental studies, the absence of gross changes in the abdominal cavity.An unsatisfactory (bad) outcome was noted in the presence of postoperative complications that entailed subsequent repeated surgical interventions or death. In instrumental studies, the presence of gross changes in the abdominal cavity.As shown in fig. 5, the main group of patients was characterized by significantly better long-term results after all operations for complicated acute appendicitis in children in the comparison groups.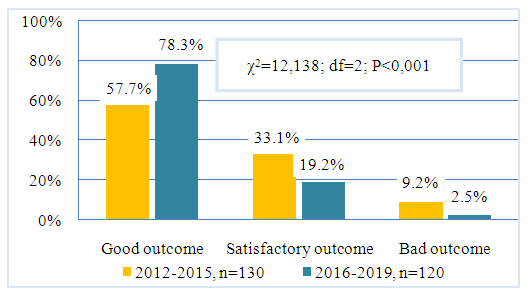 | Figure 5. Summary long-term outcomes after all surgeries |
Thus, 78.3% (94 out of 120) cases accounted for good treatment outcomes, and 19.2% (23 out of 120) cases satisfactory cases, while in the comparison group these indicators were 57.7% (75 out of 130) and 33.1% (41 out of 130) (χ2=12.13; df=2; p<0.001). The incidence of bad results was 9.2% (12 of 130) in the comparison group, 2.5% (3 of 120) in the main group of patients.Our study shows that LA has a clear superiority over OA due to shorter operating time, less intraoperative bleeding, reduced hospital stay, and a decrease in the frequency of specific and general postoperative complications. Our data are partially consistent with the results of Tuggle et al., (2010), which provided data from a nationwide study showing that in cases of complicated appendicitis, LA is better in terms of superficial and deep wound infections; and unlike our results, LA is associated with a relatively greater likelihood of developing an intra-abdominal abscess [14].In another study, C. Athanasiou et al. (2017) reported that with LA (in accordance with our results) there is no significant additional risk of postoperative abscess [15]. In terms of morbidity, in patients with LA, the authors observed 12% fewer cases of intra-abdominal abscess as a postoperative complication [15].The conversion rates reported in the literature are variable. Liu et al. (2017) reported a conversion rate of 9.7%, due to various reasons related to patients, surgeons, or technical factors [16]. The conversion rate in this study is consistent with other published studies, although lower rates (0-3.3%) have also been reported [17,18]. The results of most other studies are that the conversion of surgery to open access prolongs working time, leads to a longer stay in the hospital, and is characterized by a high frequency of postoperative complications, which often requires additional surgical interventions, including drainage of the abdominal cavity, which also increases the rate of bed days.Our results also show that even in cases of diffuse peritonitis, LA can be successfully performed and is associated with important advantages compared with patients undergoing CA. However, in cases where there are several factors (pathological changes in the abdominal cavity) during laparoscopic revision that cause significant technical difficulties, further attempts to perform the operation with a minimally invasive method lead to the development of several postoperative complications and bad treatment outcome.
4. Conclusions
Improvement of tactical and technical approaches and the active introduction of endovisual technologies in the surgery of acute complicated appendicitis in children made it possible significantly reduce the frequency of postoperative specific and general complications, and significantly increase the incidence of good long-term outcomes.
References
| [1] | Almaramhy HH. Acute appendicitis in young children less than 5 years: review article. Ital J Pediatr. 2017; 43(1): 15. Published 2017 Jan 26. |
| [2] | Cameron D, Sidhwa F, Glass CC, Feng C, Rangel SJ. Cost and cost variation burden associated with pediatric surgical conditions: implications for the prioritization of comparative effectiveness studies. Presented at the American Academy of Pediatrics Experience National Conference and Exhibition; October 25, 2015; Washington, DC. |
| [3] | Glass, C.C., Rangel, S.J. Overview and diagnosis of acute appendicitis in children. Semin Pediatr Surg. 2016; 25: 198–203. |
| [4] | Parigi GB, Czauderna P, Rolle U, Zachariou Z. European Census on Pediatric Surgery. Eur J Pediatr Surg. 2018; 28(3): 227-237. |
| [5] | Bhangu A., Soreide K., Di Saverio S. et al Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015; 386: 1278-1287. |
| [6] | Rangel SJ. Time to Appendectomy and Risk of Complicated Appendicitis and Adverse Outcomes in Children-Reply. JAMA Pediatr. 2018; 172(1): 94–95. |
| [7] | Fares A. Summer Appendicitis. Ann Med Health Sci Res. 2014; 4: 18-21. |
| [8] | Drake FT, Mottey NE, Farrokhi ET, et al. Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg. 2014; 149(8): 837-844. |
| [9] | Peyvasteh M, Askarpour S, Javaherizadeh H, Besharati S. Modified alvarado score in children with diagnosis of appendicitis. Arq Bras Cir Dig. 2017; 30(1): 51-52. |
| [10] | Khan YA, Zia K, Saddal NS. Perforated Neonatal Appendicitis with Pneumoperitoneum. APSP J Case Rep. 2013; 4: 21. |
| [11] | Jahangiri M, Hosseinpour M, Jazayeri H, Mohammadzadeh M, Motaharizad D, Mirzadeh AS. Perforated Acute Appendicitis in a Pre-Term Neonate. Iran Red Crescent Med J. 2013; 15: 497-499. |
| [12] | Ingraham AM, Cohen ME, Bilimoria KY, et al. Effect of delay to operation on outcomes in adults with acute appendicitis. Arch Surg. 2010; 145(9): 886-892. |
| [13] | Eko FN, Ryb GE, Drager L, Goldwater E, Wu JJ, Counihan TC. Ideal timing of surgery for acute uncomplicated appendicitis. N Am J Med Sci. 2013; 5(1): 22-27. |
| [14] | Tuggle KR, Ortega G, Bolorunduro OB, et al. Laparoscopic versus open appendectomy in complicated appendicitis: a review of the NSQIP database. J Surg Res. 2010; 163(2): 225-228. |
| [15] | Athanasiou C, Lockwood S, Markides GA. Systematic review and meta-analysis of laparoscopic versus open appendicectomy in adults with complicated appendicitis: an update of the literature. World J Surg. 2017; 41: 3083-99. |
| [16] | Liu Y, Cui Z, Zhang R. Laparoscopic Versus Open Appendectomy for Acute Appendicitis in Children. Indian Pediatr. 2017; 54(11): 938–941. |
| [17] | Cipe G., Idiz O., Hasbahceci M., et al. Laparoscopic versus open appendectomy: where are we now? Chir. (Bucur). 2014; 109: 518-522. |
| [18] | Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L. Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg. 2016 Aug 30; 11(1): 44. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML