-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(6): 430-433
doi:10.5923/j.ajmms.20201006.16

Optimization of Diagnostics and Surgical Treatment Tactics of Duodenal Injuries
Ruziboev Sanjar Abdusalomovich 1, Khaidarov Genadiy Akhadovich 2, Amonov Khudoyberdi Ravshanovich 2
1Samarkand State Medical Institute, Samarkand, Uzbekistan
2Samarkand Branch of the Republican Scientific Center for Emergency Medicine, Samarkand, Uzbekistan
Correspondence to: Ruziboev Sanjar Abdusalomovich , Samarkand State Medical Institute, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This problem, due to its rarity, the development of severe life-threatening complications, is currently a serious and unresolved task in emergency surgery. An analysis of the results of surgical treatment of 41 patients with closed injuries (91.5%) and wounds (8.5%) of duodenal ulcer was performed. In the early stages after an injury, the imposition of duodenoejunoanastomosis in our opinion is the best. In the later stages after the injury, the application of duodenostomy during the period with disabling of the duodenum and with drainage operations of the stomach gave good results.
Keywords: Damage to the duodenum, Surgical treatment
Cite this paper: Ruziboev Sanjar Abdusalomovich , Khaidarov Genadiy Akhadovich , Amonov Khudoyberdi Ravshanovich , Optimization of Diagnostics and Surgical Treatment Tactics of Duodenal Injuries, American Journal of Medicine and Medical Sciences, Vol. 10 No. 6, 2020, pp. 430-433. doi: 10.5923/j.ajmms.20201006.16.
1. Introduction
- Despite more than a century of experience in the treatment of injuries of the duodenum (duodenum), this problem, due to its rarity, the development of severe life-threatening complications, is currently a serious and unresolved task in emergency surgery. Each surgeon involved in emergency surgical care, for the entire time of his professional activity, encounters a duodenal injury (DI) at best from 1 to 3 times and a positive outcome of each DI is a matter of chance, depending on many circumstances. DI is 0.93-10% of cases with open and closed abdominal injuries [2,4,10,12], and among injuries of the gastrointestinal tract - 0.43-6.5%. 76-80% are able-bodied men aged 20-40 years [5,6,12]. To date, the frequency of damage to the duodenum in the structure of injuries of the abdominal cavity is about 1.2% -2 and does not exceed 10% in the structure of injuries of the digestive system [1]. In recent years, there has been a tendency to increase the frequency of damage to the duodenum, which is primarily associated with an increase in the number of road injuries, falls from a height (catatrauma), and wounds to the abdomen with cold and firearms [3].The postoperative period with this type of injury in 25-60% of cases is accompanied by early complications, of which the most formidable and common is the failure of the sutures of the duodenal wound, retroperitoneal phlegmon. In this regard, the mortality rate for DNA damage is very high and ranges from 11-30%, and with developed retroperitoneal phlegmon reaches 100% [4,7,8,11]. To date, there are no unified approaches to determining the nature and extent of surgical intervention for damage to the duodenum [9]. The greatest difficulties in the timely diagnosis are noted with damage to the retroperitoneal part of the duodenum, which are not diagnosed in 10-30% of the victims [5].
2. Materials and Methods
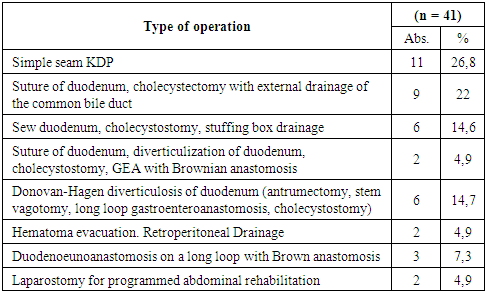
- The analysis of the results of surgical treatment of 41 patients with closed injuries (91.5%) and wounds (8.5%) of duodenal ulcers who were treated at the Samarkand branch of the Russian Center for Emergency Medicine in the period from 2000 to 2019 was carried out. Among the injured men were 36 (87.8%), and women - 5 (12.2%). At the same time, the average age of men was -32.8±9.3 years, women -34.4±13.6 years. Damage to the duodenum in 3 (7.3%) cases was the result of a fall from a height (catatrauma); in 29 (70.7%) cases - car accidents; in 2 (4.9%) - industrial injuries, and suicide attempts in 2 (4.9%) cases, iatrogenic damage occurred in 3 (7.3%) cases, beating - in 2 (4.9) patients. In the first 6 hours after the injury, 39 (75%) patients were admitted to the hospital. In the period from 6 to 24 hours, 29 (70.7%) patients were admitted; after 24 hours, 12 (29.3,%) patients were hospitalized. An isolated injury was found in 17 (41.5%) cases. Combined and multiple injuries accounted for 24 (58.5%), which were more often detected with duodenal injuries, which affected the severity of this type of damage. Damage to the duodenum was combined with pancreatic trauma 8 (33.3%), liver 6 (25%), gall bladder 3 (12.2%), large intestine 4 (16.6%,), small intestine -1 (4.2%) and stomach - 2 (8.3%). Damage to the descending section of the duodenum was detected in 24 (58.5%) cases, in the lower horizontal part in 8 (19.5%) cases, in the upper horizontal part of the duodenum in 9 (22%) cases.Analysis of clinical observations of patients with duodenal ulcer damage was carried out on the basis of anamnesis, patient complaints, objective and instrumental examination data. The results of the study did not reveal pathognomonic symptoms, characteristic damage to the duodenum. In 8.7% of cases, patients did not show any complaints at all. In addition, the clinical picture of the damage to the duodenum in many patients was erased or “masked” by combined injuries of other organs and anatomical areas, lack of consciousness, and alcohol intoxication. Upon admission to the hospital, all patients underwent clinical and biochemical blood tests, X-ray studies, ECG, ultrasound of the abdominal cavity and retroperitoneal organs and diagnostic laparoscopy, and if necessary, computed or multispiral computed tomography. Thanks to the organizational measures and the modern equipment and qualified personnel, it allowed to significantly expand the diagnostic capabilities and reduce the examination time for patients arriving according to emergency indications with closed injuries and wounds of the abdomen and acute surgical pathology. In most patients with injuries and injuries of the abdomen, the examination was performed directly in the operating room against the background of anti-shock measures.
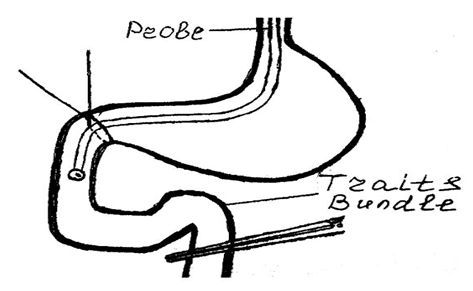 | Figure 1. Diagram of diagnosis of retroperitoneal ruptures of the duodenum |
3. Results
- To determine the most optimal treatment and diagnostic program and continuity in the provision of specialized surgical care, we used the generally recognized classification of E. Moore et al. (1990).• I degree of damage - a slight hematoma or incomplete tear without damage to the mucosa.• II degree of damage - large hematoma or rupture of less than 50% of the circumference.• III degree of damage - a large transverse gap of 50-70% of the circumference (segment D2) or 50-100% of the circumference (segment D1, D2, D3).• IV degree of damage - a very large (75-100%) gap D2, rupture of the ampoule and the distal part of the duodenum.• V degree of damage - massive pancreato-duodenal wound with duvascular duodenum.When treating injured patients with injuries and duodenal ulcers in 11 (26.8%) patients with fresh injury, they limited themselves to the application of the primary suture with drainage of retroperitoneal tissue through a contrapertural incision. In 9 (22%) cases, the primary suture of the duodenum was supplemented with cholecystectomy with external drainage of the common bile duct according to A.V. Vishnevsky. In 6 (14.6%) patients, the primary suture of the duodenum was supplemented with cholecystostomy and drainage of the omental bursa, a decompression probe in the duodenum was installed transnasally for active aspiration, and an enteral probe for enteral nutrition was performed using the Treytz ligament. In case of injuries of less than half the circumference of the duodenum, the primary suture was supplemented by simple diverticulization of the duodenum with the application of a gastroenteroanastomosis on a long loop with Brown anastomosis and cholecystostomy (2 cases, 4.9%), and in 4 (9.7%) cases, duodenum was diverticulized according to Donovan-Hagen (an antrumectomy, stem vagotomy, a gastroenteroanastomosis on a long loop, cholecystostomy).With hematomas, duodenum was limited to the evacuation of hematomas (with mobilization of all departments) with subsequent drainage of retroperitoneal tissue - 2 (4.9%) cases. In 2 cases, due to late circulation and the development of diffuse peritonitis, operations were completed with laparostomy for programmed sanitation of the abdominal cavity. In the last 3 (16.6%) cases, duodenojejunostomy on a long loop with a Brownian anastomosis using prolenic atraumatic threads was applied to the damaged area of the duodenum, and a decompression probe was placed transnasally in the duodenum for active aspiration. In these observations in the postoperative period, complications from the imposed anastomosis were not observed. In 1 patient, due to iatrogenic damage to the descending section of the duodenum, simple duodenum diverticulization was performed with a gastroenteroanastomosis overlaid on a long loop with Braun anastomosis and cholecystectomy, external drainage of the common bile duct by Abba-Pikovsky. Two-lumen drains for aspiration-flushing treatment were brought through a favorite incision. Damage to the duodenum was not sutured due to severe inflammatory infiltrate, limited to retroperitoneal phlegmon, without peritonitis. To prevent the progression of infection of retroperitoneal tissue sections, Dekasana with levomekol was used, which significantly improved the results of surgical treatment. Lumbatomy wound was regularly treated with antiseptic drug Dekasan and ointment Levomekol.
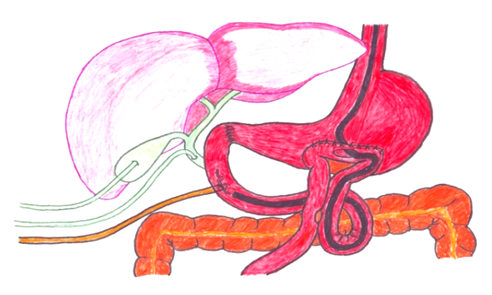 | Figure 2. Simple diverticulization of duodenum, cholecystostomy, choledochostomy, duodenostomy, Welfler gastroenterostomy |
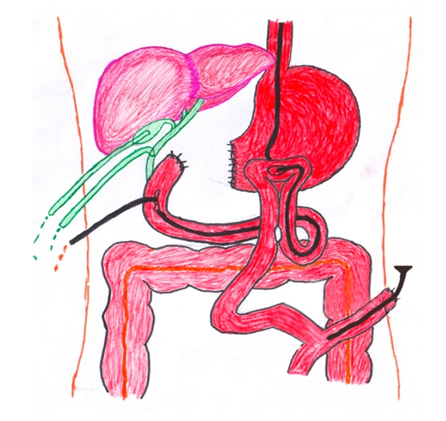 | Figure 3. In 2 cases, the patients underwent Witzel nutritional jejunostomy |
|
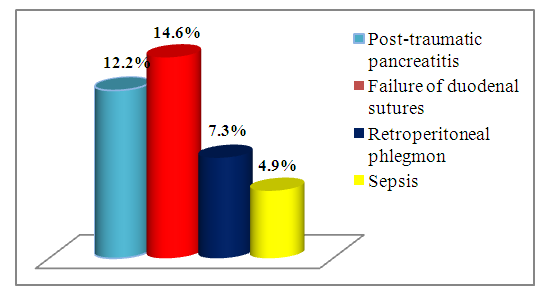 | Figure 4. Complications after surgical treatment of patients with injuries and injuries |
4. Conclusions
- 1. At the present stage, the treatment of victims with damage to the duodenum remains a difficult task requiring further study. The development of new diagnostic techniques and the choice of operations for extensive damage to the duodenum with adequate drug therapy will help reduce the number of postoperative complications and mortality in this severe category of patients.2. An effective measure for the prevention of suture failure and traumatic pancreatitis is decompression through a probe with constant aspiration of the duodenal contents in the postoperative period.3. In the early stages after injury, the imposition of duodenoejunoanastomosis in our opinion is the best.4. In the later stages after the injury, the imposition of duodenostomy over the course of disabling the duodenum and with drainage operations of the stomach gave good results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML