-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(6): 416-421
doi:10.5923/j.ajmms.20201006.14

Deficiency of Actual Bicarbonate as a Risk Factor for Delayed Kidney Transplant Function from a Living -Related Donor
Z. P. Khaybullina, L. A. Nazirova, N. M. Karimova
State Institute “Republican Specialized Scientific-Practical Medical Center of Surgery named after academician V. Vakhidov”, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Kidney transplant recipients are patients with the terminal stage of chronic kidney disease having an initially unfavorable metabolic status, such as hypoplastic anemia, uremic endotoxemia, disturbances in water-electrolyte and acid-base balance. A number of epidemiological studies have shown a link between low serum bicarbonate levels and unfavorable renal outcomes and patient mortality. Aim of research was to study acid-base balance disorders in 246 recipients of living related kidney transplantation and its link with the development of delayed transplant function, based on which to establish threshold values of the most informative indicators of acid-base balance, the excess of which was associated with the risk of developing this condition. Material and methods. The study included 246 recipients of related kidney transplants from a living donor operated at the State Institute “Republican Specialized Scientific-Practical Medical Center of Surgery named after academician V.Vakhidov” from 2010 to 2020. Parameters of pO2, pCO2, HCO3, BE, pH, lactate, hemoglobin, and deep oxygen status (p50) were determined in arterial blood taken in a PICO-70 heparinized syringe using an ABL 800 device (Radiometer, USA). Results. Estimation of the transplant function by the level of creatinine reduction in blood serum of kidney transplant recipients showed that 24 hours after the surgery, the primary functioning transplant occurred in 190 (77.2%) patients, delayed transplant function was in 51 (20.8%) patients, transplant dysfunction - in 5 (2.0%) patients (in 2 (0.8%) of them - due to acute rejection). It was found that determination of HCO3 level and creatinine immediately before surgery is informative to predict the risk of delayed transplant function. A decrease of the actual bicarbonate level of less than 19.8 mmol / l, creatinine of more than 927 μmol / l are risk factors for delayed transplant functioning 24 hours after surgery. Conclusion. Kidney transplantation recipients - patients with terminal stage of CKD - immediately before surgery have compensated MA (actual bicarbonate increase and BE), an increase of pO2 and p50 which indicates a deficiency in the metabolic component of ABB regulation and hyperoxia. It is informative to determine the level of aHCO3, creatinine immediately before surgery to predict the risk of delayed transplant function. A decrease in the actual bicarbonate of less than 19.8 mmol / l, creatinine of more than 927 μmol /l are risk factors for delayed graft functioning 24 hours after surgery.
Keywords: Transplantation, Kidney, Actual bicarbonate, Transplant delayed function
Cite this paper: Z. P. Khaybullina, L. A. Nazirova, N. M. Karimova, Deficiency of Actual Bicarbonate as a Risk Factor for Delayed Kidney Transplant Function from a Living -Related Donor, American Journal of Medicine and Medical Sciences, Vol. 10 No. 6, 2020, pp. 416-421. doi: 10.5923/j.ajmms.20201006.14.
1. Introduction
- Kidney transplantation is the most effective renal replacement therapy [1,2]. Cadaveric transplantation is widely used in the United States, Europe, Russia, Belarus. In particular, the proportion of cadaveric kidney transplantation in Russia makes up 6:1 million people, in Spain - 63: 1 million people, in the USA - 47:1 million people [3]. There is a shortage of donor organs despite the steady increase in the number of kidney transplants worldwide. The demand of population for kidney transplantation is 3,000 per 33 million people in the Republic of Uzbekistan. The legislative basis in our country governs the transplantation of a living-related donor. The advantages of live transplantation are as follows: there is no need to wait for a suitable donor, high immunological compatibility, there is no brain death, a sharp reduction in the time of cold graft ischemia, etc. [4], which is noted in the clinical recommendations of KDIGO [5].The greatest contribution to the development of the terminal stage of chronic kidney disease (CKD) is made by glomerular and tubulo-interstitial kidney diseases, the morbidity rate of which was 407.6 per 100 thousand of the population in 2016 in our country. Today there are more than 11,000 patients with terminal stage of CKD, more than 3,000 patients receive hemodialysis (according to the Republican Information-Analytical Center and the Health Institute data) [6]. After the adoption of the Decree of the President of the Republic of Uzbekistan “On measures for improving the efficiency of the providing nephrological and hemodialysis care to the population of the Republic of Uzbekistan” dated by 12.07.2018, the number of closely related kidney transplants increased. More than 90 kidney transplants have been performed at the Republican Specialized Scientific-Practical Medical Center of Surgery named after academician V. Vakhidov since 2018.One of the important aspects of kidney transplantation is the correction of the initial metabolic status of the recipient for the transplant adequate functioning [7]. Kidney transplant recipients - patients with the terminal stage of chronic kidney disease (CKD), having an initially unfavorable metabolic status such as hypoplastic anemia, uremic endotoxemia, disturbances of water-electrolyte, acid-base balance [8]. A complication of terminal stage of the CKD is chronic metabolic acidosis [9]. A direct correlation between a decrease in glomerular filtration rate (GFR) and a decrease in the level of serum actual bicarbonate as CKD progresses has been proved [10,11]. A number of epidemiological studies have shown a link between low bicarbonate levels and unfavorable renal outcomes and patient mortality [12,13]. The frequency of actual bicarbonate less than 22 mmol / l is about 19% (13-58%) in patients with 4-5 stage of CKD [14]. This level of bicarbonate has been determined as the cut off, requiring correction by the recommendation of KDIGO [15]. Metabolic acidosis (MA) is detected in 15-28% of patients after kidney transplantation, being a predictor of poor prognosis of transplant survival, cardiovascular complications and recipient mortality [16,17,18]. A retrospective cohort study involving 2318 kidney transplant recipients (1997-2015) showed that low CO2 levels 3 months after kidney transplantation (KT) significantly increased the risk of transplant loss and the risk of recipient death, even when GFR was restored [18]. MA at the level of HCO3<24 mmol / l is detected in 40% of recipients after KT, which significantly increases the risk of cardiovascular disorders (ischemia, arrhythmia, acute coronary syndrome) [16]. MA at the level of HCO3<20 mmol / l is associated with an increased risk of death from all causes [17]. The clinical significance of MA estimation and monitoring is reported by many authors, emphasizing the particular vulnerability of kidney transplant cells and the contribution of acid-base balance (ABB) disturbances to the development of endothelial dysfunction, hypertension [19], structural and functional changes in the cardiovascular system, an increase in the expression of pro-inflammatory cytokines genes, which worsens the long-term prognosis and increases the risk of KT functioning disturbance [20,21,22]. In particular, MA and bicarbonate deficiency have a direct negative effect on the kidneys, because an increase in the production of ammonium ions by nephrons at MA conditions triggers an alternative pathway for complement activation which causes tubular lesion [23]. Increased endothelin production at MA initiates tubulo-interstitial damage and contributes to a decrease of GFR [11]. Compensatory increase in the synthesis of bicarbonate in the kidneys with the loss of its ability to reabsorb leads to increased calcification in nephrons [24]. MA promotes the deterioration of perfusion at the level of the microvasculature [20], hyperkalemia and an increase in intracellular sodium, a shift of the oxyhemoglobin dissociation curve to the right with a decrease of hemoglobin affinity to oxygen and desaturation, as well as to violations of deep oxygen status [25]. The homeostasis of hydrogen ions is disrupted at MA which contributes to the inactivation of enzymes, disrupts the function of transmembrane ion channels and receptors, and ultimately leads to cells death [26]. First of all, the most vulnerable are CNS and kidney transplant cells. To ensure the initial functioning of the transplant, careful preoperative preparation is necessary to correct metabolic disorders caused by the absence of excretory function of the kidneys, as well as maintaining a stable constancy of the internal environment of the body at all stages of the perioperative period [24]. It is necessary to avoid ischemic-reperfusion, thrombotic, hemodynamic and intracellular metabolic disorders of the transplant. The study of the acid-base state in KT recipients is important, taking into account the high frequency of metabolic acidosis occurrence in KT recipients and its close relationship with vasomotor, hemodynamic disorders and a direct effect on the activity of intracellular enzyme systems. The study of the respiratory and metabolic components of compensation for ABB disorders has a particular interest, because the decision on the appropriateness and extent of corrective measures depends on this. Determination of the cut off threshold of bicarbonate levels, base excess, anion gap in KT recipients is important.Aim of research was to study acid-base balance disorders in 246 recipients of living related kidney transplantation and its link with delayed transplant function, to establish threshold values of the most informative indicators of acid-base balance (ABB), which was associated with the risk of graft function disturbances.
2. Material and Methods
- The study included 246 recipients of related kidney transplants from a living donor, treated at the State Institute “Republican Specialized Scientific-Practical Medical Center of Surgery named after ac.V.Vakhidov” in 2010-2020. Parameters of ABB (pO2, pCO2, HCO3, BE, pH), lactate, hemoglobin, and deep oxygen status (p50) were determined in arterial blood taken in a PICO-70 heparinized syringe using an ABL 800 device (Radiometer, USA). Serum creatinine and urea concentrations were determined using a Rayto Chemray-240 automatic biochemical analyzer (China), glomerular filtration rate (GFR) was calculated by MDRD, CKD-EPI. Laboratory tests were done at 2 stages of observation: immediately before surgery (before tracheal intubation - stage 1), 24 hours after surgery (stage 2). The transplant was considered to be primarily functioning if the serum creatinine level decreased by 10% or more during the first day after KT. Delayed graft function was observed at a decrease of serum creatinine level in these terms less than 10% of the initial level. A primary non-functioning transplant (transplant dysfunction) was detected with an increase of serum creatinine levels to 10% or more on the first day, or within 2 months after surgery while maintaining the need for hemodialysis. Statistical data processing was performed using the Medic-Calc software package. Data are presented as mean (M) and its 95% confidence interval (95% of CI). We used the ROC-curve analysis method to predict the diagnostic significance of quantitative signs (HCO3, BE, pH, lactate, creatinine, p50) when predicting a specific outcome, including the likelihood of this outcome, calculated using the regression model. The optimal separating value of the above mentioned quantitative sign which allows to classify patients according to the degree of risk of outcome and has the best combination of sensitivity and specificity was determined with its help. The quality of the predictive model obtained by this method was estimated based on the area under the ROC-curve (AUC) with standard deviation (SD) and 95% confidence interval (CI) and the level of statistical significance.
3. Results and Discussion
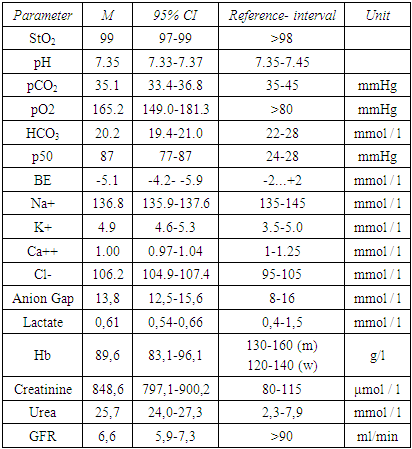
- There were 204 (82.9%) men and 42 (17.1) women from the total number of recipients (n=246). The mean age was 31.4 years (95% CI 29.5-35.6 years); 234 (95.1%) patients underwent program hemodialysis, the duration of which ranged from 1.5 to 58 months, in 167 (67.8%) patients - from 6 to 12 months. All patients, which undergoing programmed hemodialysis (PHD) received a regular PHD session 18-30 hours before surgery. All examined KT recipients had a terminal stage of CKD as evidenced by the level of creatinine, GFR (Tab. 1).
|
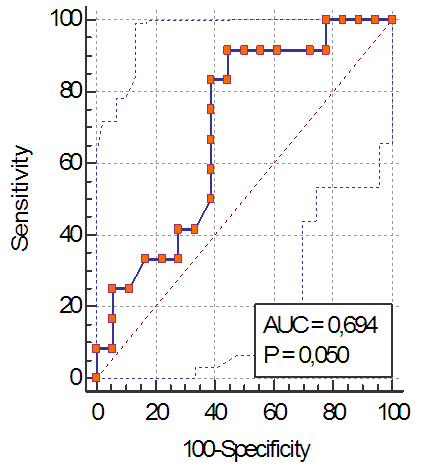 | Figure 1. ROC-curve of actual bicarbonate level before transplantation, quality of the test |
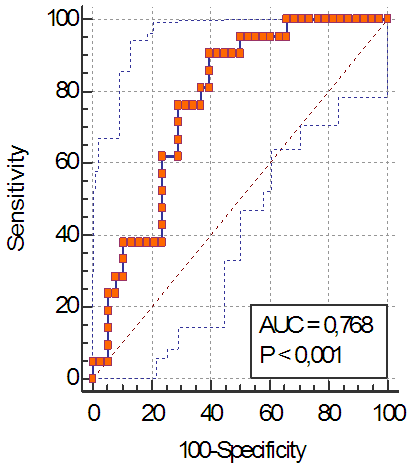 | Figure 2. ROC-curve of creatinine level before transplantation, quality of the test |
4. Conclusions
- Kidney transplantation recipients - patients with terminal stage of CKD - immediately before surgery have compensated MA (actual bicarbonate increase and BE), an increase of pO2 and p50 which indicates a deficiency in the metabolic component of ABB regulation and hyperoxia.It is informative to determine the level of aHCO3, creatinine immediately before surgery to predict the risk of delayed transplant function.A decrease in the actual bicarbonate of less than 19.8 mmol / l, creatinine of more than 927 μmol /l are risk factors for delayed graft functioning 24 hours after surgery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML