-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(6): 400-404
doi:10.5923/j.ajmms.20201006.11

Liver Echinococcosis: Improving of Surgical Tactics
Khakimov M. Sh, Khaitbaev S. K., Imamov A. A.
Urgench branch of Tashkent Medical Academy, Urgench, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to improve the treatment results of patients with liver echinococcosis by developing a differentiated approach to surgical treatment and improving tactical and technical aspects of treatment. Material and methods. The present work is based on the examination and treatment analysis results of 359 patients with various forms of liver echinococcosis. All patients were divided into two groups: control - 243 (68%) patients who were admitted between 2013 and 2016 and the main one - 116 (32%) patients who were hospitalized in 2017-2019. Results. The proposed set of therapeutic measures for liver echinococcosis provides a differentiated approach to the choice of a surgical team depending on the severity of the surgical intervention, increases the efficiency of intraoperative treatment of the residual cavity, improves the technical aspects of surgical intervention and reduces the frequency of postoperative complications from 18.9% to 10.3%, postoperative mortality - from 1.2% to 0%.
Keywords: Echinococcosis, Liver, Hydatid cyst, Residual cavity of the liver
Cite this paper: Khakimov M. Sh, Khaitbaev S. K., Imamov A. A., Liver Echinococcosis: Improving of Surgical Tactics, American Journal of Medicine and Medical Sciences, Vol. 10 No. 6, 2020, pp. 400-404. doi: 10.5923/j.ajmms.20201006.11.
1. Introduction
- Human echinococcosis remains an urgent public health problem in endemic regions, including the Republic of Uzbekistan [1]. Echinococcosis is a serious medical problem in many countries of the world where large endemic foci persist and an increase in the number of cases is observed. The disease affects almost all organs and systems of the body [2].The number of patients with liver echinococcosis (LE) has been increased for recent years. This is due to both the introduction of highly informative diagnostic methods into clinical practice and the downgrade of the social living standards in some regions. The treatment efficiency of echinococcosis is associated with timely and correct diagnostics of this disease. The widespread introduction of modern highly informative instrumental research methods (ultrasound investigation and CT) into clinical practice has significantly improved the early diagnostics of LE [3].Despite the improvement in the diagnostics of the disease, the frequency of unsatisfactory treatment results and postoperative complications exceeds 20% and mortality ranges from 1-2% depending on the nature of the disease course. One of the unfavorable moments is the fact that, despite the high antiparasitic efficacy of the agents (in particular 100% glycerol) used for intraoperative treatment of the residual cavity of liver (RCL), the analysis of long-term results shows that the specific gravity of the LE recurrence has not been changed [4-5]. Echinococcectomy, especially with complicated forms of the disease and giant cysts, is accompanied by suppuration of the residual cavity and the formation of gall-purulent fistula [6]. Aim of the study is to improve the treatment results of patients with liver echinococcosis by developing a differentiated approach to surgical treatment and improving tactical and technical aspects of treatment.
2. Material and Methods
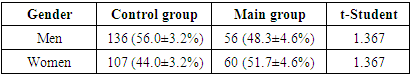
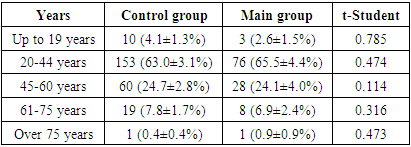
- The study is based on the examination and treatment analysis results of 359 patients with various forms of liver echinococcosis. All patients were divided into two groups: control - 243 (68%) patients who were admitted between 2013 and 2016 and the main one - 116 (32%) patients who were hospitalized in 2017-2019.Such a division is connected with different approaches to treatment as they develop and improve therapeutic and tactical measures. The distribution of patients by gender and age is given in Tables 1 and 2.
|
|
3. Results
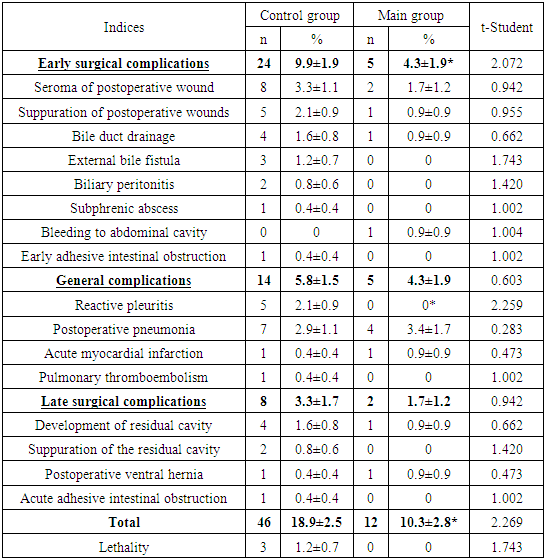
- The proposed therapeutic tactics was used in 116 patients of the main group. 24 of them had a complicated course of the disease, 92 – uncomplicated one. After examination and preoperative preparation 112 patients were performed elective surgery; 3 patients with a rupture to the bile ducts and phenomena of obstructive jaundice were performed an emergency-delayed surgery after RPCG with EPST; 1 patient was operated on an emergency basis when EC was ruptured into the free abdominal cavity. According to our system, in 61 (52.6 ± 4.6%) cases surgical intervention was rated as “light”, in 36 (31.0 ± 4.3%) - as “moderate-severe” and in 19 (16.4 ± 3.4%) - as "severe”. There were 131 (53.9 ± 3.2%; t = 0.235), 74 (30.5 ± 3.0%; t = 0.112) and 38 (15.6 ± 2.3%; t = 0.179) observations in the control group respectively. The absence of a statistically significant difference in the frequency of surgical interventions by their severity in clinical groups indicates the representativeness of the comparative studies.The overall frequency of early postoperative surgical complications was 4.3%. Seroma of the postoperative wound was most often observed, the frequency of which was 1.7% (2 cases). Suppuration of the postoperative wound was noted in 1 (0.9%) patient. Bile leakage was noted in 1 (0.9%) observation. Bleeding from the abdominal cavity on the 2nd day after echinococcectomy of the liver and dissection of adhesions with recurrent echinococcosis was noted in 1 (0.9%) case. Conducted conservative hemostatic therapy was ineffective. The patient was reoperated. In a comparative aspect, the incidence of early surgical complications in the main group significantly decreased relative to the control group from 9.9 ± 1.9% to 4.3 ± 1.9% (t = 2.072).The total frequency of general complications in the postoperative period in the main group was 4.3%. The development of postoperative congestive pneumonia was noted in 4 (3.4%) cases. The development of acute myocardial infarction against the background of existing CHD in the early postoperative period was noted in1 (0.9%) patient. There were no significant differences between the clinical groups in a comparative aspect, the frequency of general postoperative complications in the main group slightly decreased relative to the control group from 5.8 ± 1.5% to 4.3 ± 1.9% (t = 0.603). In the late postoperative period, the complication rate was 1.7%. In 1 (0.9%) patient with a giant LE complicated by a rupture into the abdominal cavity, a residual liver cavity was developed in the postoperative period. A ventral hernia was developed in 1 (0.9%) case 1 year after surgery. There were no cases of relapse. A statistically insignificant decrease in late postoperative complications from 3.3 ± 1.7% to 1.7 ± 1.2% was noted in the main group relative to the control group. There were no lethal outcomes in the main group, but in a comparative aspect with the control group, where the mortality rate was 1.2 ± 0.7%, there was no statistically significant difference (t = 1.743) (Tab. 3).
|
4. Discussion
- The analysis of the clinical treatment results of patients in the control group showed that the incidence of postoperative complications was 18.9%, mortality - 1.2%. Our results treatment of patients with EP completely correlate with the data of Agaev R.M. (2001), Wafin A.Z. (2002), Zhuravlev V.A. (2004), which indicate that the incidence of postoperative complications ranges from 4.8% to 9.7%, with a total mortality rate reaching 1% [7-9]. It should be noted that the relatively high frequency of postoperative complications is due to tactical approaches to the treatment of LE. These authors adhere resection methods of treatment (pericystectomy, economical liver resection, anatomical liver resection). Many domestic researchers (Akhmedov R.M., 2003; Karimov Sh.I., 2006), like us, consider echinococcectomy with the implementation of various methods of the residual liver cavity capitonnage as the main method of treatment. Their results are approximately identical to ours (the incidence of postoperative complications ranges from 5.2 to 5.9%, mortality - from 0.6 to 0.9%) [10-11].As Lebedev N.V. (2007) has shown in his research, the high incidence of postoperative complications is due to difficulties in diagnosing complicated forms of the disease, the lack of objective criteria for determining the severity of an upcoming operation, the presence of errors and complications in the surgical treatment of LE [12]. Given this fact, Lokhvitsky V.S. (1991) believes that improving of surgical treatment results largely depends on an adequate approach in assessing the severity of the patients’ condition, a rating approach to surgical intervention [13-14].Gaybatov S.P. (2006) in his studies proved a direct dependence of the infectious complications frequency from the residual cavity of the liver (RCL) on the level of microbial contamination. The incidence of RCL suppuration at bacterial contamination of echinococcal fluid in 103-104 CFU / ml is 5.4% and at dissemination of 107-108 CFU / ml - 64.8% [15]. Intraoperative RCL treatment is advisable at complicated forms of LE. Electrolysis aqueous solution (EAS) obtained by electrochemical oxidation, in particular sodium hypochlorite, have found increasing application in medicine for recent years. As it has been shown by Petrosyan’s E.A. (1991) research, during blood electrolysis in the form of an intermediate product, sodium hypochlorite is formed which has an evident antibacterial effect, a sharp increase of bacteria sensitivity to antibiotics, a disinfectant action [16].We developed quantitative criteria for evaluating a surgeon’s rating, adequate methods for assessing the severity of surgical interventions at LE and indications for a particular surgical team to perform various surgical interventions were determined by conducting statistical studies, depending on the severity of the upcoming operation. We have chosen EAS of sodium hypochlorite, which has a number of properties that fully meets our requirements for intraoperative treatment of RCL. Our experimental studies have revealed the antiparasitic properties of EAS of sodium hypochlorite, once again have proved the high antimicrobial effectiveness of this antiseptic and morphological studies have proved its safety.Of course, our studies do not completely solve the problem of LE surgical treatment. Currently, it is necessary to continue the search for ways to improve the results of surgical treatment of echinococcosis. It is necessary to improve methods for early diagnostics of the disease, prevention of relapse, to reduce the frequency of complicated forms. Existing accesses to various segments of the liver need technical improvement. The search for tools that can achieve high anti-parasitism and reduce microbial contamination with minimal aggression on the liver tissue is needed. The use of video endoscopic interventions for LE requires the development of treatment standards.
5. Conclusions
- At the traditional treatment of LE, the overall incidence of postoperative complications was 18.9%, mortality - 1.2%. The analysis revealed that the unsatisfactory treatment results were due to the lack of a differentiated approach to the choice of surgical team depending on the severity of the upcoming operation and the preparedness of the surgeon, the presence of technical shortcomings in surgical interventions with a high risk of developing inconsistency of sutures of sutured large biliary fistulas, the need to develop new ways to achieve intraoperative aparasitism with minimal aggression on the liver tissue.Determining the level of the surgeon’s preparedness allows to have a differentiated choice of the surgical team depending on the severity of the upcoming operation. The proposed set of treatment measures for LE allows to increase the efficiency of intraoperative treatment of the residual cavity, to improve the technical aspects of surgical intervention and helps to reduce the frequency of postoperative complications from 18.9% to 10.3%, postoperative mortality - from 1.2% to 0%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML