-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(6): 358-362
doi:10.5923/j.ajmms.20201006.02

Prevalence of Mycoplasma hominis Infection in Pregnant Women with an Adverse Pregnancy Outcome: A Prospective Study
Osama Mohammed Saed Abdul-Wahab 1, Hamid Mubashar M. Mubashar 2, Aisha Rizwan 3, Safinaz Ibrahim Khalil 4, Nazar M. Abdalla 5
1Assistant Professor of Medical Microbiology, MSc, PhD, Department of Clinical Laboratory Science, Faculty of Applied Medical Science, King Khalid University, Abha, Kingdom of Saudi Arabia
2Consultant of Obstetrics & Gynecology, MBBS, MD, ABOG, Omudurman Maternity Hospital, Khartoum, Sudan
3Specialist of Obstetrics and Gynecology, MBBS, Abha Maternity and Children Hospital, Kingdom of Saudi Arabia
4Lecturer of Clinical Pharmacology, MBBS, MSc, Department of Medicine, Faculty of Medicine, University of Medical Sciencs, Khartoum, Sudan
5Assistant Professor of Medical Microbiology, MSc, PhD, Department of Microbiology, College of Medicine, King Khalid University, Abha, Kingdom of Saudi Arabia
Correspondence to: Osama Mohammed Saed Abdul-Wahab , Assistant Professor of Medical Microbiology, MSc, PhD, Department of Clinical Laboratory Science, Faculty of Applied Medical Science, King Khalid University, Abha, Kingdom of Saudi Arabia.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Genital Mycoplasmas are implicated in a number of adverse outcome of pregnancy and some other conditions. M hominis might be associated with or causing the conditions such as ectopic pregnancy, spontaneous preterm labour, preterm prelabour rupture of the membranes, pelvic inflammatory disease, maternal postpartum or postabortal fever, Low birth weight and bacterial vaginosis. Objectives: To evaluate the prevalence of Mycoplasma hominins infections among the pregnant woman and its association with an adverse pregnancy outcome and some other conditions at maternity and Children Hospital, in Abha (a city southwest region), Saudi Arabia. Methods: A hundred pregnant patients (mean age 29.00 years) were enrolled in the study whose urogenital swabs were analyzed for the presence of Mycoplasma hominis. Detailed history was obtained for all patients including an adverse pregnancy outcome and some other clinical conditions. Results: The incidence of Mycoplasma hominis among pregnant woman was 12 positive out of 100(12%) associated pregnancy outcomes and other conditions including threatened miscarriage, 5/12, and spontaneous preterm labour, 3/12 were the most common clinical conditions and all other condition including, ectopic pregnancy, pelvic inflammatory disease, preterm prelabour rupture of membrane and secondary infertility, were observed as the less common, 1/12. All positive isolates were identified as Mycoplasma hominins. Conclusion: Our study shows considerably a higher prevalence due to Mycoplasma hominis infections in pregnant patients and its associated various pregnancy outcomes and other clinical conditions and further work studies are needed for the role and the effect of this pathogen in patients with genital tract infections.
Keywords: Prevalence, Mycoplasma hominins, Pregnancy outcomes
Cite this paper: Osama Mohammed Saed Abdul-Wahab , Hamid Mubashar M. Mubashar , Aisha Rizwan , Safinaz Ibrahim Khalil , Nazar M. Abdalla , Prevalence of Mycoplasma hominis Infection in Pregnant Women with an Adverse Pregnancy Outcome: A Prospective Study, American Journal of Medicine and Medical Sciences, Vol. 10 No. 6, 2020, pp. 358-362. doi: 10.5923/j.ajmms.20201006.02.
Article Outline
1. Introduction
- Genital mycoplasmas (collectively, Mycoplasma genitalium, Mycoplasma hominis and Ureaplasmaspp.), are most often implicated in genital or reproductive health conditions [1]. Mycoplasma hominis and Ureaplasma urealyticum are suspected to be the causative agents of vaginitis, cervicitis, pelvic inflammatory disease (PID), pregnancy complications, prenatal infections, infertility, non-gonococcal urethritis, and acute epididymitis [2,3,4,5,6]. Genital mycoplasmas have been implicated in a number of adverse outcomes of pregnancy such as spontaneous pretermlabour (SPTL) and pretermbirth (PTB) as an important contributor to perinatal mortality and morbidity When Mycoplasma hominis has an integral part in this problem, it will likely to contribute through its involvement with bacterial vaginosis (BV) [9]. Previous PID, particularly that resulted in damage to the fallopian tubes, often leads to an ectopic pregnancy but there is a little evidence to suggest that M.hominis could have a mycoplasmal aetiology [9], Other adverse outcome of pregnancy, include PTB which is often classified by clinical presentation, namely, SPTL about 50%, preterm prelabour rupture of the membranes (PPROM), 30% and medically induced preterm birth because of fetomaternal indications 20%, Although the cause was multifactorial, various microorganisms have been linked to the pathogenesis of preterm birth, by ascending from the lower genital tract and sometimes penetrating the chorioamnion, followed by chorioamnionitis, invasion of the amniotic cavity and fetal infection [9].In Saudi Arabia, there are very little information concerning the prevalence of Mycoplasma hominis infections in pregnant woman and there is lack of national data available from the community in this country and apart from a study of detection of Mycoplasma hominis and Ureaplasma urealyticum that has been conducted recently [7], It was found that two specimens out of 263 infertile female patients specimens screened for genital mycoplasmas were positive with culture-proven infections as M. hominis [7], Therefore, it seem it is an important in the present prospective study to investigate and determine the prevalence of Mycoplasma hominis infections among pregnant woman and its association with an adverse pregnancy outcome and some other conditions at maternity and children hospital in Abha (a city southwest region), Saudi Arabia.
2. Materials and Methods
- This is a prospective Study that conducted at Abha maternity and children hospital in Saudi Arabia over a period of one year from January 2015 to December 2016. A hundred pregnant patients of reproductive age (mean age 29.00 years.) were attending the Outpatient Clinic of obstetrics & gynecology department in the hospital whose urogenital swabs were analyzed for the presence of Mycoplasma hominis. All investigated patients had symptoms of genital infections. A detailed history including an adverse pregnancy outcome and some other clinical conditions were obtained from pregnant woman. These conditions include, the post-partum or post-abortum fever, PID, ectopic pregnancy, cervical cerclage with threaten miscarriage, PPROM.Genital swabs for detecting genital mycoplasma were taken from patients and was inoculated into mycoplasma transport medium (l0 B broth) for culture of mycoplasma. Shepard's growth medium was processed for recovery of Mycoplasma hominis. All inoculated broths were incubated aerobically at 37°C and cultures showing pH shift were sub-cultured onto agar plates, which then incubated anaerobically in a candle jar at 37°C up to 7 days. Agar plates were examined every 24-72 hours under stereomicroscope for the characteristic of Mycoplasma hominis colonies. Isolates were identified serologically as M. hominis by growth inhibition test (disc method), as described by Clyde [8]. The approval of the Ethics clearance and approval for conducting this research was granted by committee of abha maternity and children hospital director. Data were analyzed using the SPSS version 13.0 (SPSS software, Inc., Chicago, USA).
3. Results
- One hundard pregnant woman were studied (mean age 29.00 years). Age distribution of Pregnant women group infected with Mycoplasma hominis As shown in Figure 1.
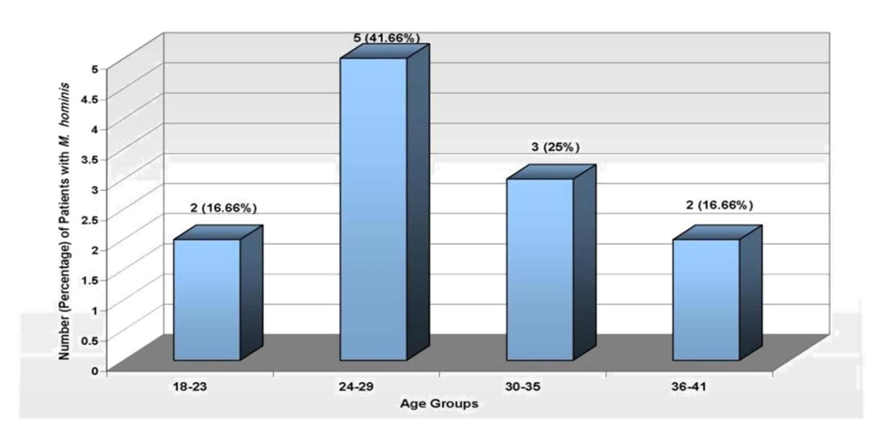 | Figure 1. Age Distribution of Pregnant Women infected with mycoplasma hominis (n=12) |
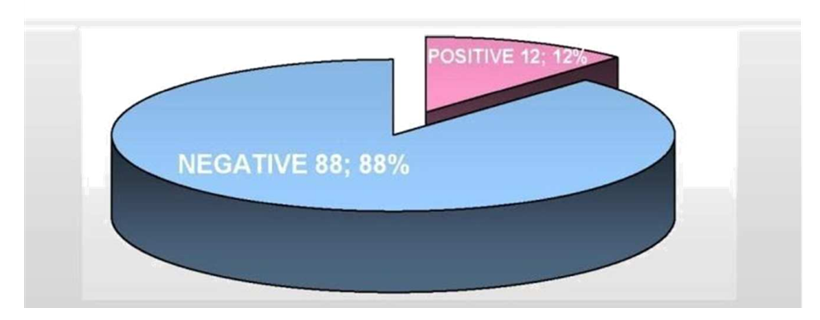 | Figure 2. Prevalence of M. hominis Among Pregnant Women |
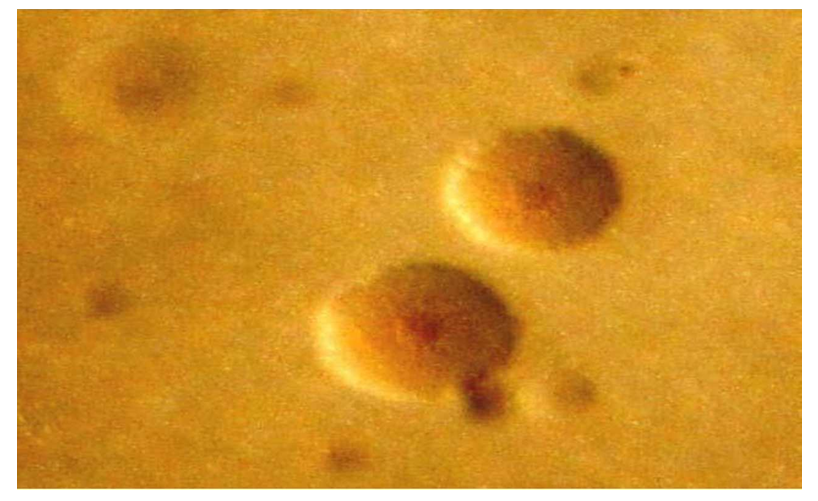 | Figure 3. Colonies of detected Mycoplasma hominis grown on A8 medium after 72 hours of incubation |
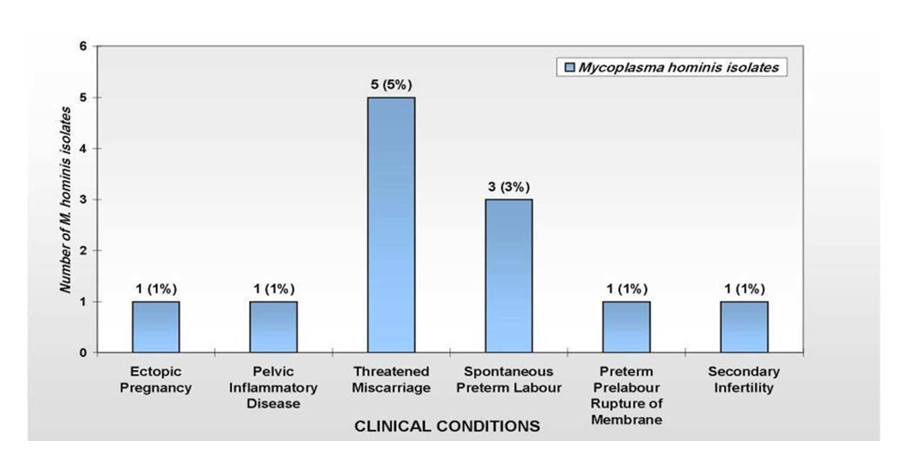 | Figure 4. Numbers of Mycoplasma hominis infections with Adverse Pregnancy Outcomes (12%) |
4. Discussion
- In this study, we found a higher rate (12%) prevalence of M hominis among pregnant women diagnosed with its association with an adverse pregnancy outcome and some other conditions in this country. Our the first recent study reported for detection of Mycoplasma hominis from infertile females was with low prevalence rate of (0.8%) [7], although the incidence and occurrence is still to date with no information studies, To the best of our knowledge, this was the first study to examine the prevalence of patients with pregnancy that showed M. hominis infections had a high prevalence rate (12%) among pregnant women diagnosed with its association with an adverse pregnancy outcome some other clinical conditions than our the first reported study for detection of Mycoplasma hominis from infertile females (0.8%) [7]. Occurrence of Mycoplasma hominis infections in association with pregnancy outcomes and other clinical conditions have been reported in other studies [2,3,4,5,6,7,9]. In addition to the considerable prevalence of Mycoplasma hominis of our study, there are several previously published reports revealed various prevalence rates for this organism. In study conducted by Akya, et.al. [10], they reported the prevalence of M. hominis and Ureaplama urealyticum were 34.9% and 6%, respectively, which was higher than our results while in some other studies the prevalence of these bacteria was lower [11,12]. The different prevalence rates reported by previous studies may be due to factors, including the population tested whether the subjects had received antibiotics, had a genital infection or not, and type of samples (vaginal swabs, cervical swabs, urine, etc.), number of samples collected, methods of sampling, experimental methods, age, socioeconomic status, geographical area, season of sampling and even climate of the sampled area [13]. Furthermore, detection of mycoplasmas in the genital tract usually depends on culturing specimens on appropriate media and identifying the isolates, which was found to be the most sensitive method for the isolation of both M. hominis and U. urealyticum [14]. The lower detection rate of Mycoplasma hominis might be due to high sensitivity of mycoplasma (pH, temperature, and materials present in culture media and clinical specimens) as well as loss of viability during specimen collection and/or transport [14,15], However, the use of other diagnostic method, such as, PCR could be necessary as it was used as a safe, sensitive, specific and fast method for diagnosis of M. hominis and U. urealyticum [7,13], and found to be higher compared with culture in detection of genital mycoplasmas infections [16] and has an advantage of detecting DNA of dead organisms [7,17]. We believe further studies are needed to investigate the use of PCR as superior sensitive molecular diagnostic method than culture method and allow fast and reliable diagnosis for detecting Mycoplasma hominis and the treatment of the positive cases and prevent infection.In this study, the clinical conditions in pregnant women infected with Mycoplasma hominis (12%) have threatened miscarriage 5/12 and Spontaneous Preterm Labour 3/12, were the most common symptoms among these patients whereas other conditions will include ectopic pregnancy, PID, PPROM, and one pregnant women case with secondary infertility for previous five years has been observed as the less common clinical condition 1/12, were observed (Fig.4). Recent study shown that genital mycoplasma, namely, Ureaplasma urealyticum, U. parvum and M. hominis have increasingly been linked to adverse pregnancy outcomes such as, miscarriage, SPTL, pre-term premature rupture of fetal membranes, still birth and low birth weight, However, there is still no definitive consensus on their causative role [18]. There are an accumulated evidence that considering M. hominis may be of significance in the condition of BV which in turn has been associated with subsequent early pregnancy loss [19]. In study conducted by investigators, it has been found that Mycoplasma hominis, and Ureaplasma urealyticum were associated with an increased risk of early miscarriage. [18,19]. Mycoplasma hominis may act symbiotically with other BV associated bacteria or as the sole pathogen based on the observation that this mycoplasma can be found in large numbers in the vagina of most women with BV, but less often in healthy women [18,20]. Association of the genital mycoplasmas in adverse outcomes of pregnancy has been complicated by the presence or absence of BV, and this will requires further research investigation [9]. Previous PID, particularly if this has resulted in damage to the fallopian tubes, often leads to an ectopic pregnancy, whereas Neisseria gonorrhoeae and Chlamydia trachomatis are the most likely causative organisms, there is no evidence that Ureaplasmas can cause PID, and there is a little evidence to suggest that M hominis can cause the condition, thus, there is a small chance that an ectopic pregnancy could have a mycoplasmal aetiology, but further studies need to be conducted [9,21]. In this study, infertility in one case of pregnant woman has been observed as the less common clinical condition, 1/12, associated with M hominis infection. Although previous studies have been demonstrated the association of genital mycoplasmas with variety of genital infections, however, the possible role in infertility is not clear and there has been little enthusiasm in many other previous studies for concluding that Ureaplasma spp. or M. hominis plays an important role in infertility [7,14,22].In our study and due to limitation there was no consideration for coinfections of pathogens other than mycoplasmas. Furthermore, as the study was a prospective, it was impossible to test more subjects within the limited planned period of the study, thus, the clinical conditions observed will reveal that clinical diagnosis and confirmation of infections for Mycoplasma hominis, and to other genital mycoplasmas, namely, Ureaplasma urealyticum, Mycoplasma genitalium, will need further clinical and laboratory studies.
5. Conclusions
- This study shows considerably a higher prevalence due to Mycoplasma hominins infections as compared with previous study in pregnant women in our population. These infections such as threatened miscarriage, spontaneous preterm labour, were observed the most common observed clinical conditions among pregnant woman whereas other conditions include ectopic pregnancy, pelvic inflammatory disease, preterm prelabour rupture of membrane and secondary infertility as the less common condition, However, there is still no definitive consensus on their causative role. Therefore, it is important in order to maintain a safe pregnancy outcome, testing for detecting and identify culture mycoplasma isolates and treatment with use of appropriate antibiotic susceptibility tests in diagnostic laboratories.
ACKNOWLEDGMENTS
- The authors thank Daniel R. Brown, from Department of Infectious Diseases and Immunology, College of Veterinary Medicine, Gainesville, University of Florida, for kindly providing antisera of Mycoplasma hominis-Type Strain-PG21.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML