-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(5): 298-302
doi:10.5923/j.ajmms.20201005.05

Plastic Surgery with Deltopectoral Flap for Facial and Scalp Extensive and Through Defects
Kayumkhodjaev A. A., Nizamkhodjaev Sh. Z.
Republican Specialized Scientific-Practical Medical Center of Surgery Named after Academician V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

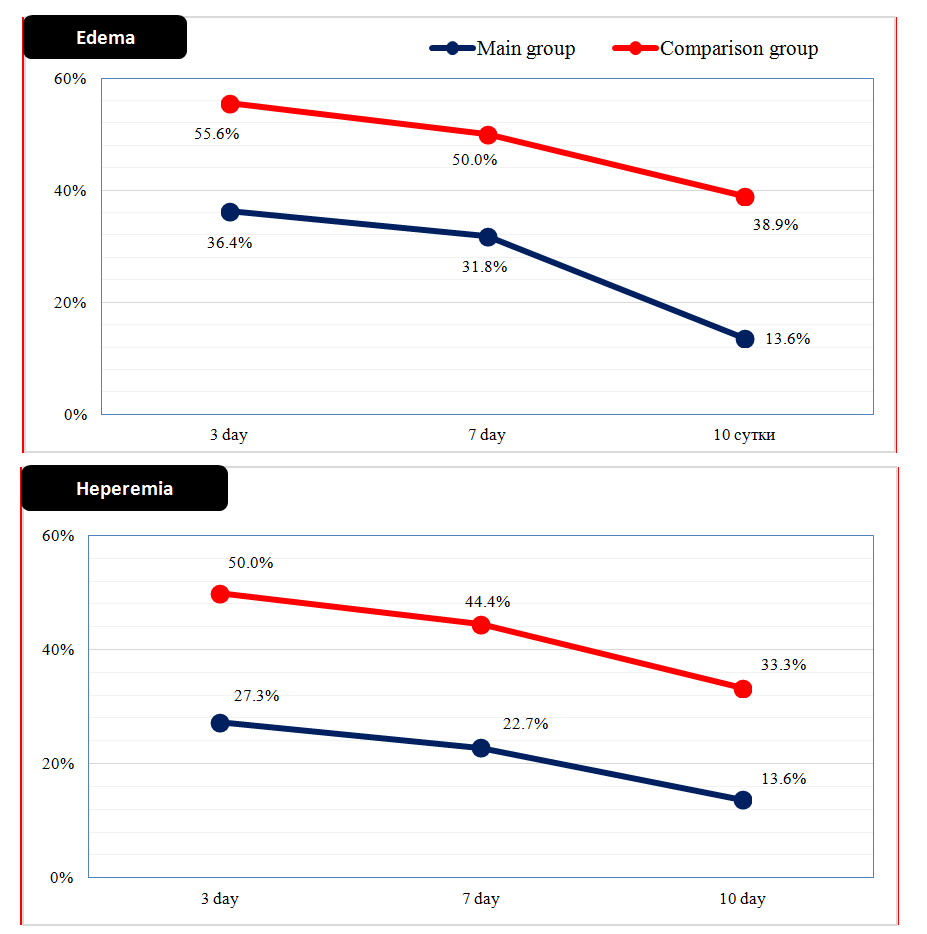
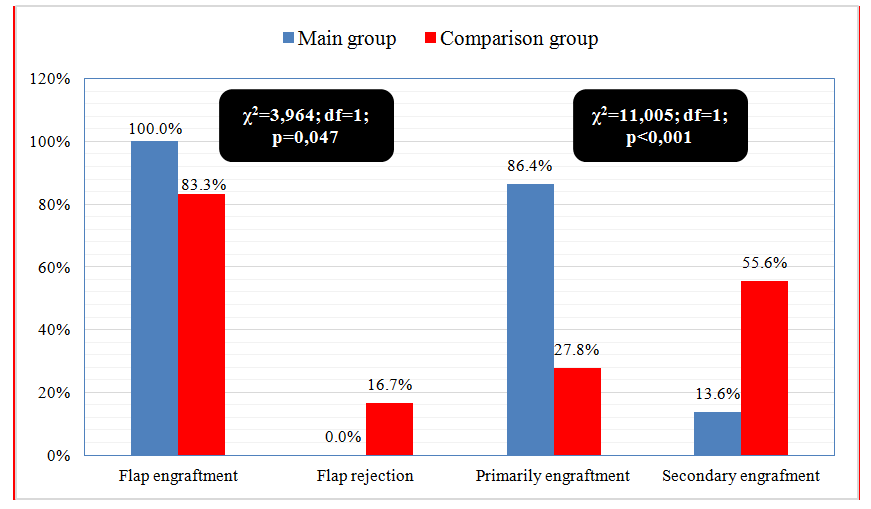
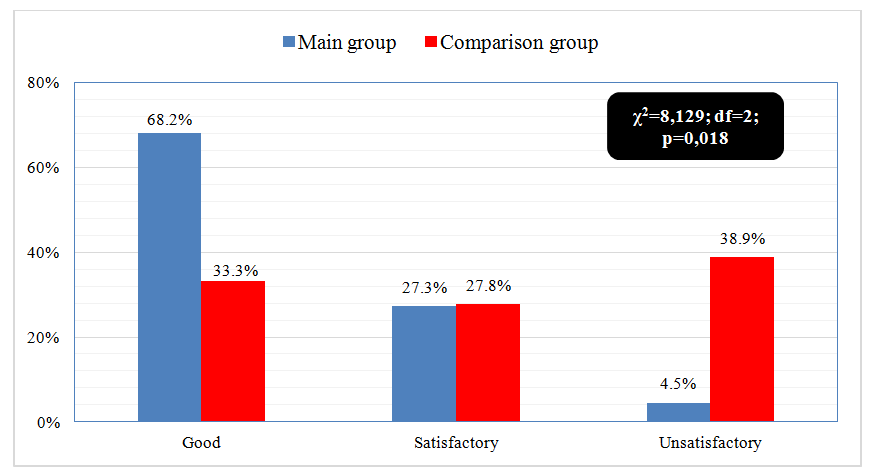
Objective: a comparative analysis of the results of surgical treatment of patients with face and scalp defects. Material and methods. The comparative study was conducted in 2 groups – 40 patients with face and scalp extensive and through defects. In the main group (n=22), plastic surgeries were performed using a deltopectoral flap, and in the comparison group (n=18) – using a free flap on microvascular anastomoses. To assess the patients quality of life after surgery, a modified University of Michigan head and neck quality of life questionnaire (UM-HNQOL) was used. Results. Complications with impaired graft trophic features were observed in 55.6% (in 10 of 18) cases in the comparison group and in 13.6% (3 of 22) in the main group (p<0.001), where flap engraftment was noted in 100% of cases, then as in the comparison group - in 83.3% (15 of 18) (p=0.047). A study of long-term outcomes showed that the frequency of unsatisfactory results in the comparison group was 38.9% (in 7 of 18 patients), in the main group - 4.5% (in 1 of 22) (p=0.018). The quality of life indicator in the main group increased from 54.9±6.3 (initial) to 85.6±3.0 in the long term after surgery. Conclusion. The closure of extensive and through face and scalp defects with delto-pectoral axial flap and preliminary “trial hardening” and improving the graft blood supply is a highly effective technique and allows to ensure 100% flap engraftment, increasing the frequency of good long-term functional and aesthetic results and improve the quality of life of patients.
Keywords: Face and scalp extensive and through defects, Plastic microsurgery, Deltopectoral flap, Immediate and long-term outcomes
Cite this paper: Kayumkhodjaev A. A., Nizamkhodjaev Sh. Z., Plastic Surgery with Deltopectoral Flap for Facial and Scalp Extensive and Through Defects, American Journal of Medicine and Medical Sciences, Vol. 10 No. 5, 2020, pp. 298-302. doi: 10.5923/j.ajmms.20201005.05.
1. Introduction
- Plastic reconstruction surgery of the face and scalp defects, which include various component, is the subject of an ambiguous approach in various clinics of the world. Only the main goal remains single – this is the restoration of form, function and improving the quality of life of patients. The increase in the number of victims with face and scalp injuries of the facial, the severity of the resulting post-traumatic and post-surgical defects, the severity of the complications of the wound process and the complications of radiotherapy, necessitate a full anatomical and functional restoration of the lost area. Today it is impossible to imagine the full-fledged elimination of extensive and through face and scalp defects without microsurgical autologous tissue transplantation, which is able to restore the lost shape and function, thereby improving the quality of life of patients. The last two decades indicate significant achievements in reconstructive microsurgery of the maxillofacial region. Against this background, developments in the field of reconstructive microsurgery have led to the widespread use of various skin-fascial flaps [1,2]. At the same time, specialists in this field began to focus on individual methods of plastic surgery for specific defects, classifications are often discussed to determine the choice of a bone flap depending on the lost borders of the jaw bones with extensive and through defects in soft tissues. However, despite the technological advances in the field of plastic microsurgery, only a few reconstructive flap options have many unique advantages (technical simplicity, reliable axial blood supply, large size, subtlety and flexibility) that can ensure the closure of extensive and end-to-end head defects [3,4].Over the past few decades, several flap preparation options have been developed that further enhance its versatility. B.D. Bradford et al. pointed out that “a radiation flap offers a thin, supple skin-fascial flap, but the complication rate associated with microvascular anastomosis is high due to significant functional impairment when closing through face defects” [5]. According to RC Chan. et al. the use of a dentate musculocutaneous flap with extensive defects of the head showed good results, however, complications associated with the bulkiness of the flap and cosmetic discomfort were noted [6]. Another modification of the traditional technique for creating the flap is closed perforated and deltopectoral flaps, which allow performing simultaneous plastic surgery, provide a cosmetic result in both donor and recipient areas and avoid or at least minimize the complications associated with the graft engraftment [8].The literature data on the clinical experience of applying technologies in closure and extensive and end-to-end face and scalp defects indicate that various factors can contribute to unsatisfactory results, and opinions on the causes of complications are mixed. At the same time, there is no clearly formulated treatment strategy using the capabilities of flaps with an axial type of blood circulation, which dictates the need to continue studying this problem.
2. Material and Methods
- The foundation of this study was 40 patients with extensive and transverse face and scalp defects of various etiologies. The main group included 22 patients who underwent plastic surgery according to an improved methodology for preparing and closing defects with a fascial delto-pectoral flap. A comparison group consisted of 18 patients in whom the plasticity of these defects was carried out by free microsurgical flaps (fascial-fascial lower scapular flap on microvascular anastomoses and fascial-fascial thoracodorsal flap on microvascular anastomoses).In the comparison group, 18 patients with cicatricial deformities and defects in the facial area underwent autotransplantation of 18 soft tissue flaps (thoracodorsal flap n = 16 and scapular n = 2) on microvascular anastomoses. The microsurgery flap transplantation was performed in the following stages: preparation of the receptive bed and recipient vessels, sampling of a soft-tissue autograft, laying of the flap and its revascularization (formation of microvascular anastomoses).The surgery was performed by two teams. The preparation of the recipient bed consisted of a wide excision of the scarred tissue, isolation from the surrounding tissues and preparation for the anastomosis of the recipient artery and vein by dissecting them under an operating microscope. The collection of soft tissue microvascular flaps was carried out according to well-known methods of plastic microsurgery. For the formation of microvascular anastomoses, suture material Ethicon 8-0, 9-0, and an operating microscope Opton (Germany) were used.The adequacy of the blood supply to the transplanted flaps was monitored for 10 days - a period that is critical in terms of circulatory disorders and the development of thrombosis of microanastomoses.Radical excision of fibro-altered tissue in all cases led to exposure of the underlying structures (muscles, superficial vessels), that is, the defects in all cases were deep. This was one of the indications of using an adequately circulated graft to replace the defect. The lack of effect from the use of traditional plastic methods, the nature of the scar and the extent of the defect were also indications for the use of microsurgical free flaps.Arterial microanastomoses were formed by traditional methods (“end to end” - n = 15, or “end to side” - n = 3). An intravenous anastomosis was formed, almost always, of the end-to-end type (16 cases).Long-term results of plastic surgery were studied in all patients in the period from 1 to 5 years and were evaluated according to two main criteria: aesthetic and functional effects.The following complaints were referred to local functional disorders: salivation, chewing disorders, violation of the frame properties of the flap, local pain during movement (chewing, communication, facial expressions, etc.), limitation of the mobility of facial muscles.The problems of the aesthetic effect include: cicatricial deformity in the plastic area, unevenness of the soft tissue contour, the difference in the color of the skin of the flap from the surrounding tissues.A good result was characterized by the absence of complaints from patients on the specified criteria. If there was only an aesthetic defect and only one manifestation of a functional problem, the result was regarded as satisfactory. The result with the presence of several functional defects or their combination with a rough local deformation was considered unsatisfactory.In assessing the immediate results of plastic surgery of extensive and transverse defects of the head, the main clinical criteria are: the dynamics of the pain syndrome, the dynamics of the inflammatory syndrome, the dynamics of the local temperature of the flap, the structure of the early postop-complications and especially the engraftment of the flap (primary and secondary engraftment, rejection).In our study, a modified questionnaire from the University of Michigan head and neck quality of life (UM-HNQOL).
3. Results
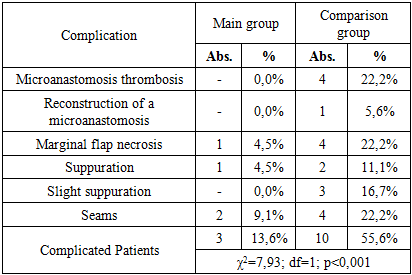
- When analyzing the resolution dynamics of the inflammatory syndrome (Fig. 1), its main signs were evaluated - hyperemia and edema. So, on the 3rd day after surgery, flap edema was noted in 8 (36.4%) cases in the main group, while in the comparison group this symptom of inflammation was more frequent and amounted to 10 (55.6%) cases. On the 7th day after surgery, flap edema persists in 7 (31.8%) patients of the main and 9 (50.0%) patients of the comparison group. Already on the 10th day, flap edema was noted in only 13.6% of cases in the main group and 38.9% of cases in the comparison group (p <0.05).
 | Figure 1. Dynamics of the inflammatory syndrome after surgery |
|
 | Figure 2. Flap engraftment features in the study groups |
 | Figure 3. Long-term outcomes in study groups |
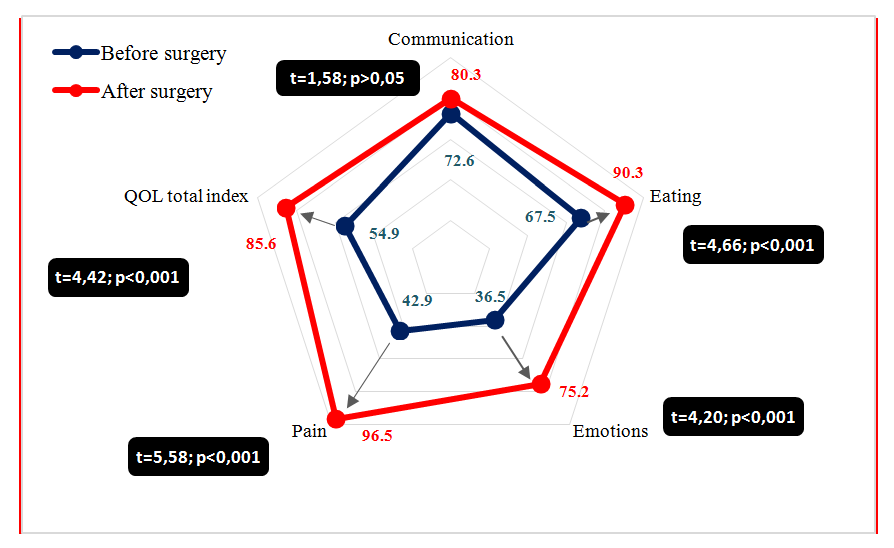 | Figure 4. Quality of life in the main group |
4. Conclusions
- The closure of extensive and through face and scalp defects with a delto-pectoral axial flap is a highly effective technique for reducing the incidence of postoperative complications associated with impaired graft trophy from 55.6% to 13,6% (p <0.001), flap engraftment in 100% cases, while in the comparison group this indicator was 83.3% (p=0,047).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML