-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(4): 246-257
doi:10.5923/j.ajmms.20201004.17

Designing Intelligent System for Stratification of COVID-19 Asymptomatic Patients
Mohamed Buheji 1, Abdul Rahman Buheji 2
1Founders of the International Inspiration Economy Project, Bahrain
2Arabian Gulf University, Bahrain
Correspondence to: Mohamed Buheji , Founders of the International Inspiration Economy Project, Bahrain.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The world is going through a life-threating, a war-like, virus attack called COVID-19. Since its inception in the last four months, it has been increased ten times every two weeks outside mainland China. In this case, we address this challenging human crisis with a focus on the early discovery of coronavirus asymptomatic patients which would help to reduce the cross-infection of COVID-19 that estimates to attack at least 60% of the world population, according to WHO (2020). This paper aims targets to raise the capacity of the health services authorities and help the community decision-maker to discover early asymptomatic and mild patients infected with COVID-19 by developing and applying intelligent decision-making protocol that would enhance the 'hit rate' of identifying and stratifying such cases. The paper has important implications of both the elimination of the COVID-19 and enhances the cost-effectiveness and the return of the efforts of the other isolation and quarantine measures taken all over the world.
Keywords: COVID-19 Coronavirus, Asymptomatic Patients, Symptomatic Patients, Infectious Diseases, Isolation and Quarantine, Inspiration Economy, Advanced Differential Diagnosis, Public Health, WHO
Cite this paper: Mohamed Buheji , Abdul Rahman Buheji , Designing Intelligent System for Stratification of COVID-19 Asymptomatic Patients, American Journal of Medicine and Medical Sciences, Vol. 10 No. 4, 2020, pp. 246-257. doi: 10.5923/j.ajmms.20201004.17.
Article Outline
1. Introduction
- This research reviews first the best practices followed by many countries and per WHO guideline to reduce or mitigate the impact of the coronavirus COVID-19. All the type of actions, community involvement, and what followed from aggressive public health actions, like social distancing and isolation of infected patients were reviewed. Nature (2020).However, as per the massive amount of information and publication that came since the beginning of the COVID-19; the body of knowledge seems to be missing a valuable perspective about addressing this human existence challenge from the total reliability preventive approach. As the cases from this pandemic outbreak spread all over the world, the catchment of the transmittance of the virus has proven to be the main challenge, Pappas (2020). Without identifying the transmitters of the COVID-19 with high availability, efficiency and effectiveness, the world would lose lots of people. It would a cycle of socio-economic crisis that might lead to deep recessions. Li et al. (2020).The literature reviews the description of COVID-19 infectious transmittance in general. Then, a general review of the available methodologies used to mitigate the threat of COVID-19 Pandemic is done. This review should help to realise the extent of the COVID-19 infectious challenge. CDC (2000b).Methodologies as community awareness and involvement, social distancing measures, cities or countries lockdown, utilisation of Apps and technology for codification and quarantine are briefly discussed. Even future coming methodologies as the early segregation of the vulnerable as the elderly or those with chronic illnesses are presented. The researcher presumes that there would be even soon more advanced screening that would help discover the mild cases. Finally, the author questions the cost-effectiveness of the mass screening as done by the Korean as a means for eliminating COVID-19 threat.The researcher then focusses on the importance of codification, classification and stratification of the asymptomatic individuals as a means for early eliminate COVID-19 and in a cost-effective means. Based on this review building an intelligent system that would help to discover early asymptomatic individuals would the target of this paper methodology. Rothe et al. (2020).
2. Literature Review
2.1. Description of COVID-19 Infectious Transmittance
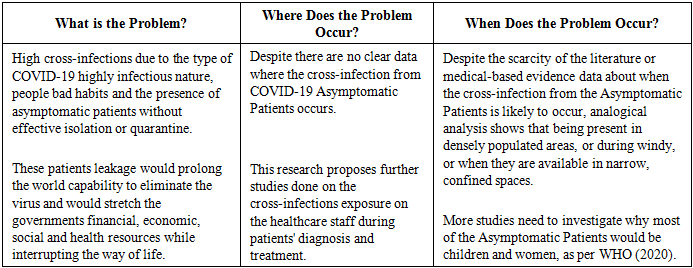
- COVID-19 is a novel pandemic highly infectious virus with no known pharmaceutical interventions, at the time of writing of this paper. This makes this coronavirus to be categorised as highly transmissible, WHO (2020). Both observed experience and emerging scientific evidence show that this coronavirus is easily transmitted from person to person and even from an animal to person, Huang and Wang (2020). The US Centres for Disease Control and Prevention (CDC) estimates that the virus's reproduction number (the number of additional cases that likely result from an initial case) is between 1.6 and 2.4, making COVID-19 significantly more transmissible than seasonal flu (which its reproduction number is estimated at 1.2 to 1.4). CDC (2000a, b), Zhu et. al (2020).More than ninety-seven countries have started 'community mitigation strategies' at the time of writing this research. All these measures target to help compensate the fierce attacks of the COVID-19 and a common method for intervention to slow the virus transmission, especially its impact on the respiratory infection. JHU (2020)The most hazard from COVID-19 infectious transmittance is the individuals with chronic diseases who come at increased risk from any severe illness. This includes older adults and persons of any age with underlying health conditions as those with Non-Communicable Diseases (NCDs). Yet, the world at the time of paper is already over-stretched and stressed on its healthcare and critical care infrastructure due to both the strength of the COVID-19 speed of infections and to low the impact of the mitigation efforts. During such complex Problem and global crisis, the need for re-inventing the way we do things is highly essential. Any innovative approach used to minimise morbidity and mortality would save thousands of lives and reduce the socio-economic impact of the COVID-19. Li et al. (2020), Buheji (2018).The challenge and complexity of COVID come from its ongoing speed of community transmission without detection of the source of infection. CDC (2000b) confirms that there is a sharp increase of confirmed cases of COVID-19 with no epidemiologic link to travellers or known cases, or more than three generations of transmission, Linton et al. (2020). This is going to hit hard on businesses, schools, and community organisations that need people around in order to survive. People would continue to have panic from COVID-19 or similar coming waves of such infectious viruses, unless innovative screening solution would help to exploit the sources of risks and contain them. Finding such a solution would minimise the disruptions to global development and growth or the daily life of the world.Figure (1) shows the infectious capacity of COVID-19, as illustrated by McKinsey, called the reproduction number. Currently COVID-19 infectious capacity is similar to SARS and MERS, which are viruses of the same family that came in the recent years; however, this novel coronavirus has a high probability of increasing its reproductive ration if not contained in the right time. Huang and Wang (2020), Zhu et al. (2020).
 | Figure (1). Illustrates the Infectious Capacity of COVID-19 |
2.2. Reviewing the Available Methodologies Used to Mitigate the Threat of COVID-19 Pandemic
2.2.1. Understanding the Extent of the COVID-19 Infectious Challenge
- The way the virus works is not known so far, despite many theories. However, almost all scientists and medical practitioners, especially those who were and maybe still are in the front line see the COVID-19 moves slow at the beginning with a long incubation period, then have a quick attack. If this is true, then it is expected to have at least three types of patients or virus carriers: asymptomatic, mild symptomatic and severe symptomatic. Lauer et al. (2000).When one person gets a confirmed diagnosis, they are usually put in isolation, hoping they won't spread the disease further. Then their contacts can be identified and put into quarantine. But what about the those who are asymptomatic or those who seem to spread the COVID-19 before they show any symptoms, or when their symptoms are mild. Azad (2020).Hence, the challenge of the whole world is how to reduce the ratio of transmittance of the COVID-19 infected patient from 3 victims or more to less than one victim. This seems to be a target that is very hard with having many asymptomatic that cannot be identified by the current methodologies.
2.2.2. Community Awareness and Involvement
- One of the main benefits of the COVID-19 Pandemic is that it forced many governments to be transparent, or at least to show respect to its community citizens. The communication model for many countries followed WHO emergency preparedness plans, where the media kept the people to be part of the solution not part of the problem. The civil society played a significant role in advising proper hygiene like hand washing, reducing unnecessary travel movements and not overburdening the health systems. The involvement of the citizens created a combination of top-down policies and bottom-up commitment from ordinary people to fight the spread of the virus. Nature (2020).
2.2.3. Effectiveness for Social Distancing Measures
- Despite social distancing was used as the primary method for mitigating the threat of COVID-19 since its inception in December 2019, starting from China and then to most of the world countries; WHO emphasised later this measure is not going to stop the Pandemic. WHO said later that this type of self-isolation is only a technique to give the healthcare workers to manage the flow of cases. Fleming (2020).Many governments have taken necessary measures that support social distancing as encouraging people to work from home, closing schools and prohibiting large gatherings.
2.2.4. Lockdown as a Solution
- One of the most stringent solutions taken by humanity in recent history is the lockdown Wuhan and other 15 cities in Hubei province which the Chinese government taken to mitigate the threat of the COVID-19, the last week of January 2020, Huang and Wang (2020). Even though this measure, as we write this paper in March, i.e. after less than six weeks from the lockdown, seems to have worked and the number of COVID-19 reported cases reduced drastically; this cannot be the model for a permanent solution for a developing world. CDC (2000b).The lockdown model also cannot be followed by every country who do not have both the human resources and the financial resources as China. The Chinese manage to draft the healthcare workers from all over China and where hospitals were built in just a week. Repeatedly shutting down public services as transports, schools, businesses, etc. for more than one week might create disruptions and crisis more the COVID-19. Hence, this cannot be considered to be a solution model that could be generalised for a world under more immediate threats. Fleming (2020).
2.2.5. Utilisation of Apps and Technology
- Chinese used a form of people codification in the latest Wuhan crisis. This codification was facilitated by the authorities and leading popular social platforms; we chat besides other apps, Huang and Wang (2020). The apps helped to monitor the movement, through colour codes, of those that should be allowed to pass to a particular area. Again, this approach seemed to have helped the Chinese to restrain the movement of the people and thus reducing the transmission rate. Fleming (2020), Li et al. (2020).
2.2.6. Guarantee of Quarantine
- Recent research suggests that even though the quarantine helped to give confidence to the governments and the people about the active catchment for those infected with COVID-19, there is still no guarantee that those recovered may not acquire the virus again.The best successful quarantine besides China was Singapore which supported its quarantine with tracking points for access and departure. Citizens who returned to Singapore from affected countries were immediately placed under quarantine conditions. Those who do not give accurate information would be fined.
2.2.7. Segregating the Elderly
- The reports coming from analysing more than 72,000 of COVID-19 infected cases in China confirms that the virus disproportionately affects older people with underlying conditions and especially the elderly. The current fatality rate for 70- and 80-years old patients found to be consequently four and seven times the average. JHU (2020).Despite no measures taken by any country regarding segregating the elderly, except preventing visitors from nursing homes, as USA did in March 2020, there are no other clear efforts in this area. This mitigation technique might help reduce the morbidity to one of the threatened categories of the population, however again its does not contribute to detect and eliminate the virus. CDC (2000a).
2.2.8. Detect Milder Cases
- One of the hidden mysteries of COVID-19 is the extent of undetected milder cases. Knowing how to deal with this mysterious characteristic will affect how the disease progresses, and its socio-economic scenarios in the future. Linton et al. (2020).As a respect to the human advancement in technology, one could expect that in few months we would see requirements that would help to detect the milder cases faster and would help the healthcare workers be confident about this decision. Still, as of the time of this paper, this is not available as an option.
2.2.9. Cost-Effectiveness of Mass Population Screening of COVID-19
- Resnick and Scott (2020) illustrated how the US has been extremely slow in releasing the diagnostic tests for the Covid-19 disease. The problem seems to come from the combination of manufacturing problems, chronic underfunding, and an apparent lack of foresight, as per Resnick and Scott. With the unfolding of much public health crisis as COVID-19, there needs to be an overall evaluation about the cost-effectiveness of the mass population screening and whether it would help the country or the community to be more prepared? So far, at the time of writing this paper, this no 100% accurate testing that could help in stopping the cross-infection of this deadly outbreak. Pappas (2020).The South Korean approach of mass testing of about 140,000 people has, of course, its advantages, but again doesn't guarantee that the COVID-19 is over and that there are no infected people, it only mitigates the risk through speeding up the catchment of those need to be self-isolated or quarantined.The Korean method is not affordable for many developing countries, and in short, it is not cost-effective.
2.2.10. Possibility of Getting Infected After the Screening
- Beuesekom (2020) mentioned about the possibility to test positive after proven to test negative. He said about specific incidences in China that shows that people might be re-infected, or that in certain times the screening doesn't help. Beuesekom mentioned about the real-time reverse transcriptase-polymerase chain reaction (RT-PCR) tests can show the results 5 to 13 days later. Although screening might help to segregate the positive from the negative tested individuals, the test results only mean that the virus is present or was present a day or two before. However, such screening is less useful for telling us whether someone is contagious, or not. The positive result due to screening doesn't differentiate between a patient that is a carrier or having only viral genomic material without any infectious virus, or being genuinely contagious. Beuesekom (2020) confirms that testing positive in a nucleic acid-based test does not mean that the person is still shedding contagious virus.
2.3. The Challenge of the COVID-19 Tricky Incubation Period
- Studies now confirm that COVID-19 can have a tricky incubation period, where the people may be able to spread the virus before symptoms appear or without feeling ill at all, Lauer et al. (2020). Both the USA Centres for Disease Control (CDC) and the WHO now confirms that coronavirus infections can be asymptomatic, and the CDC says the role of pre-symptomatic transmission "is unknown." Lessler et al. (2009).Azad (2020) reported after Hanage, a Harvard University epidemiologist, that the confusions caused by the COVID-19 make the individuals act as transmitters of the virus before they are aware of their infectious destruction to the community around them. This, of course, raises the panic and the unambiguity in dealing with such Pandemic. Li et al. (2020).Individual researchers now see the challenge of COVID-19 is extending to be more of 'cryptic transmission' and this even raise the threats of this disease dynamics. Due to an increase of the asymptomatic coronavirus infected individuals, the period between reported infections and going into being the emergency case are also becoming very short enough. Azad (2020).
2.4. Impact of the Asymptomatics on the Pandemic
2.4.1. Defining Risks of Asymptomatics
- A pandemic cannot be eliminated as long as there is a loophole in the comprehensive efforts of reducing the COVID-19 infectious ration and capacity. This seems to be challenging at the moment since when individuals become asymptomatic for a specific viral disease, they may become a source of shedding and transmitting the virus without knowing or feeling ill. This becomes more of a community and global risk with a fierce illness as COVID-19, which is very infectious and life-threatening. Rothe et al. (2020).The evidence is mixed about whether asymptomatic people can transmit the virus, and about the length of the incubation period, Lauer et al. (2020). If the asymptomatic transfer is a significant driver of the Pandemic, then different public-health measures will be needed. Lessler et al. (2009).Infection with the COVID-19, found to cause severe acute respiratory cases. Similar to SARS, this coronavirus can be asymptomatic or can result in mild to severe symptomatic signs. This level of uncertainty is not covered in literature, and the body of knowledge has a shortage of addressing this critical gap for the worse pandemic virus in the last century. Rothe et al. (2020). Lately, a USA leading medical experts emphasised to CNN reporter that they are not clear what is the level of the transmissions happening by those who have no symptoms or very mild symptoms. Cohen (2020).Pappas (2020) emphasised that more data on mild and asymptomatic cases is desperately needed regarding defining 'how many cases are asymptomatic, versus mild, moderate or severe?' Not having an accurate figure for the total asymptomatic and symptomatic patients makes forecasting the disease severity, besides its morbidity and mortality rate to be not precise. Wu et al. (2020).US Secretary of Health and Human Services, on an interview on 1 March that asymptomatics are not the major drivers and that the containment strategy depends on focusing the symptomatic patients of the spread of the new coronavirus. Missing to account for asymptomatic patients would hinder building accurate knowledge about the total number of cases that could be estimated to become severely ill or die. This accuracy might make lots of difference to the current world panic about the COVID-19, which is reported to have a fatality rate of less than 2.5%. Once mild and asymptomatic cases are identified and are included as part of the total virus victims, then the number if the mortality would drop much further, which make the threat of the virus a bit near the danger of the seasonal flu. Cohen (2020).
2.4.2. Identifying COVID-19 Asymptomatics as a Complex Problem
- We can't start any complex problem solving without understanding the essence of the threat it represents and visualising the hidden opportunities it carries. Realising the amount of cross-infection all over the world from the COVID-19, despite the high precautions of the people and community, shows there are a niche and a gap that need to be addressed to minimise the lobe hole of the public health system, despite the increase of the awareness and alert of the public.Cohen (2020) reported about 82 cases coronavirus outbreak in Massachusetts started by people who were not yet showing symptoms. More than half a dozen studies have shown that people without symptoms are causing substantial amounts of infection.Bill Gates (2020) sees that the spread of the coronavirus disease by people who haven't yet developed symptoms, or who are only a bit sick means that COVID-19 will be much harder to contain than the Middle East respiratory syndrome (MERS), or the severe acute respiratory syndrome (SARS), which were spread much less efficiently and only by symptomatic people. This challenge has a significant impact on the efforts of screening, identification and also minimisation of threats of the COVID-19, or even mitigation of the risks as a result of consequences that could come from the panic that speed and the throughput of such virus could cause to the world economy and socio-economy. Solving such a problem also would help the stretched emergency healthcare services resources in the future. It would even contain having as many patients reaching the intensive care units (ICUs), or reaching too late for ventilation. CDC (2000b).
2.4.3. COVID-19 Threat on Asymptomatic Patients
- Guan et al. (2020) reported as a team of Guangzhou Institute of Respiratory Disease in China that 1.4% of the deaths of the COVID-19 patients for the total 1,099 patients' medical records from 522 hospitals in 30 Chinese provinces had a median age of 47 years and showed no fever or radiographic abnormalities. The study was carried from December 2019 to Jan 29. The none availability of fever or radiologic abnormalities makes increases the complexity of the COVID-19. JHU (2020).Moss et al. (2020) reported the UK's first patients did not meet testing criteria in describing how their country's first two COVID-19 patients tested positive for the virus even though they didn't meet current case definitions.The patients were identified as at-risk while still in the community and transported from their hotel to the university hospital, where they were tested.Cohen (2020) reported after Dr Deborah Birx, the USA administration's coronavirus response coordinator, saying in the second week of March 2020, that now they are trying to understand people under the age of 20 who don't have potentially asymptomatic or significant symptoms to be source for spreading the virus. In another report to CNN, the director of the Center for Infectious Disease Research and Policy at the University of Minnesota confirms that asymptomatic transmission cross-infections surely can fuel the COVID pandemic and make it very difficult to control. The threat is even more substantial as countries keep receiving travellers. CNN study shows that passengers are testing positive for coronavirus even though they have no symptoms. In other studies where the Viral load was measured to see the concentration of the virus in the respiratory secretions, the viral load of the specimens from the asymptomatic patients was higher than the viral load of the samples from the three patients who did have symptoms. This means that the asymptomatic patients have chances to spread the infection to others than the symptomatic patients. Cohen (2020).
3. Methodology
- Based on the literature review, identification of the COVID-19 asymptomatic patients become the primary research aim, which has the objective of designing an intelligence system that helps the decision-makers take effective, comprehensive decisions regarding the threat of such life-threatening virus. The COVID-19 asymptomatic problem is fully described in the case presented. A study of the attitudes and the history of symptomatic and asymptomatic COVID-19 patients is done to help discover the later type. The case shows how this problem is being analysed through both convergent and divergent thinking approaches and which we call it Advanced Differential Diagnosis, which is a technique developed by the author, Buheji (2018). Then, the proposed intelligence system for mitigating the risk of COVID-19 asymptomatic patients' is linked to stages of codification, classification and stratification of the asymptomatic individuals. These efforts should help to raise the capacity of the practitioners for reducing the COVID-19 problem's complexity which would help to establish asymptomatic intelligence program.
4. Case Problem Solving
4.1. Designing the Intelligence System for COVID-19 Asymptomatic Inputs
- In order to outline the asymptomatic infected patients' problem, we need to start codifying the type of patients or victims of COVID-19. Then, we can classify the categories of the type of patients or victims of COVID-19 in terms of place, time, type of area, the way infected and detected. Specifying the relation and the correlation between symptomatic and asymptomatic patients (both from an analysis of previous history and field observations).The researchers used the potential sources of risks for COVID-19 to emphasis the application of the intelligence program proposed represented in a table. The proposed Table would use the CDC (2020b) reference for controlling the level of community transmission. The weightage of each factor would be taken into account the number and the type of outbreaks reported in the accommodation and the area. Wong et al. (2020).The Table would also include the demographics that are causing an impact on the critical care infrastructure or services. The size of the community in relevant to its habitat characteristics and surroundings would have a weightage in the intelligent system. The other important variables in the intelligent system are the size of the community and the population density. Finally, the system table should preferably include the size of the vulnerable population.
4.2. Studying Attitudes and History of Symptomatic and Asymptomatic COVID-19 Patients
- Without understanding the attitudes both symptomatic and asymptomatic COVID-19 patients, we can't solve problems. Thus, here we need to identify the types of hygiene, self-isolation, emergency readiness attitudes (both in the symptomatic and asymptomatic patients).Then we need to dig into the history of the length of time taken to reach an emergency for some of the infected patients, similar to Guan et al. (2020). Understanding all the challenges in compacting the threat of asymptomatic patients as regards the type of accommodation, social boundary areas, and age are also significant.
4.3. The Challenge of Containing the COVID-19 Pandemic using Convergent and Divergent Thinking Approaches
- In order to start reasoning of the COVID-19 asymptomatic patients' threat, the research applies both convergent and divergent thinking to see the type and amount of cross infections in relevance to the level of type accommodation and the size of the population in a specific area. Thus, the reasoning could be used to re-engineer the process of screening of the patients to enhance the capacity of response health staff and medical teams. This focused reasoning would help to remove the non-value-added steps.
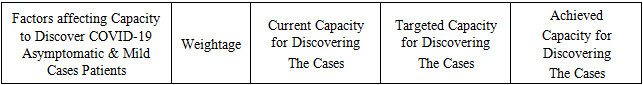
4.4. Establishing the basis of the COVID-19 Asymptomatic Intelligence Program
- Building the base of the COVID-19 Asymptomatic Patients Intelligence Program (APIA) would enhance the health authorities to a proactive response to any potential coronavirus cross-infection with high availability, better efficiency, and more effectively. The presence of APIA would help the decision-makers to apply the most suitable 'Mitigation of Risks Programme' (MRP).As shown in Table (1), APIA needs could be addressed by the following basic questions: what is the problem of a priority now, where does the problem occur and when does the problem occur. Answering these questions would help the healthcare professionals and the decision-makers setup specific MRP suitable to the needs of the community.
|
4.5. Importance of Codification of Individuals being Asymptomatic to Other Diseases
- In order to enhance the detection individuals prone to be asymptomatic for future infectious disease, the medical files need to be codified for those that would experience such history, so that they could be called for screening early in the stages of any pandemic.
4.6. Reducing the Problem's Complexity
- We need to continue to reduce the problem complexity in order to create more resilience, tolerance and enhance our capacity to reduce COVID-19 victims. The effective detection of asymptomatic patients would help to speed up the response of the emergency team.We can start simplifying the problem by understanding the places where cross-infection occurs inside the accommodations and then study the trends or the repetitions in terms of these cross-infections and where, when they occurred.
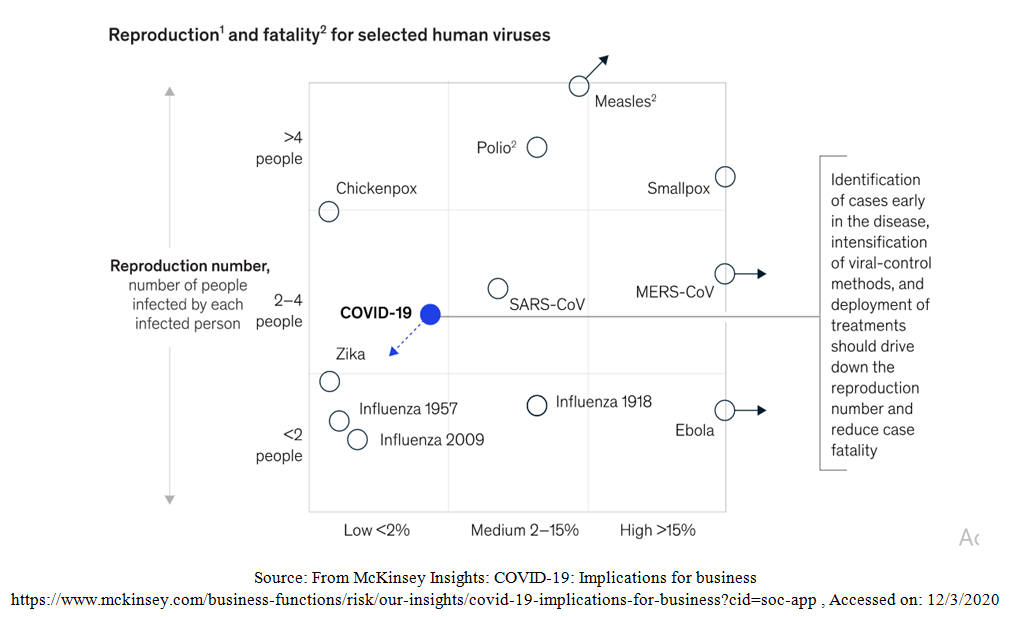
4.7. Re-phrasing the Problem
- To solve a complex problem, we need to re-phrase it, by first categorising the type of COVID-19 asymptomatic patients' and then designing specific protocols that can be both flexible yet robust. As a result of re-statement and defining the magnitude of the re-phrasing the problem and curves we can re-invent and re-design specifically where screening needs to be more emphasised, or where quarantine need to be stronger. Many international researchers found that infection is being transmitted on average 2.55 days and 2.89 days before symptoms. Tindale et al. (2020). Hence, the proper phrasing of the problem is “how to discover COVID-19 asymptomatic patients before they infect others, taking that they are on the move and dynamic. i.e. define the intelligence system needed or meet the demand and the threats of the COVID-19; according to the maturity and latest incidences analysis. Then, we should start a codification of the possible COVID-19 asymptomatics to mitigate the risk of having the health system to be fatigued due to being stretched in resources for long-time due to the hidden sources of cross-infection. One of the techniques here is that we should replace specific words in the problem statement with a substitute needs a pre-requisite work that explicitly defines the reframed problem. This means we should try reverse-thinking in rephrasing the problem statement. Or restarting the problem with positives instead of negatives, Beuesekom (2020). Figure (2) shows that once the problem issues are defined, its situation and possible ideas and opportunities can be precisely evaluated. Based on this, the problem can be re-defined.
 | Figure (2). Cycle of Stating and Defining the Problem |
4.8. Exploring Steps towards COVID-19 Asymptomatic Patients' Knowledge-Based System
- Building a knowledge-based system helps the healthcare leaders and decision leaders to forecast and precisely predicts where the asymptomatic are causing cross-infections. Wu et al. (2020) The knowledge-based system starts with exploring the field and seeing how the issue is currently handled and then design disruptive alternatives that can be tested again. The renowned psychology professor George Loewenstein sees that this requires a curiosity that joins the focused mental state besides the emotions that push us until we complete gaps in our knowledge.
4.8.1. Codifying COVID-19 Asymptomatic Patients
- The first exploration journey towards building the knowledge-based system is to collect and study all the observations on the COVID-19 asymptomatic patients' and specify the pathways that would help to triage, or capture, or codify them. Since this first identification step might be complex, the 'rate of cross-infection' within a specific area or accommodation need to be investigated and then considered as part of the codification. The types of COVID-19 patients demographics and the type of populations not included in the earlier demographics, need then to be categorised. Here, it might be an opportunity to identify the non-value-added steps, i.e. those steps not helping the public health professional to determine the patients. Then, we need to try to codify any none symptomatic patients. The outcome of this exploration should help to address the essence of codifying COVID-19 asymptomatic patients. This is done through a troubleshooting codification exploratory journey, as shown in Figure (3).
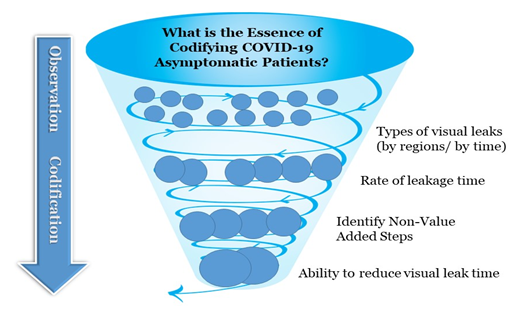 | Figure (3). Illustrates Example the Codification of COVID-19 asymptomatic patients' Exploratory Journey |
4.8.2. Classifying COVID-19 Asymptomatic Patients
- The second journey to build up the knowledge base from the classifying of the COVID-19 asymptomatic patients. Here, it is good to start with taxonomies-based questions to reduce the ambiguity about such type of patients. Then, inquiries and investigations screening should be The focused approach should be designed, based on the developments of experimentation for the type COVID-19 asymptomatic patients proposed. This would be the start of classifying such type of patients. Then more focus and selective screening inquiries and investigations would be done based on this classification. This investigation would conclude to assessment and deployment of self-isolation and/or quarantine of the classified COVID-19 asymptomatic patients. Figure (4) shows the COVID-19 asymptomatic patients' classification journey.
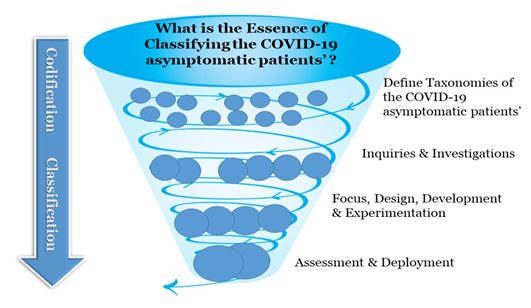 | Figure (4). Illustrates the Classification of COVID-19 Asymptomatic Patients Exploration Journey |
4.8.3. Stratifying COVID-19 Asymptomatic Patients
- As we arrive into the third exploratory journey, the focus here would be a viable solution that would help to finalise the establishment of the knowledge-based system that would help in the stratification of COVID-19 asymptomatic patients till they are either self-isolate or be quarantined. Hence, this is the stage where the threads towards absorbing the knowledge about COVID-19 asymptomatic patients. In this stage, more profound vital signs of the asymptomatic patients would be assessment and deployment of testing the models would be defined to ensure that the asymptomatics are stratified regardless of the different areas and conditions. Figure (5) shows the entire third exploration journey applied until the establishment of the knowledge base, which we'll call the COVID-19 asymptomatic patients' intelligent system.
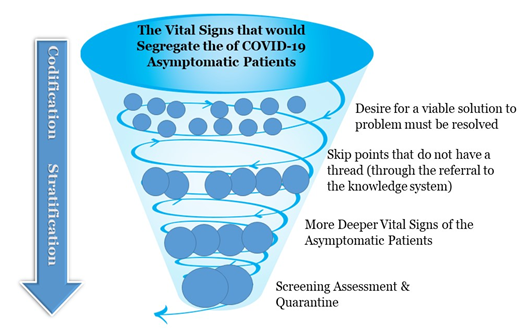 | Figure (5). Illustrates Exploration towards Stratification of COVID-19 Asymptomatic Patients |
5. Analysis of the Case
5.1. Importance of this Study
- Building a more intelligent system to identify COVID-19 asymptomatic patients would re-build the trust of the community, establish confidence to sustaining social life, community bonding and reduce the level of panic. The study would also reduce the level of irrational behaviours due to the level of uncertainty, ensure effective social isolation in the right time and most of all reduce potential inequality or stigma against a specific type of nationalities where countries were hit by COVID-19 most. Ultimately this study would reduce the negative spillovers on the already constrained stretched economy and healthcare services.
5.2. Managing the 'Availability Bias'
- One of the challenges towards adopting the proposed COVID-19 asymptomatic patients' intelligent system is the 'availability bias' amongst the over-stretched healthcare workers who all their attention now is directed towards screening, detecting and quarantining those identified with COVID-19 or coming countries with the Pandemic. Buheji (2018).In order to give more focus on asymptomatic patients, the intelligent knowledge-based system needs to be tested.
5.3. The Classical Solution to Such Problem
- The classical solution to deal with the similar life-threating viral outbreak is to follow a robust public-health response. The Chinese followed this classical model affectively, followed by Singapore, and Hong Kong. Such measure can't be followed by many developed, or cannot be followed drastically for a long time from all the countries of the world; otherwise, it would have a devastating effect on the economy and even the social stability. Pappas (2020).
5.4. The New Proposed Solution for COVID-19
- The newly proposed solution should help in minimising the time, the efforts and the risks of not identifying patients or populations that are causing cross-infection without being in social isolation or quarantine. The proposed intelligent system could enhance the ability of the healthcare workers to discover early the COVID-19 asymptomatic patients pull thinking, i.e. selective screening through more focused observations that leads consequently to codification, classification and stratification. The intelligence on the proposed system comes from its capacity in raising the healthcare staff and public health decision-makers opportunities to mitigate and manage or control the potential threats of the asymptomatic patients and thus more containing the spread of the COVID-19. The early identification of the asymptomatic patients' targets to raise the level of knowledge that has accumulated from the different experiential learning that is collected from the three explorations journeys. The outcome of these journeys should help to raise the observations, the absorptions and the reflections that could support the COVID-19 pandemic containment decision-makers all over the world, starting with the healthcare workers.
5.5. The Constructs of the COVID-19 Asymptomatic Patients Intelligent System
- The constructs of the intelligent knowledge-based COVID-19 asymptomatic patients system comes from the advanced differential diagnosis technique developed by the research through a tool called problem vectors, Buheji (2018). In this case, the problem vectors are made of three vectors, or variables, which are represented in Figure (6) that are important towards an effective exploiting of the infected COVID-19 asymptomatic patients. As shown in Figure (5), the first vector is about the intelligent prediction of COVID-19 asymptomatic patients. The second vector is about realising the amount and the resources lost in relevance to COVID-19 elimination due to low availability of other types of difficult to identify patients. The third vector is about the innovation to improve the detection of the asymptomatic patients in relevance to symptomatic patients in specific demographics or areas or time. Buheji (2018).
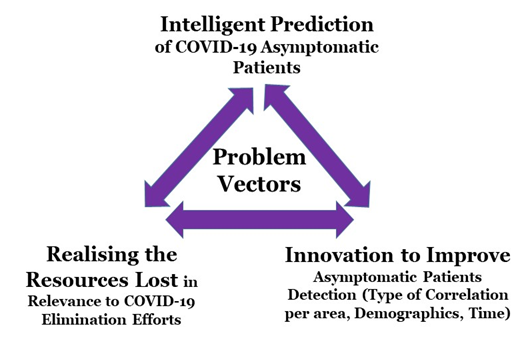 | Figure (6). Illustrates the Problem Vectors of Identification of COVID-19 Asymptomatic Patients |
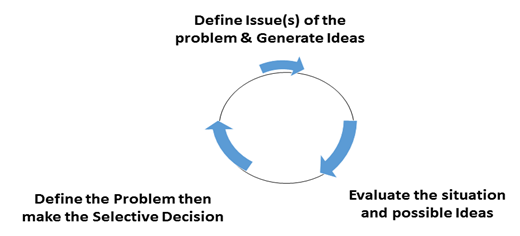
5.6. Applying the Intelligence System of Mitigating COVID-19 Asymptomatic Patients'
- As mentioned in the literature review and the case presented the purpose of the COVID-19 asymptomatic patients' intelligence program (APIA) is to help the decision-makers to apply the most suitable 'Mitigation of Risks Programme' (MRP). To apply a sample of the proposed intelligent system that following Table (1) is set to help the decision-makers and healthcare professional develop their hit rate and availability of discovering the asymptomatic and mild cases as early as possible. The first column has the main factors affecting the capacity to discover COVID-19 asymptomatic and mild cases of patients. Each of these factors would have a weightage value depending on its impact on eliminating or its probability for spreading the virus. The other three columns in Table (2) are meant to visualise and then realise the effect of the discovery and the mitigation achievement for COVID-19 asymptomatic and mild patients. First, the current capacity for discovering the cases is evaluated. Then the targeted and the achieved or realised capacity for discovering asymptomatic patients are entered.
|
6. Discussion & Conclusions
6.1. Framework Proposed for Discovering Presymptomatic Transmissions for COVID-19 and Similar Threats
- Cohen (2020) reported about the analysis of Caroline Colijn team who is doing mathematical model, genomics to create the predictions of COVID-19 infection at Simon Fraser University in British Columbia, emphasising that presymptomatic transmissions are highly one of the main causes for the spread of this highly infectious virus. When we have a dilemma of not knowing how to totally meet a certain demand as this; it might be time to change from the capital-based economy of (supply vs demand) to another formula. In Inspiration Economy, we developed a formula that raises the capacity; focus on emphasising the relation of (Capacity vs Demand), Buheji (2016). In order to set a practical holistic and comprehensive approach for eliminating the COVID-19 threat through a community mitigation program, using the earlier formula, a framework was proposed. The framework supports risk assessment and intelligent decision making for the countries.The purpose of the framework is to establish a COVID-19 knowledge system that lead to a COVID-19 intelligence system, where the decision-makers and healthcare professional can depend on when making decisions related to the individuals or the mass in relevance to screening and testing. Both the symptomatic and asymptomatic patients would be or might be exposed to one or more of the following pathways or protocols: self-isolation, clinical isolation, quarantine, and ambulatory care services. The framework emphasis that we should not leave anyone behind, i.e. to strengthen the efforts for effective decision making in relevance to saving lives and eliminating global threatening viruses, as the COVID-19.
6.2. Piloting the Investigation in the Field
- Since now, and as reported by Cohen of CNN at the time of submitting this paper, there are confirmed reports coming from different countries of significant transmission by people who are asymptomatic or only mildly symptomatic, the researchers believe that it is about time to speed up the testing of the proposed framework and intelligence system.The investigation for COVID-19 asymptomatic patients should start with piloting the framework proposed in Figure (7) in relevance to the different demographics and areas as mentioned the intelligence system and represented by Table (1). This should also be linked to observing the attitudes emergency cases identified who did not contact any symptomatic, or self-isolated, or quarantined individuals.
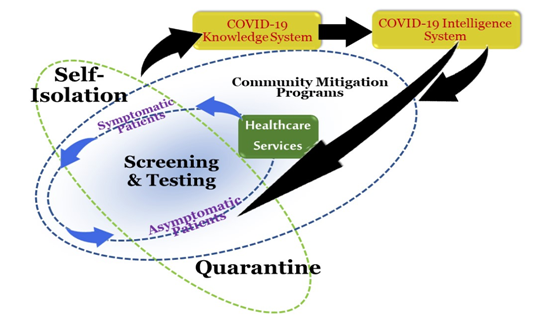 | Figure (7). Framework Proposed for Comprehensive COVID-19 Community Mitigation Programs |
6.3. Implications and Limitation of the Study
- Recent large-scale studies using mathematical modelling of outbreaks in Tianjin, China, and Singapore in January and February show significant amounts of spread by people who no developed symptoms. The statistics, as per the studies reviewed by CNN, the infections from someone who was pre-symptomatic ranges between 48% and 77%. Hence, this shows the importance of this study and the viability of its approach.This research is also essential for elderly patients, or those with chronic diseases, or respiratory issues. Also, it is highly necessary for densely populated areas, or communities with high population density. In order to ensure the generalisation of this study, more longitudinal study research is recommended. Also, more medical and clinical diagnosis supported by immunologist experts might be carried for selected asymptomatic patients stratified by as per the intelligent system. This can be done through more screening or utilisation of RT-PCR viral genomic tests or more advanced kits.
6.4. Final Recommendations
- It is highly recommended that future research continue in this line both for the asymptomatic and mild cases in all the virus-related diseases. The practice of troubleshooting a problem rather than describing its, or constraining it, or mitigating it, or preventing it needs to be embedded in the mindsets of both the healthcare professional and the national emergency response teams. This type of mindset can save lives with minimal resources and could lead a new breakthrough in the future foresighted changes in the public health services after the elimination of COVID-19 outbreak.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML