-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 0(4): 233-235
doi:10.5923/j.ajmms.20201004.14

Hemodynamic Disorders in the Eye Vessels and Their Correction in Children with Chronic Glomerulonephritis
Karimjanova N. I.
Tashkent Institute of Postgraduate Medical Education
Correspondence to: Karimjanova N. I., Tashkent Institute of Postgraduate Medical Education.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

There were examined 59 sick children with chronic glomerulonephritis (CGN). All patients underwent ultrasound dopplerography of eye and kidney vessels. Hemodynamic disorders in the form of reduced blood flow rates and resistance of blood vessels were found in 94.9% of the patients. Standard therapy (ST) of CGN in children does not lead to normalization of hemodynamic disorders. Inclusion of chophytol preparation in ST CGN in 93% of cases promotes normalization of blood circulation disorders in the eyes and kidneys.
Keywords: Doppler, Eyes, Kidneys, Chronic glomerulonephritis, Chophytol
Cite this paper: Karimjanova N. I., Hemodynamic Disorders in the Eye Vessels and Their Correction in Children with Chronic Glomerulonephritis, American Journal of Medicine and Medical Sciences, Vol. 0 No. 4, 2020, pp. 233-235. doi: 10.5923/j.ajmms.20201004.14.
1. Introduction
- Kidney disease in children is a pressing problem of pediatrics. Chronic glomerulonephritis (CGN) often leads to the development of chronic renal failure. [4,5]. Distinguish from mechanisms of progressing of CGN immune (the damages of nefron induced immune) and not immune (haemo dynamic, connected with the system and glomerular hypertensia, metabolic, caused by the violation of fatty exchange [2,4,6]. It is known that the rate of progression of chronic kidney diseases is also influenced by proteinuria [3,7]. It has been established that increased passage of protein through tangles exacerbates glomerulosclerosis, leads to disorders of hemodynamics, tubulointerstitial sclerosis due to damage of proximal canals in case of increased protein reabsorption. Cytokines stimulating inflammation in kidney tubulointersion followed by sclerosis are released [3,12]. Often in such patients, the functions of various organs, including organs of vision, are impaired [1,14].There are known methods of pathogenetic therapy which promote stopping and slowing down, reverse the development of processes in kidneys, eyes and other organs. Glucocorticosteroids, cytostatics, antiaggregants, hypotensive and hypolipidemic drugs [5,7,11,13] are among such means. In recent years there have been clinical studies in cardiology, gastroenterology, neonatology, nephrology about the positive effect of chophytol on hemodynamics, protein and nitrogen metabolism [10].However, the works devoted to studying of chophytol preparation influence on the hemodynamics of eye vessels in children with CGN have not been found in the literature available to us, which was the basis for the current research.The work aimed to estimate the influence of chophytol preparation on eye vessel hemodynamics in children with chronic glomerulonephritis.
2. Research Materials and Methods
- 59 children with chronic nephrotic glomerulonephritis who were undergoing inpatient treatment at the 1st clinic of the Tashkent Medical Academy were examined, 37 (62.7%) of boys and 22 (37.3%) of girls aged 7-14 years. The duration of the disease was 1-3 years in 23 children, 4-5 years in 24.5 years and more in 12 years. The diagnosis was based on anamnesis and the results of clinical and laboratory tests. The classification adopted at the International Symposium of Pediatricians and Petrologists (Vinnitsa, 1976) was used for diagnostics.All patients were studied generally accepted in nephrological practice: general urine analysis, Zimnitsky's and Reberg's samples, measurement of daily diuresis, blood pressure, biochemical studies (urea, creatinine, total protein and its fraction), kidney ultrasound; functional state of the kidneys was assessed by the level of residual nitrogen in the blood serum, the rate of ball filtration, concentration ability of kidneys, proteinuria. The state of blood circulation of both eyes was determined by ultrasound Doppler ultrasound on PHILIPS HD 11X. Maximal systolic speed (Vmax) and final diastolic speed (Vmin), resistance index (Ri) were studied. Biomicroscopy of the anterior and posterior eye regions was performed on Karl Zeis. Visual acuity was determined using Snellen tables, eye bottom condition was determined by ophthalmoscopy. Patients were divided into two groups - with chronic glomerulonephritis with preserved kidney function (CGNPKF) and disturbed kidney function (CGNDKF). The group of patients with CGNDKF included children with oliguria, proteinuria, high content of urea and creatinine, decreased rate of ball filtration.29 sick children received standard therapy (CT) of CGN (glucocorticosteroids, curantils, heparin, diuretics, cytostatics and symptomatic agents), 30 patients received chophytol (CT + chophytol) along with standard therapy.
3. Results and Discussion
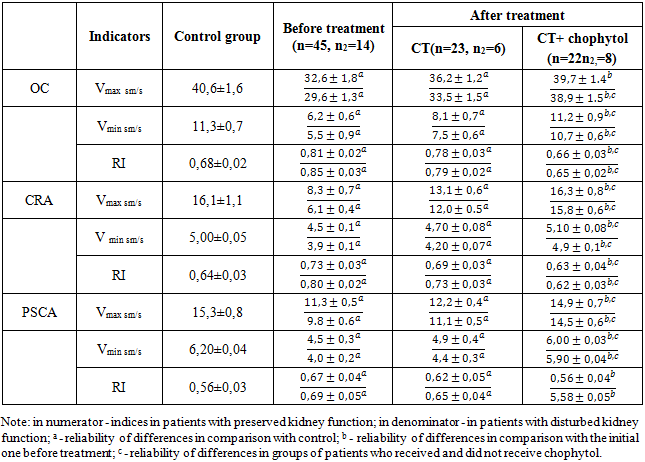
- The study of hemodynamics parameters in ocular vessels showed that in 56 (94,9%) patients with chronic glomerulonephritis a decrease of Vmax and Vmin was established at the level of ocular artery (OA), central retinal artery (CRA) and posterior short ciliary artery (PSCA) (P<0,05) before treatment with simultaneous increase of Pi(P<0,05). Violations of blood flow velocities and vascular resistance were more pronounced in the group of patients with CGNDKF (P<0,05), which seems to be associated with a significant number of patients with CGN with more than 5 years of experience in this group (Table 1). This indicates a significant complication of the blood flow in the blood vessels of the eye and explains the vascular side of the pathogenesis of changes in the structures of the eye bottom. The obtained results are consistent with the research data on the development of retinopathy, nephropathy, cardiopathy, and lesion of brain vessels exactly from the periphery, in the course of microcirculation [5].
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML