D. A. Alimov, S. N. Salakhitdinov, B. S. Alimkhanov, S. A. Akilova
Republican Scientific Center of Emergency Medical Help
Correspondence to: D. A. Alimov, Republican Scientific Center of Emergency Medical Help.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The objective: In the article we reviewed characteristics and frequency of cardiac rhythm disorders, safety of electrical coagulation performance in mono polar mode during various non-cardiological surgical interventions in patients with earlier implanted electrical cardiac stimulators (ECS). Data and research methods: We studied the factors most often leading to disorders in the operation of ECS during non-cardiological surgical interventions in various terms after implantation of the stimulator in 56 patients in the age from 53 to 84 years old in the units of general surgery, traumatology, and vascular surgery of the RSCEMH. Besides that, measures for the prevention of these disorders were observed. Cardiac activity during surgical interventions was assessed with the help of cardiomonitor. Results: In 8.9% of the patients we registered dysfunction of ECS such as ineffective stimulation, stimulus inhibition, and temporary change in the stimulation mode. Conclusions: The study showed, that application of electric coagulation in mono polar mode was the most often cause of intra operative complications linked with the work of ECS and duration of a single impact of electric coagulator within different surgical operations.
Keywords:
Coagulation mono polar mode, Continuous electric cardiac stimulation, Electric coagulation, Cardiac rhythm disorders
Cite this paper: D. A. Alimov, S. N. Salakhitdinov, B. S. Alimkhanov, S. A. Akilova, The Impact of Electrical Coagulation on the Operation of ECS in Patients with Acute Pathologies in Abdominal Cavity, American Journal of Medicine and Medical Sciences, Vol. 10 No. 4, 2020, pp. 187-191. doi: 10.5923/j.ajmms.20201004.02.
Disorders of rhythm and heart conductibility take the 4th place in the structure of cardiac vascular pathologies. In the modern time the basic method in the therapy of chronic bradyrhythmia is still implantation of a permanent electric cardiac stimulator (ECS). Implementation of ECS implantation into clinical practice significantly increased expectancy and improved quality of life of the patients with symptomic bradycardia. Within the last decade the range of indications to ECS implantation increased, due to which the number of patients with implanted artificial pace maker increased too [1,2].Among the patients applying for emergency and planned operations in abdominal cavity the portion of those with previously implanted ESC is equal to 1-2% [3]. There is data about successful surgical operations in patients with ECS [4-6]. The main reason for surgeons and anesthesiologists worries performing surgical interventions is the risk of ECS dysfunction development. In the foreign literature there is data about disorders in ECS work appearing in cases when during surgical interventions electric coagulation is used. Though the character, prevalence, danger, prevention methods, and treatment of possible complications of these disorders are rarely described in detail [1-7]. The objective of the research was to study the impact of electric coagulation on the function of cardiac stimulator during abdominal surgical operations in patients with acute pathologies in abdominal cavity with previously implanted electric cardiac stimulators (ECS).
1. Data and Research Methods
In the RSCEMH within the period from 2015 to 2018 fifty-six surgical interventions were performed in the patients with various forms of acute abdominal pathologies with previously implanted artificial pace makers. The age of those patients varies from 53 to 84 years old, average 63.9±14.6 years old. There were 35 (55%) men and 25 (44%) women. Among the concomitant diseases 35.71% (20 patients) were taken by diabetes mellitus, 57.14% (32 patients) by arterial hypertension, 66.07% (37 patients) angina, and 50.0% (28 patients) by cardiac failure. For the assessment of cardiac activity during operations all patients had a record of electrocardiogram (ECG) on cardiomonitor with evaluation of the indicators of ECS operation during mono polar mode electric coagulation (EC). For the analysis of possible damaging effect of EC on cardiac tissue in the endocardial electrode fixation area 13 patients had tests of cardiotropic enzymes amount and assessment of ECG dynamic alterations at the 1st and 3rd days after the surgery. In all the cases during operations mono polar mode EC was used with 100 W capacity.
2. Discussion and Results of the Research
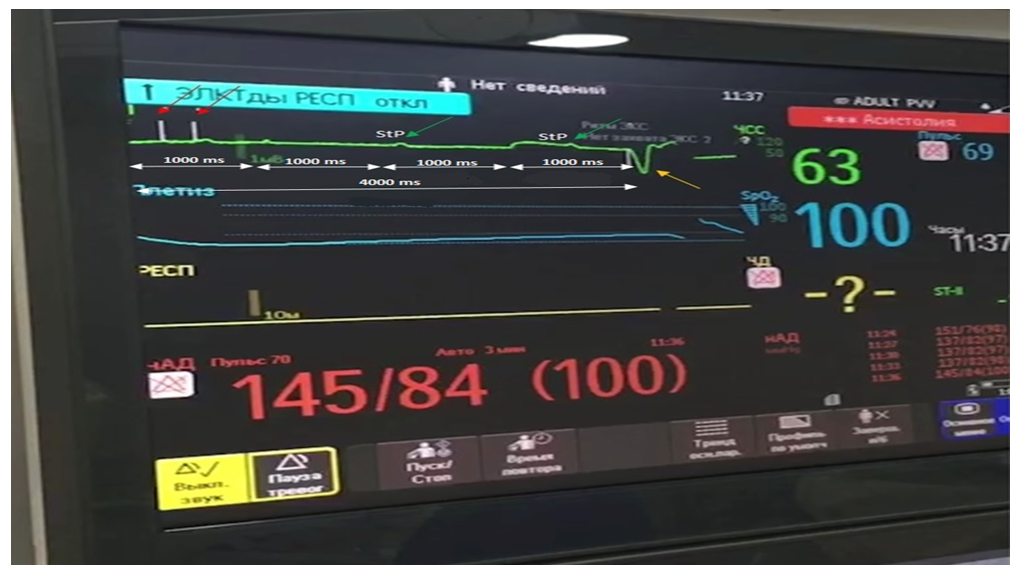
All (100%) patients had successful emergency surgical operations without intra operation lethal outcome. In spite of the following all the safety rules some patients had registered ECS dysfunctions when electric coagulator was used. In two (3.6%) patients EC impact on ECS work was accompanied by periodic absence of stimuli at the moment of electric coagulation (figure 1).With the help of cardiomonitor with separated channel for the stimulator analysis and Medronic – a device programming cardiac stimulating coagulation in five (8.9%) cases we registered the following interactions of coagulator with cardiac stimulator. During EC two patients (3.6%) had ECS dysfunction, accompanied by temporary asystole (figure 1,2).In the photo №1 there is a part of cardiomonitor record where we can see that at the moment mono polar mode electric coagulation impact, indicated as Mm, there is registered asystolia of ventricles (4000ms-15imp/min) (intervals are indicated by a dotted arrow).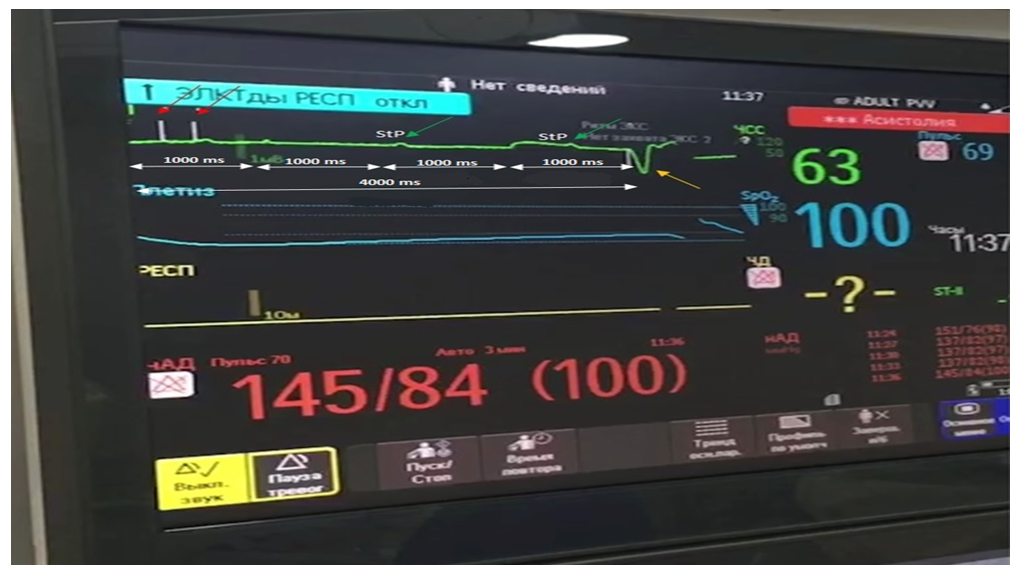 | Photo 1. Intra operation cardiomonitor. Biventricular mode of stimulation (DDD) with basic stimulation frequency equal to 60 imp/min at the moment of EC. Record speed is 50mm/sec, amplification 1mV = 10mm (explanation herein) |
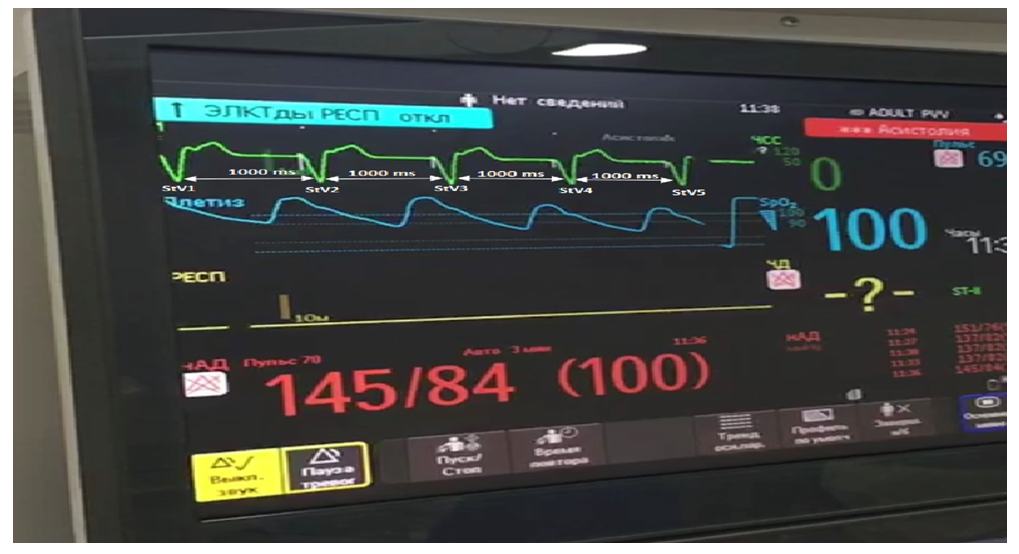
Application of EC led to disorder of ECS function in more than 4 cardiac stimulation cycles (original duration of cardiac stimulation cycle was equal to 1000 ms or 60 imp/min. red arrow shows cardiac stimulator impulses without ventricular response. There is no ventricular stimulus for more than 4000 ms. Green arrow shows (StP) atrial proper stimulations without ventricular myocardium response. After a long pause a yellow arrow shows an effective stimulation V with ventricular coverage. Record speed is 5-mm/sec, amplification is 1mV = 10 mm.In the photo №2 there is a part of cardiomonitor record after EC application. Biventricular mode of stimulation (DDD) with basic stimulation frequency equal to 60 imp/min. Stimuli are bipolar: StV - ventricles. 4 ventricular stimuli (V1, V2, V3, V4) are effective, causing ventricular myocardium response displayed in the registration of wide artificial ventricular complexes manifested by a complete block of the left bundle branch. There is notable complete recovery of ECS work. 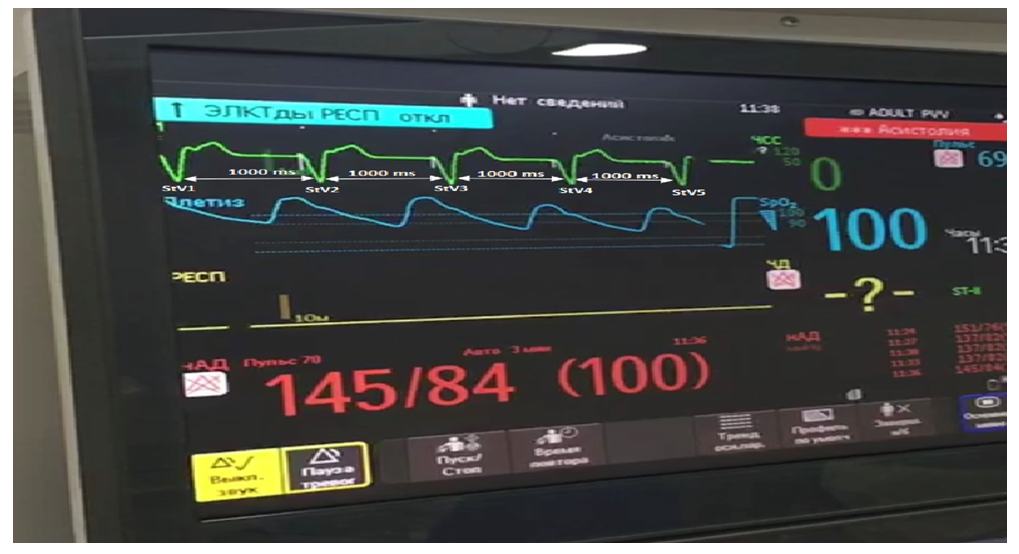 | Photo 2. Intra operation cardiomonitor. Double-chamber mode of stimulation (DDD) with basic stimulation frequency equal to 60 imp/min after EC. Record speed is 50mm/sec, amplification is 1mV = 10 mm (explanation herein) |
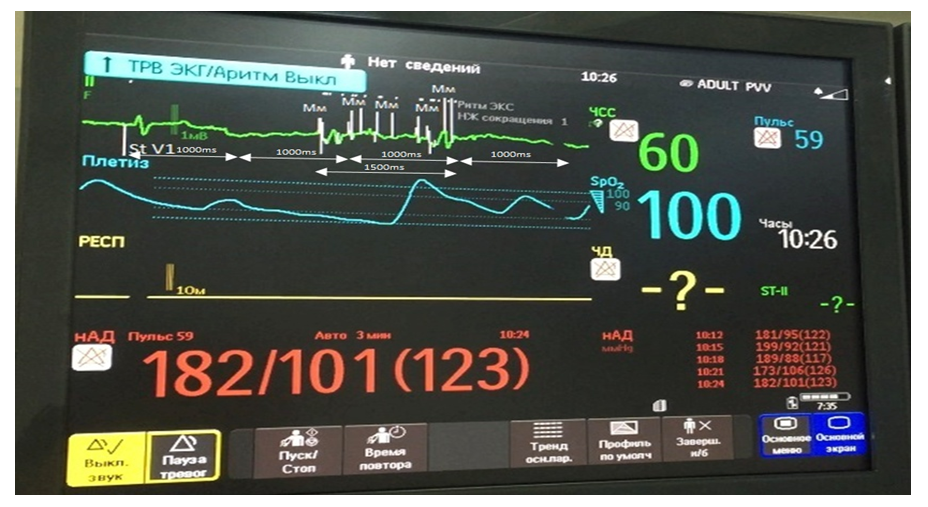
Thus, application of EC caused ineffective stimulation along the ventricular channel and a short-term asystole in ventricles. When a patient has a rhythm below a programmed basic stimulation interval, we could observe the pattern presented in the photo №1.In three patients (5.3%) at the moment of mono polar EC application we registered singular ineffective ECS stimuli (photo № 3).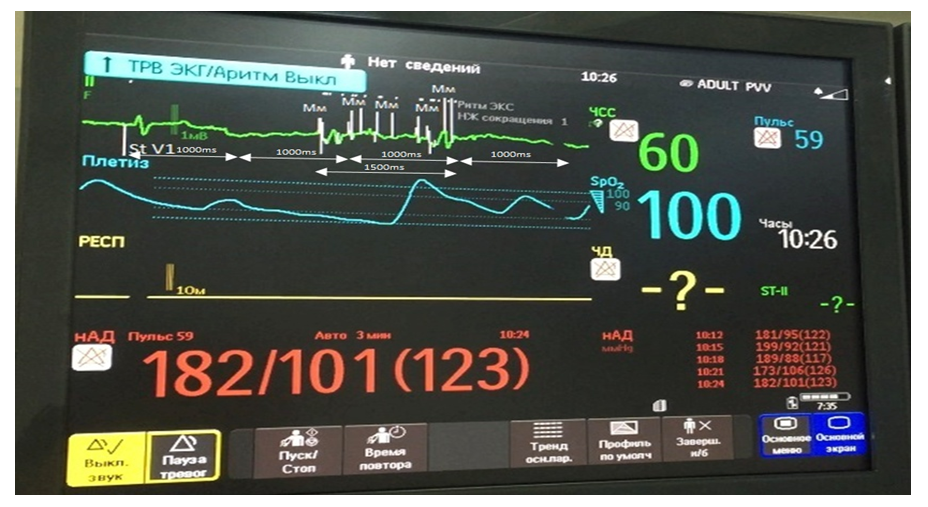 | Photo 3. Intra operation cardiomonitor. Double chamber stimulation mode (DDD) with basic stimulation frequency equal to 60 imp/min at the moment of EC application. Record speed is 50mm/sec, amplification is 1 mV = 10 mm (explanation is hereafter) |
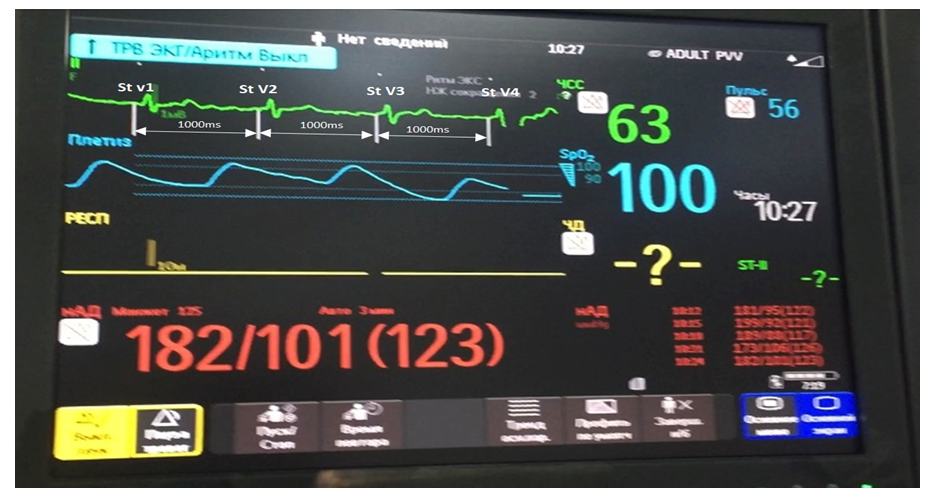
In the photo №3 there is a part of cardiomonitor record showing StV1- the first effective ventricular stimulation, causing ventricular myocardium response. After a short-term electric coagulation impact we registered low and high amplitude “pseudo stimuli”, which were multi-range noise interferences coming from EC. Interferences coming from electric coagulator were perceived by ECS as ventricular myocardium contractions. That is why there was no stimulation. 1500ms pause indicates the absence of effective excitement in myocardium. After effective stimulation StV1 of ventricles, we registered the first and the last stimulation of ventricles, which did not lead to myocardial excitement, as there was EC impact. In the photo №4 there is double chamber stimulation mode (DDD). StV1-StV4 are effective ventricular stimuli. Basic stimulation interval determined according to the length of the intervals StV-StV, was equal to 1000ms (60 b/min). In the continuous record of ECS after EC application we registered recovery of ECS operation.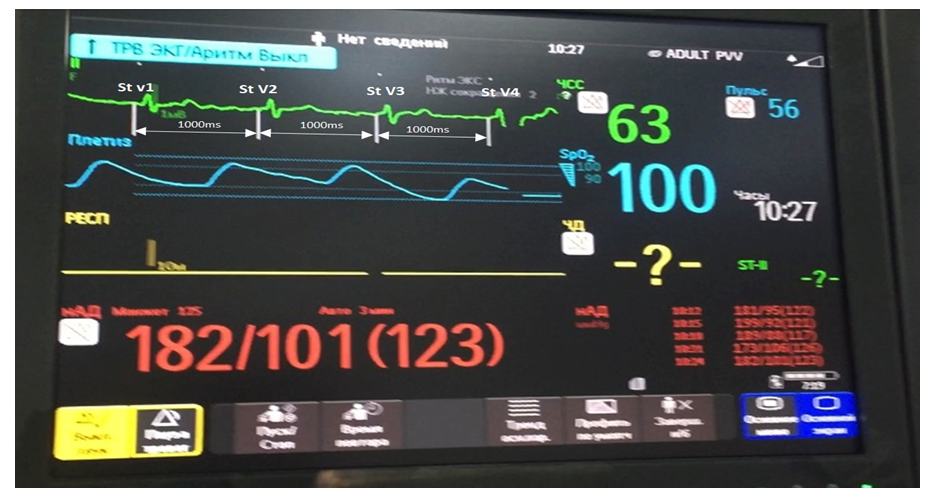 | Photo 4. Intra operative cardiomonitor. Double chamber stimulation mode (DDD) with basic stimulation frequency equal to 60 imp/min after EC application. Record speed is 5-mm/sec, amplification is 1 mV = 10 mm (explanation is hereafter) |
EC impact caused not only ineffective stimulation along the ventricular channel, but also a short-term disorder in synchronization. Dynamic control testing of ECS system within post operative period did not reveal any alterations neither in amplitude-time parameters of stimulation, nor in previously programmed ECS functions; that confirms the dependence of these disorders on EC.During surgical operations we had no situations requiring resuscitation and interventions to ECS system due to its dysfunction. Post operative lethality rate was equal to 1.7% and was not dependent on ECS dysfunction. Characteristic feature of new ECS models is capability to perceive electric impulses of heart, and when the heart beat rate is above a programmed one ECS stops generating impulses, working in a “waiting” mode. External electromagnetic EC impulses, especially those in mono polar mode, can be perceived and wrongly detected by ECS to be a high heart rate, which leads to inhibition of stimulation till the end of EC [6,8,9,7]. Re-programming of ECS sensitivity from mono to bipolar one, and increase of its absolute indicator provide decrease of the ECS impulse perception degree. It was determined that, in bipolar mode sensitivity ECS is the least exposed to external electric impacts. Thus, disorder dynamic registered in two patients according to the term of appearance is not dangerous in any group of patients. Nevertheless, it is impossible to exclude temperature impact on cardiac tissue in the area of ECS electrode attachment at the moment of registration of that disorder [6]. So, in case of the registration of ineffective stimuli the further application of EC should be stopped. A surgeon and anesthesiologist should be informed about the basic parameters programmed for a certain patient and be ready for possible alterations on electrocardiogram [10]. Assessment of preoperative ECS testing provides information about the model, characteristics of the program, and stimulation parameters. Besides that, we assessed proper cardiac rhythm, probable alterations in ECS sensitivity to external impacts. If necessary, correction of stimulation parameters was performed. Basic functions of stimulation system testing prior to surgery:1. Assessment of basic stimulation parameters of ventricular myocardium: mode (AAI, VVI, DDD, etc.), amplitude, impulse time, stimulation threshold, stimulating impulse and perceived impulse polarity, magnetic test frequency, battery and electrodes condition.2. Alterations in ECS program for the purpose of inclusion of the functions, which can change normal stimulation mode at the time of certain stages of surgical operation: switching off the sensor functions, automatic definition of stimulation threshold, sleeping function, frequency hysteresis.3. Correction of the program, which serves to prevent development of disorders in stimulation system: re-programming of atrial/ventricular sensitivity from mono to bipolar (most models). 4. Setting of individual protective functions. For example, for prevention of SVT conduction to ventricles, inclusion of AMS.5. In cases when disorders are revealed to make a decision about necessity of surgical revision and correction of stimulation system. On the basis of the results of our study and data from literature we tried to make a system of ECS operating disorders, which could appear in EC interaction with cardiac stimulator during surgical interventions.
3. Conclusions
Presence of ECS is not a counter-indication for the performance of surgery using electric coagulation in mono polar mode. Though 8.9% of the patients had development of disorders in ECS system such as stimuli inhibition, ineffective stimulation, and temporary alteration of stimulation mode. Stimulator-dependent patients should be operated with EC in conditions of specialized clinic due to minimal risk of ECS damage. The most often disorder developing under the influence of mono polar electric coagulation was ECS stimulus inhibition, appearance of which depended on the cardiac stimulator’s sensitivity polarity configuration. To diminish the risk of development of the aforesaid disorder it is rational to use bipolar mode sensitivity of electric cardiac stimulator. That disorder is dangerous in the group of stimulator-dependent patients. Short-term episodes of ineffective stimulation at the moment of electric coagulation are not so dangerous as rhythm disorders. In all cases of ECS operation disorders development short-term stop in electric coagulation should be done; in case of ineffective stimuli registration surgeons should quit EC application. The term of single electric coagulation application during operation in any patient with cardiac stimulator should not exceed 3 seconds. ECG characteristics in the work of electric cardiac stimulator can be registered independently of electric coagulation, set basic stimulation frequency, hysteresis function and other settings (including those due to myopotential inhibition). That is why during preoperative examination of a patient control testing of ECS system, and, if necessary, performance of special tests for the detection of these characteristics, should be done.
References
| [1] | Bazayev V.A. Electrocardiography in electrocardiostimulation of heart [Elektrokardiografiyaprielektrokardiostimulyatsiiserdtsa] // Functional diagnostics in cardiology. V2 Bokeria, Y.Z. Golukhova, A.V. Ivanitski publ. M. SCCVP under the name of Bakulev A.N. of the RAMS, 2002. V.1. p.311-333. (in Russian) |
| [2] | Bokerya L.A., Retishvili A.S., Stupakov I.N., Samorodskay I.V. Organizatuion of medical help to patients with disorders of heartbeat rate [Organizatsiyameditsinskoypomoshibolnimsnarusheniyamiritmaserdtsa] // Quality Clinical Practice. 2003. № 1. p.75-82. (in Russian) |
| [3] | Bokerya L.A., Retishvili A.S., Dubrovski I.A. Electric coagulation in Russia in 2006 [Sostoyaniyeelektrokoagulatsiivrossiivdvetisyachishestomgodu], Elect. Libr. Available from URL: http://www.electrophysiology.ru/library/article.php?new_article_id=23, free. (18.01.2008). |
| [4] | Grigorov S.S., Votchal F.B., Kostilyova O.V. Electrocardiogram with artificial pace maker [Elecktrokardiogrammapriiskustvennomvoditeleritma]. M: Medicine, 1990. p 240. (in Russian) |
| [5] | Day monitoring complex of ECS automated «Astrocard® - Holter analysis» (Astrocard® - Holtersystem-2F for Windows). Passport. Moscow. Meditech. 1996. p. 39. |
| [6] | Kostileva O.V., Vitchal F.B., Morgunov V.S. Guideline on application of implanted electric cardiac stimulators ECS-511 and ECS-530. [Rukovodstrvopoprimeneniyuimplantiruemikhelektrokardiostimulyatorovecc511iecs530], Tver, Gubernian medicine, 1999. p. 32. (in Russian) |
| [7] | Wilson S., Neustein S.N., Camunas J. etal. Rapidven-tricularpacingduetoelectrocautery: a casereportandre-view. // MtSinai J Med. 2006; 73(6): 880-883. |
| [8] | Manual. Propgrammer APSµ model 3250 with 3264а software. APSµ model 3251 base with 3265 software version. Sylmar, USA: St.JudeMedical; 1999. Apraxia; p. 148 (translated). |
| [9] | Salukhe T. V., Dob D., Sutton R. et all. Pacemakers and defi brillators: anaesthetic implications. // British Jour-nal of Anaesthesia. 2004; 93 (1): 95-104. |
| [10] | Shibata Hil-oshi, Yano M., Okahisa T.et al. Effects of High-frequency Current on Pacemakers during Endo-scopic Gastric Surgery: Experimental Study. // Digestive Endoscopy 1999; 11: 150 - 157. |
| [11] | Caramella J.P., Aliot E., Claude E. et al. Anesthesia and cardiac pacing. // Ann Fr Anesth Reanim. 1988; 7(4): 309-319. |
| [12] | Chauvin M., Crenner F., Brechenmacher C. et al. In vi-tro study of the effects of high frequency electrical current on cardiac pacemakers. // Ann Fr Anesth Reanim.1990; 83 (7): 997-1002. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML