-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(3): 166-174
doi:10.5923/j.ajmms.20201003.08

The Features of Liver Perfusion in Various Hepatic Diseases and Portal Hypertension According to Data of Multidetector Computed Tomography
Babadjanov A. Kh., Djurayeva N. M., Amirkhamzayev A. T.
Republican Specialized Scientific-Practical Medical Center of Surgery named after academician V.Vakhidov, Tashkent, Uzbekistan
Correspondence to: Amirkhamzayev A. T., Republican Specialized Scientific-Practical Medical Center of Surgery named after academician V.Vakhidov, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Perfusion computed tomography has a great potential for determining hepatic and portal blood flow; it offers the advantages of quantitative determination of lesion hemodynamics, distinguishing malignant and benign processes. Many studies have reported the use of this method in the assessment of hepatic fibrosis and hepatic perfusion changes associated with chronic liver disease (liver cirrhosis, liver fibrosis, portal hypertension). The main goal of liver perfusion imaging is to improve the accuracy in the characterization of liver disorders. In this study, we tried to identify the features of liver perfusion in various hepatic diseases and portal hypertension according to data of multidetector computed tomography. The study included three groups: blocking the intrahepatic postsinusoidal circulation - 63 patients with cirrhosis; blocking the intrahepatic presinusoidal circulation - 10 patients with liver fibrosis; blocking the subhepatic circulation - 13 patients with extrahepatic portal hypertension. And 24 healthy people were included to analyze the nature of changes in perfusion indicators relative to normal values. The study included the determination of liver perfusion parameters such as arterial fraction, portal fraction and portal index.
Keywords: Liver cirrhosis, Liver fibrosis, Portal hypertension, Perfusion CT-imaging of the liver
Cite this paper: Babadjanov A. Kh., Djurayeva N. M., Amirkhamzayev A. T., The Features of Liver Perfusion in Various Hepatic Diseases and Portal Hypertension According to Data of Multidetector Computed Tomography, American Journal of Medicine and Medical Sciences, Vol. 10 No. 3, 2020, pp. 166-174. doi: 10.5923/j.ajmms.20201003.08.
1. Introduction
- Hemodynamics disorders in liver cirrhosis (LC) affect all the main criteria for the severity and prognosis of the pathological process. Timely identification of the development of functional and hemodynamic complications of LC affects the choice of optimal treatment tactics and, accordingly, the duration of its effectiveness. The degree of impaired intrahepatic circulation affects the functional status of hepatocytes, respectively; the state of perfusion of the liver will affect the effectiveness and long-term hepatoprotective therapy [1-3]. Decrease in liver perfusion and progression of impaired liver function leads to the development of decompensation of cirrhosis and the solution of the issue of radical treatment - liver transplantation [4,5]. The features of hemodynamic rearrangement affect the severity of portal hypertension (PH) and, accordingly, the frequency of complications such as variceal bleeding, splenomegaly and hypersplenism, the vascular component of ascites syndrome [6]. Compensated indicators of hepatic perfusion expand the choice of surgical methods for the prevention of gastrointestinal bleeding. The newest and most promising options for studying the features of intrahepatic hemodynamics is perfusion computed tomography (CT-perfusion). There are limited number of scientific studies in this direction, as well as the existence of controversial issues about the effectiveness of perfusion CT-imaging of the liver to verify specific criteria for assessing the LC severity and its complications [7,8].The objective of this study was to determine the features of liver perfusion in various hepatic diseases and portal hypertension according to data of multidetector computed tomography.
2. Material and Methods
- The research was conducted at the Republican Specialized Scientific-Practical Medical Center of Surgery named after academician V.Vakhidov (Tashkent, Uzbekistan). The study was conducted in 110 patients aged 18 to 67 years with various liver diseases and included three groups taking into account the level of the blocking the portal circulation: - blocking the intrahepatic postsinusoidal circulation - 63 patients with LC, - blocking the intrahepatic presinusoidal circulation - 10 patients with liver fibrosis (LF) - blocking the subhepatic circulation - 13 patients with extrahepatic PH (EPH). Also, 24 healthy people were included (fourth group) to analyze the nature of changes in perfusion indicators relative to normal values.We used a multidetector CT “Aquilion One - 640” of the GENESIS version (Canon Medical Systems, Japan). The study included the determination of liver perfusion parameters: - arterial fraction (AF), - portal fraction (PF), - portal index (PI). These data were studied in all liver anatomical segments - at 8 points. That is, for 110 studied, 880 indicators of AF (ml/100 ml/min), PF (ml/100 ml/min) and PI (%) were obtained. The statistical data included for each indicator the determination of the average value (M), standard deviation (σ). Reliability calculation was carried out according to the definition of Student’s t-test.
3. Results
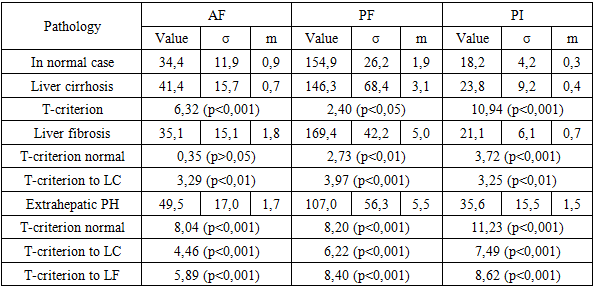
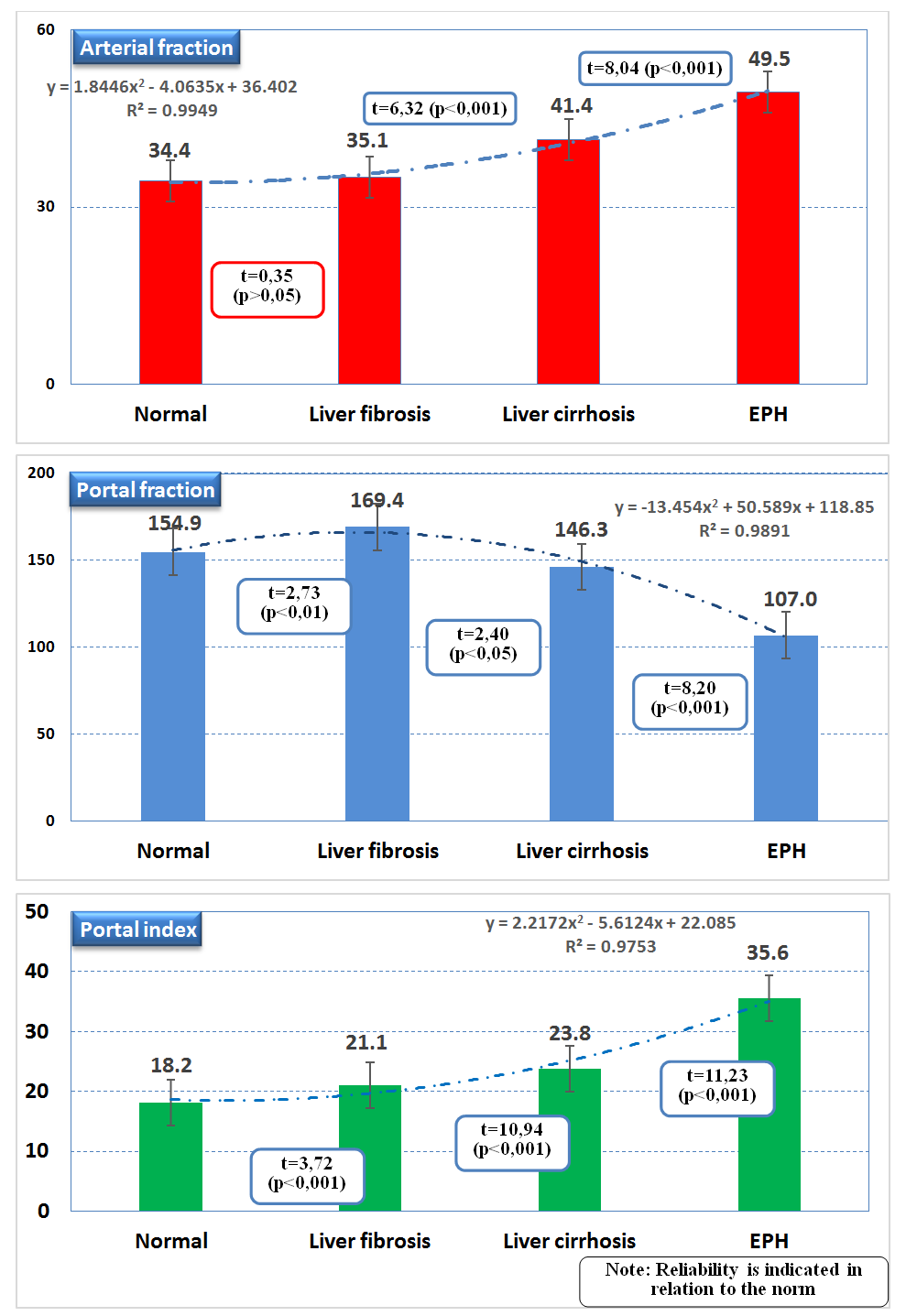
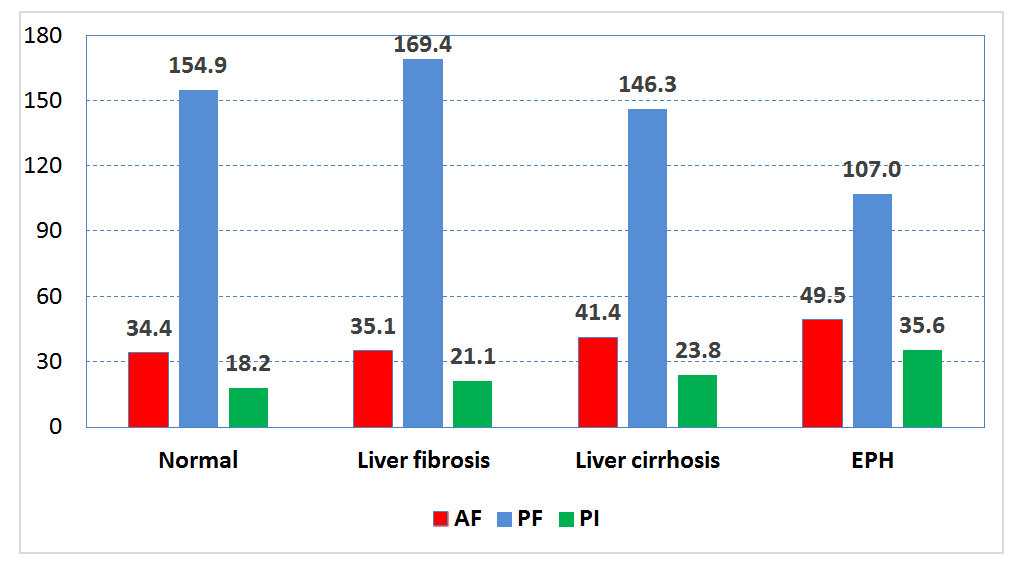
- The perfusion values for any variation of blocking the portal circulation were significantly different from those in healthy group, with the exception of only the AF in LF. In case of LC the PF decreased from 154.9±1.9 ml/100 ml/min (normal values) to 146.3±3.1 ml/100 ml/min (p<0.05). In case of EPH the PF decreased from 154.9±1.9 ml/100 ml/min (normal values) to 107,0±5.5 ml/100 ml/min (p<0.001). In case of LF the PF was significantly higher than the norm - 169.4±5.0 ml/100 ml/min (p<0.01).Correspondingly, a decrease in portal blood flow showed a compensatory increasing in the AF - from 34.4±0.9 (the norm) to 41.4±0.7 ml/100 ml/min in patients with LC (p<0.001) and to 49.5±1.7 ml/100 ml/min (p<0.001) for EPH (table 1). The obtained values (fig. 1) of the liver perfusion fractions showed a high degree of linear relationship of the features of changes in the intrahepatic blood flow at various etiology of PH in relation to the norm.
|
 | Figure 1. Indicators of perfusion CT imaging of the liver |
 | Figure 2. Summary of liver perfusion CT scores depending on the cause of portal hypertension |
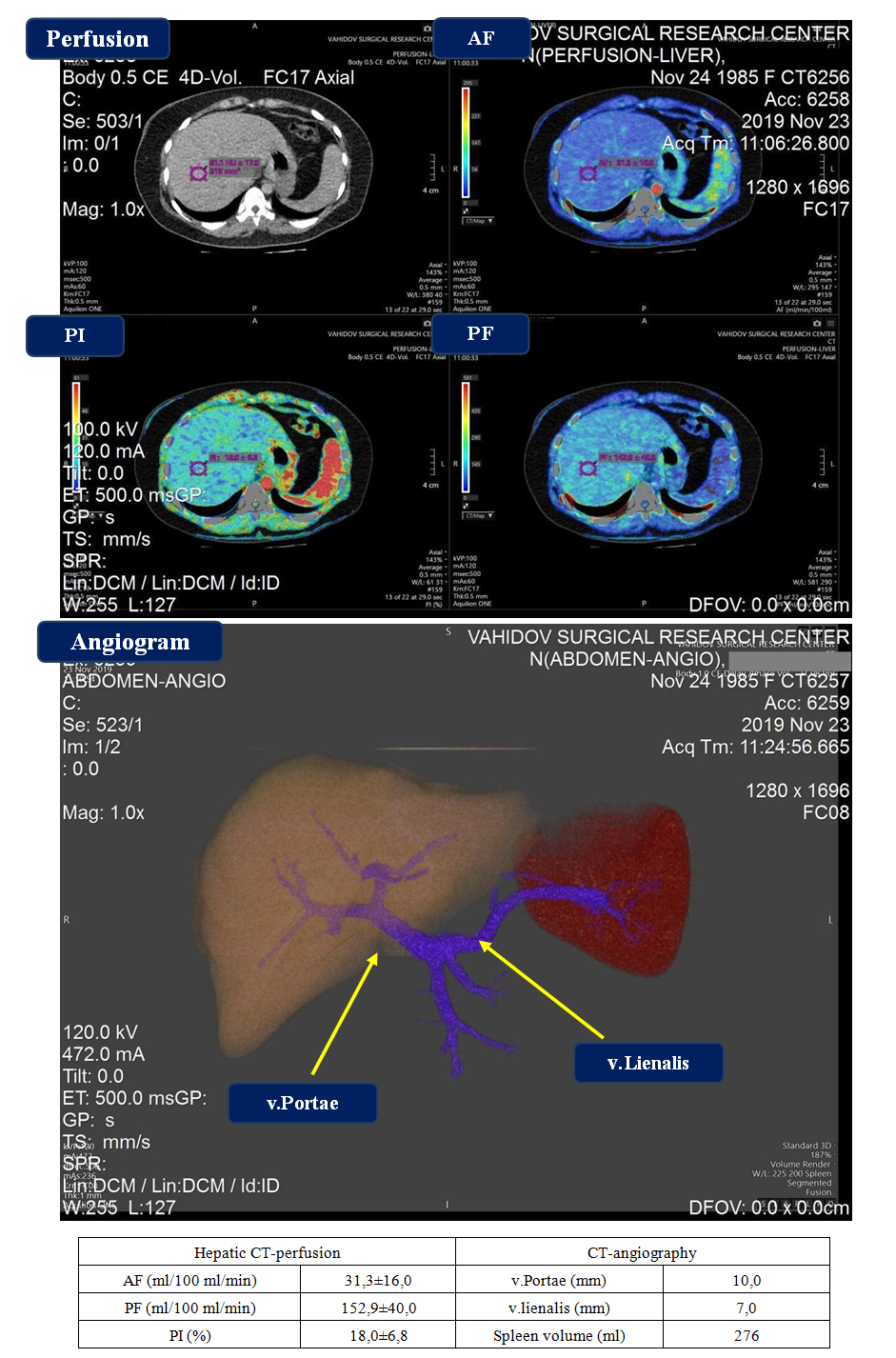 | Figure 3. Normal perfusion CT-imaging and CT-angiogram of the liver |
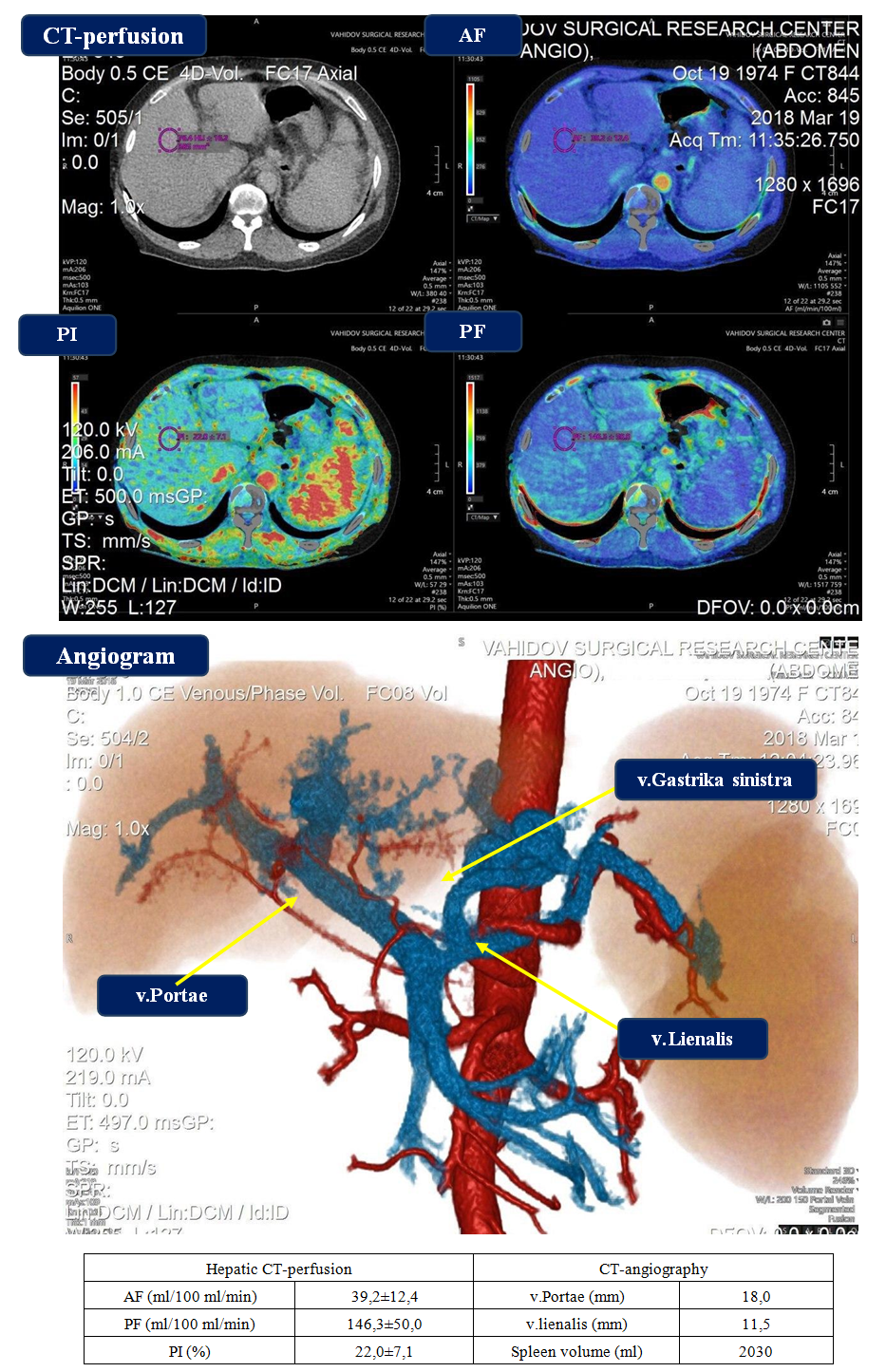 | Figure 4. Perfusion CT-imaging and CT-angiogram in case of liver cirrhosis |
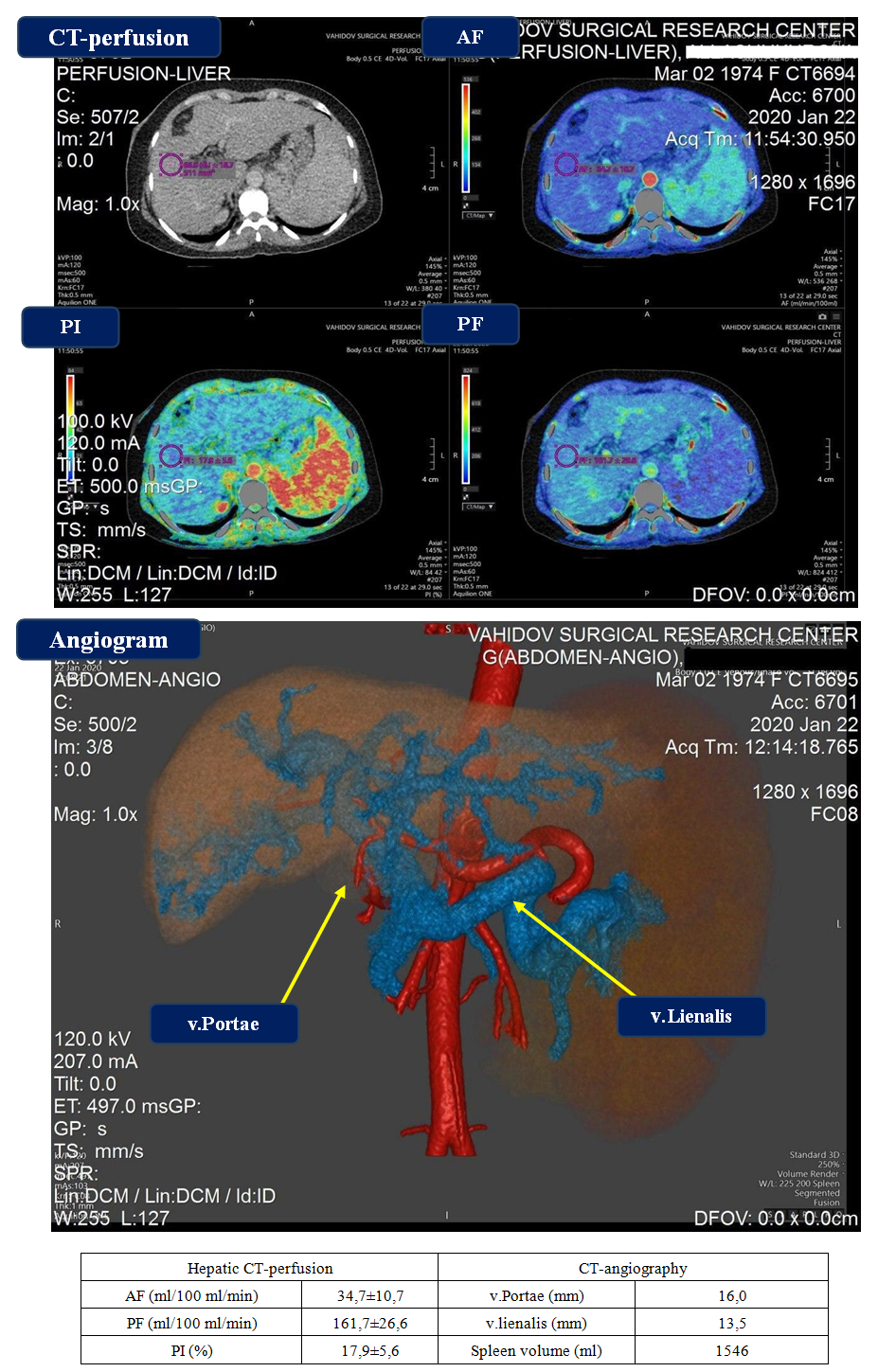 | Figure 5. Perfusion CT-imaging and CT-angiogram in case of liver fibrosis |
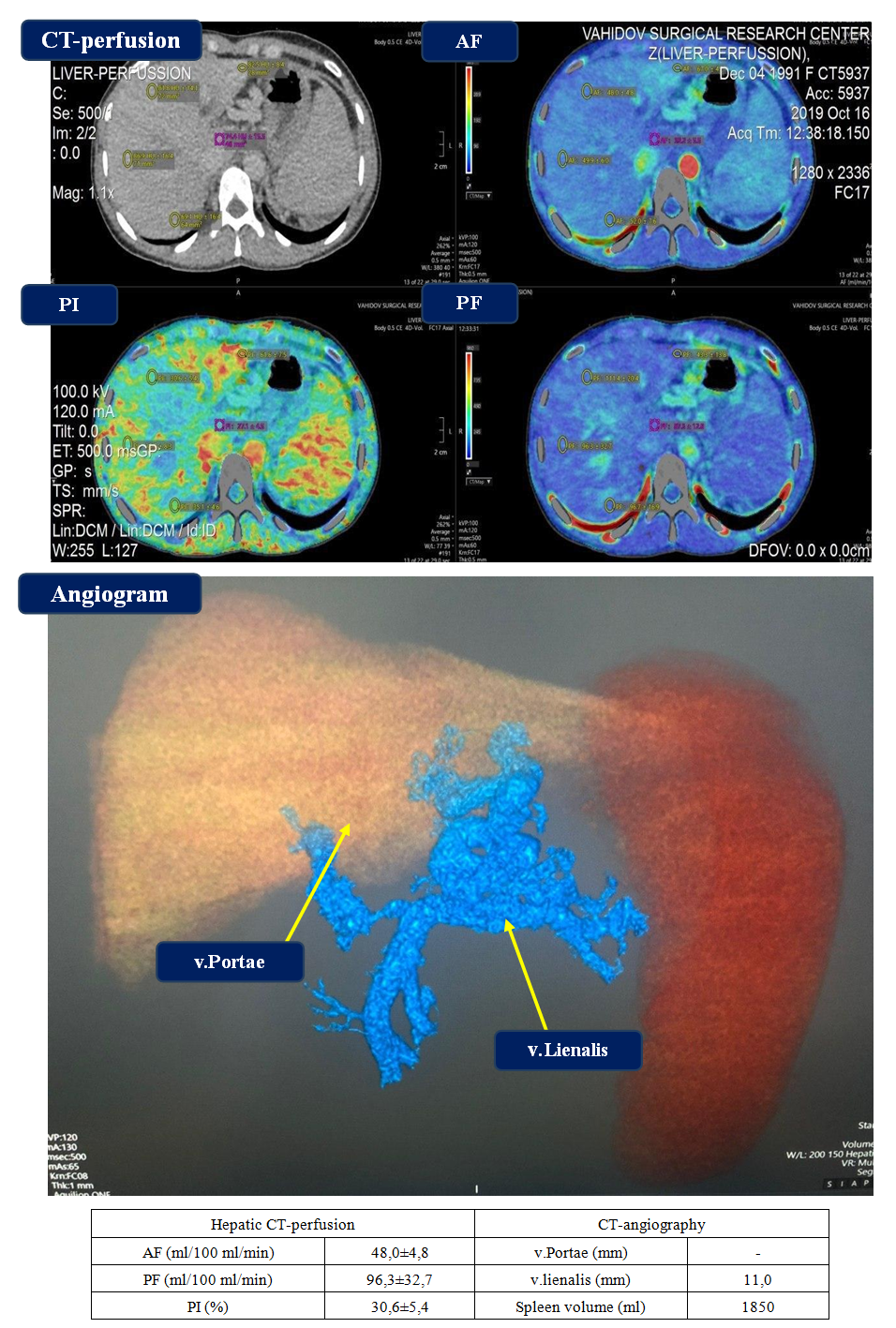 | Figure 6. Perfusion CT-imaging and CT-angiogram in case of extrahepatic portal hypertension |
4. Conclusions
- The etiological factor in the development of PH affects the features of changes in liver perfusion, while blocking the presinusoidal circulation in LF leads to PF increasing with a slight change in AF and minimal increase in the PI.In case of LC with blocking the postsinusoidal circulation, a decrease in the PF is observed, which leads to a compensatory increase in AF and a correspondingly higher increase in the PI.In case of blocking the subhepatic circulation, the most pronounced deviations in liver perfusion are detected: the preservation of the minimum PF level; partial or complete absence of portal blood flow, the maximum compensatory stimulation of reserve capabilities of arterial supply with a significant increase in the PI (with the early development of PH).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML