-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(3): 133-136
doi:10.5923/j.ajmms.20201003.01

Assessment of Results of Instrumental Researches with Damages of the Knee Joint in Persons Who Train with
B. K. Bakiyev1, Sh. A. Mustafaeva2
1Assistant of the Department of Traumatology and Orthopedics of Urgench Branch of the Tashkent Medical Academy
2Assistant of the Department of Occupational Diseases and Folk Medicine of Bukhara State Medical Institute
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

With the introduction of magnetic resonance imaging (MRI) into clinical practice, it became possible to study in detail all the anatomical structures of the knee joint and the changes that occur during their traumatic injury without penetrating the joint cavity [4]. The total number of injuries of the knee joint has increased in recent years due to the popularization of extreme and other sports Many of these sports place high demands on the functional state of the knee joint. Damage to the knee joint is one of the first places among injuries of the musculoskeletal system, making up 4.9-24% and 10-24% of all injuries of the lower extremities and 40-50% of injuries of all human joints according to different authors . In this case, acute trauma to the knee joint of a person occurs in 43-80% of cases.
Keywords: Echostructure, Femoris muscle mediocellar fold, Paracapsular zone, Synovitis Traumatology, Orthopedic, Ultrasound, MAGNETOM Avanto, Popliteal region
Cite this paper: B. K. Bakiyev, Sh. A. Mustafaeva, Assessment of Results of Instrumental Researches with Damages of the Knee Joint in Persons Who Train with, American Journal of Medicine and Medical Sciences, Vol. 10 No. 3, 2020, pp. 133-136. doi: 10.5923/j.ajmms.20201003.01.
1. Introduction
- The problem of accurate diagnosis of damage to the structures of the knee joint to date remains difficult. Known difficulties with examination of the knee joint in the acute period after an injury often lead to late diagnosis and a decrease in the effectiveness of treatment [2,9].Indications and contraindications for the use of ultrasound (ultrasound) is a widely used method [5,10].The accuracy of the MRI diagnosis on the fact of meniscus damage exceeded the accuracy of the clinical and radiological examinations and amounted to 89.1% in total. In this case, transchondral ruptures of menisci in the area of the body and horn were most fully revealed - up to 91.7% [1,5].The problem of timely and high-quality diagnosis of damage to the structures of the knee joint remains one of the pressing issues of modern traumatology and requires further study.The aim of the study was to study and evaluate instrumental research methods - ultrasound and MRI - in individuals with injuries of the knee joint who are constantly involved in sports.
2. Materials and Methods
- A total of 326 patients aged 16 to 55 years were examined, with injuries of the knee joint in people constantly involved in sports who were treated at the sports injury department of the Research Institute of Traumatology and Orthopedics of the Ministry of Health of the Republic of Uzbekistan in 2011-2013. Among the examined men were 72.7% (n = 237), and women 27.3% (n = 89). Most often, people aged 22-35 years sought medical help (49.5%, n = 160). In the next place, patients aged 36-60 were located - 35.3% (n = 115), the least patients were among adolescents 15-17 years old (0.9%, n = 3) and older than 60 years (3.4%, n = 11). The nature of the injury in all patients was sports (n = 326). The causes of knee injury among men were dominated by football (54.4%), wrestling (22.8%), and among women practicing rhythmic and sports gymnastics (42.7%), as well as basketball (28.1%).Most patients showed lateral meniscus damage (58.9%; n = 192), some patients showed damage to the medial meniscus (27.6%; n = 90), a certain group of patients consisted of patients with injuries of both menisci (12.6%; n = 41). Of all the examined, 43.6% (n = 142) showed hamstring tendons enthesopathies.Clinical and laboratory examination of the observed patients was traditional in orthopedic surgery (preoperative and postoperative general clinical and biochemical studies).Ultrasound diagnostics to detect injuries of the menisci of the knee joint, collateral ligaments, soft tissue structures surrounding the knee joint was performed in 102 (31.3%) patients. The study was carried out by linear or convex sensors with a frequency of 5 to 10 MHz, on an ultrasonic scanner HDI-3500 and IU 22 (Philips) in real time.Various protocols (T1- and T2-modes) were used for MRI of the knee joint; studies were performed on 201 (61.7%) patients in the coronary and sagittal planes. The condition of menisci, cartilage, ligamentous apparatus, bone substance was examined in detail using a special method on a Siemens MAGNETOM Avanto 1.5 T.The data obtained during the study were subjected to statistical processing on a personal computer using the programs developed in the Excel and Statistic 6.0 packages. All results and conclusions are based on the principles of evidence-based medicine.The obtained results and their discussion. In the course of the study, we tried to answer the question about the diagnostic effectiveness of ultrasound in determining damage to the soft tissues of the knee joint during damage to the menisci of the knee joint in individuals who are constantly involved in sports.It was found that ultrasound diagnosis is much easier to perform and more economical for patients, and ultrasound of the knee joint can be performed with changes in its position in the mode of communication with the patient, which increases the diagnostic value of the study.As our observations have shown, the advantage of ultrasound over other methods for diagnosing lesions of the knee joint is the ability to study not only bone structures and muscles, but also ligaments, cartilage, joint bags, as well as detecting fluid in the joint cavity. This feature of the study allows you to identify early lesions of the soft tissues, which is almost impossible with joint radiography. Ultrasound of the joints clearly visualized ruptures of the ligaments of the knee joint, hemorrhages in the ligament, violations of the structure of the ligament, tears of the meniscus of the knee joints are visible, but the diagnosis of cruciate ligament ruptures is difficult due to their poor visualization. At the beginning of the study, the patients were lying on their stomach, their legs were slightly bent at the knees. The sensor was located in the popliteal fossa region parallel to the length of the axis of the lower extremity at the site of maximum pulsation of the artery, determined by palpation, and on the monitor screen this position served to determine the correct position of the sensor.Under the control of the arm, the sensor was projected laterally along the projection of the joint space until a wedge-shaped echopositive structure of moderate intensity appeared on the screen, which corresponded to the posterior horn of the external meniscus in 98.0% of cases (n = 100) from all studies. Moreover, before visualization of the horn of the meniscus, the sesamoid bone was sometimes detected in 8 cases (7.8%).Then the patient turned to the sore side, the leg bent at the knee to 50-60°, the sensor was placed in the projection of the joint space above the intermediate part of the meniscus and gradually shifted forward until the structure of the front horn was visualized on the monitor screen. From this position, visualization was high and allowed to determine the anterior horn of the lateral meniscus in 97 cases out of 102 (95.1%). The medial meniscus was also studied in a similar manner, where a qualitative scan of the anterior horn of the medial meniscus was also performed in 93.1% (n = 95) cases. The difference between the indicators is not statistically significant, and therefore it can be argued that both meniscus are viewed the same.Examination below the popliteal region of the knee joint at an angle of 60° from the longitudinal section allowed us to visualize the medial and lateral heads of m.gastrocnemius. The results were identical to each other - respectively, 95.1% (n = 97).A 90° rotation of the ultrasound probe from the longitudinal axis of the limb in the projection of the femur made it possible to visualize the medial and lateral condyles of the femur in 99.0% (n = 101) cases, vessels of the popliteal region in 100% of cases (n = 102), partially posterior and anterior cruciate ligaments in 99.0% (n = 101) cases.The study of the anterior knee joint allowed us to assess the condition of the patella (99.0%, n = 101), the tendon m.quadriceps (98.0%, n = 100), the patellar ligament (100.0%, n = 102), fat bodies (98.0%, n = 100) and upper inversion of the knee joint (99.0%, n = 101).In the protocols of ultrasound of the knee joint of the patients examined by us (n = 102), the following positions were reflected: the presence of effusion in the upper inversion (yes, no); fluid echostructure (homogeneous, heterogeneous); the presence of foreign bodies (yes, no); tendons of the rectus femoris muscle (integrity is broken, not broken); patella (contours are even, uneven), own ligament (integrity is broken, not broken), structure (homogeneous, heterogeneous, decreased echogenicity), presence of bursitis (yes, no); state of fat bodies (structure changed, not changed), hypertrophy (yes, no); the state of the mediocellar fold (structure changed, not changed), damage (yes, no); lateral ligaments (structure changed, not changed); the presence / absence of tendon diastasis during a functional test; articular surfaces of the femur and tibia (smooth, uneven), bone growths (yes, no), the presence of additional inclusions (yes, no); hyaline cartilage (contours are even, uneven), thickness (thinned, within normal limits - up to 3 mm); menisci: external - (the form is regular, irregular), structure (homogeneous, inhomogeneous), contours (clear, fuzzy, even, uneven), fragmentation (yes, no), calcification (yes, no), fluid formation in the paracapsular zone ( yes, no); internal - in a similar way the shape, structure, contours, the presence of fragmentation, calcifications, paracapsular zone are described; the presence of a Becker cyst in the popliteal region (yes, no).With trauma, an effusion in the joint cavity is visible due to hemorrhage and reactive inflammation. For chronic injuries, the meniscus compaction and heterogeneity are visualized.As a result of the obtained data, the following main indications were determined for ultrasonography in patients with knee joint pathology: synovitis; damage and inflammation of the ligament component and muscles; the presence of free bodies in the joint, cysts; damage to menisci, cartilage.The advantage of this method is: non-invasiveness, harmlessness, speed of implementation, multiple studies and relatively low costs. But at the same time, the ultrasound picture of ruptures of the meniscus of the knee joints is often uninformative, since the rupture line is not always visible.In recent years, the possibilities of radiation diagnostics have expanded significantly due to the appearance of ultra-high field MRI (3 Tesla). However, the possibilities of this method in clinical practice are still not well understood, which does not allow them to be included in the clinical algorithms for examining patients with injuries of the knee joint.When MRI was performed on the mid - sagittal sections, the fibers of the quadriceps muscle and tendon of the patella were clearly visible with low intensity of the MR signal in T1 and T2 images in 88.1% (n = 177) of the total number of patients. The fatty tissue located beneath the patella almost always (99%, n = 199) gave a high-intensity MR signal in both T1 and T2 images. In this case, large vessels in the popliteal fossa were clearly visualized with an increased MR signal in T2 images (99.5%, n = 200) and a reduced MR signal in T1 images (100.0%, n = 201). In these conditions, the artery was located in the front, and the vein in the back.Collateral ligaments in sagittal images usually did not differentiate (0%). It should be noted that the unchanged synovial membrane is practically not visualized (1.0%, n = 2). Own ligament of the patella, Goff's fatty body, muscles and their tendons were clearly differentiated in 194 cases (96.6%) due to their natural MR contrast.At the same time, in this projection it was impossible to assess the state of the lateral and medial collateral ligaments, intercondylar elevations of the tibia; in addition, there was little information on the condyle of the femur and tibia. Images of the knee joint in the frontal projection were mainly necessary to determine the condition of the collateral ligaments, condyles of the femur, menisci, intercondylar elevations of the tibia and, to a lesser extent, the anterior and posterior cruciate ligaments. This projection was optimal for assessing the state of the medial collateral ligament.The lateral collateral ligament is identified (98.0%, n = 197) in the posterior frontal sections in the form of a thin tape with a low MP signal intensity in T1 and T2 images (Fig. “A”). The ligament extends from the head of the fibula to the lateral condyle of the femur. It is separated from the lateral meniscus of the knee joint by a layer of adipose tissue giving a high-intensity MP signal in T1 and T2 images.The medial collateral ligament was identified in 199 cases (99.9%) in the mid sections. The meniscus of the knee joint looks like a bundle of fibers with a low-intensity signal in the T1 and T2 modes, extending from the medial condyle of the femur (Fig. “B”).
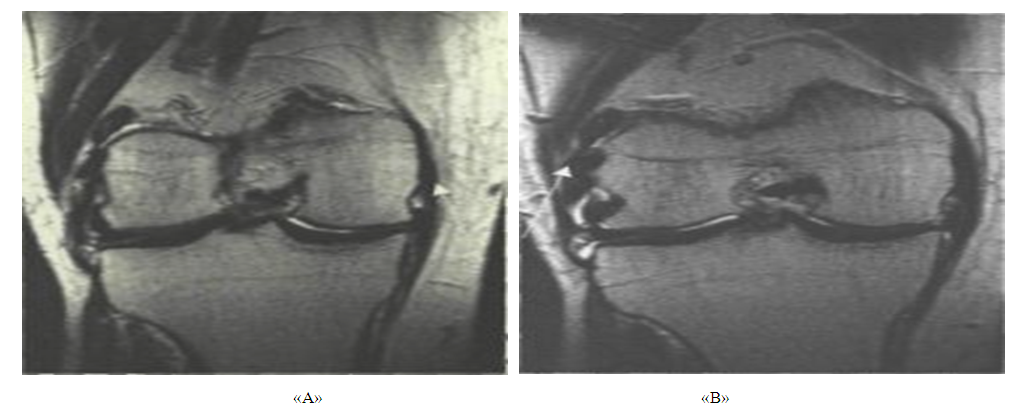 | Figure 1. MRI image of lateral ("a") and medial ("b") collateral ligaments (patient M., 26 years old) |
3. Conclusions
- 1. Ultrasound for damage to lateral and medial meniscus of the knee joint has great diagnostic value and allows to determine the presence of enteropathy of the hamstring in patients. The correct step-by-step technique of this study is the key to the correct diagnosis and successful treatment of this category of patients. This method of research is offered as additional research to arthroscopic for the final diagnosis of patients.2. In pre-operative training, MRI improves diagnosis and increases the positive outcome of surgery. In this regard, MRI is recommended for the diagnosis of damage to lateral meniscus knee and enteropathy of the hamstring in persons constantly engaged in sports.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML