-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(2): 112-116
doi:10.5923/j.ajmms.20201002.08

Future of Reproductive System after Massive Obstetric Bleeding and Analysis of Childbirth Stories with Postpartum Hemorrhage
N. N. Karimova
Bukhara State Medical Institute Candidate of Medical Sciences, Associate Professor of the Department of Obstetrics and Gynecology
Correspondence to: N. N. Karimova, Bukhara State Medical Institute Candidate of Medical Sciences, Associate Professor of the Department of Obstetrics and Gynecology.
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of our study was to retrospectively examine the history of childbirth and the quality of primary care for bleeding and evaluate the prescribed rehabilitation measures for women who have suffered postpartum hemorrhage and massive bleeding. The materials and methods of the study were 242 birth histories with postpartum hemorrhage for the last 6 years (2013-2018) in the city maternity hospital of Bukhara. The average age of the patients was 26.7 ± 1.2 years. The obstetric pathology leading to bleeding mainly consists of uterus hypotonia - 143 (59.1) and large fetus - 68 (28.1), and preeclampsia and DIOV are equal amounts - 33 (13.64). Only about 20% of women who had postpartum hemorrhage underwent early rehabilitation in the form of prescribing contraceptives.The aim of the research was to study the effectiveness of modern principles of stopping postpartum obstetric bleeding. From 127 cases of bleeding in 101 women (79.5%) the childbirth were with the operational method. With the development of blood loss was renderedstepwise ways to stop bleeding. During hemostasis of the bleeding, ligatures were imposed on the ovarian arteries and the ascending branch of the uterine artery for ischemicization of the uterus, which was effective in 30 (30%) women, and in 114 (89.7%) women managed to achieve organ-sparing tactics.
Keywords: Bleeding, Postpartum hemorrhage, Pregnancy, Massive bleeding, Obstetric bleeding, Hypotonia of the uterus, Cesarean section, Reabilitions
Cite this paper: N. N. Karimova, Future of Reproductive System after Massive Obstetric Bleeding and Analysis of Childbirth Stories with Postpartum Hemorrhage, American Journal of Medicine and Medical Sciences, Vol. 10 No. 2, 2020, pp. 112-116. doi: 10.5923/j.ajmms.20201002.08.
Article Outline
1. Introduction
- Among the various obstetric complications arising in childbirth and the early postpartum period, bleeding continues to occupy one of the leading places [1,2]. In the population of women of reproductive age in 15.5% obstetric complications (atonic bleeding, pathology of the placenta, scar on the uterus, rupture / perforation of the uterus, severe pre-eclampsia) caused radical operations [3,4]. One of the factors affecting the growth in the frequency of obstetric hemorrhage at the present days is the increase the numbers of abdominal delivery. The frequency of bleeding during abdominal delivery increased by 3-5 times, compared with spontaneous birth [5]. In some cases, surgery is complicated by even more massive bleeding, mainly due to a decrease in the contractile function of the myometrium. Saving a woman's life in critical situations is the main task of obstetricians, since obstetric hemorrhages are the main cause of maternal mortality, accounting for 20-25% in pure form, 42% as a competing cause, and up to 78% as a background cause [1,3]. At the same time, pathological blood loss in childbirth and the postpartum period has an adverse effect on the subsequent health of the woman [6,7]. In obstetric practice, bleeding continues to be the most serious problem, as among the causes of maternal mortality they constitute 20-25% [2,4,5].The most common causes of bleeding at Caesarean section are hypo- and atonic states of the uterus and DIC (dissemination intravascular coagulation) syndrome [6,7]. Hypotonia of the uterus is accompanied by 1.8% of all Cesarean section operations. In case of massive bleeding the main task of obstetricians is to save the woman’s lifewith hysterectomy, and then to prevent immediate and remote complications [8,9]. This prompted us to analyze the immediate and long-term results of assisting 127 women with acute massive obstetric blood loss in our clinic over the past 5 years.Among the various obstetric complications, obstetric hemorrhages are among the leading ones, which were and remain the most dramatic among the urgent complications in obstetrics. This is due to their intensity, the rapid increase in the volume of blood loss up to the critical, the rapid depletion of the compensatory mechanisms of the body and the inevitable finale of the general pathophysiological process - the development of DIC syndrome [4,5]. Currently, obstetric hemorrhages continue to attract the attention of obstetricians and gynecologists in all countries of the world. Australian obstetricians rightly point out that obstetric bleeding, as the leading cause of maternal mortality, is becoming an international problem [8]. However, this position contains a certain contrast in assessing the actual situation. Thus, in the most backward regions of the world, as a result of pregnancy and childbirth, during the entire reproductive period of life, every sixth woman still dies, on average, and in the Nordic countries, only every 30,000th woman [12]. The authors note that the differences in the indicators of maternal death from obstetric hemorrhage exist not only for the regional, but also for a number of other factors, which is both a general medical and a social problem. E.K. Aylamazyan et al. [2] note that bleeding is most often observed in the postpartum and early postpartum periods — 15.3 per 1000 births, with placenta previa -1.7 per 1000 births, and with premature detachment of a normally located placenta — 9, 1 per 1000 genera. Some people believe that postpartum bleeding can quickly lead to the development of DIC and remains an important cause of maternal mortality [6,7]. Analysis of massive obstetric bleeding in women (“nearly dead”, “nearmiss”) showed that hypo- and atony of the uterus was observed in 76.6%, pre-time detachment of a normally located placenta in 19.1%, tight attachment placenta - 3.2% and 1.1% placenta previa [10].EK Aylamazyan et al. indicate that at the present time precisely bleeding in the postpartum period leads in frequency among other obstetric hemorrhages and believe that among all the bleeding leading to maternal mortality, 50% are caused by hypo or atony of the uterus in the postpartum period [1,2].Thus, in general, based on the foregoing, postpartum hemorrhage is a very serious obstetric problem, which requires further more detailed study.The aim of our study, was to retrospectively examine the history of childbirth and the quality of primary care for bleeding and evaluate the prescribed rehabilitation measures for women who have suffered postpartum hemorrhage and massive bleeding.The aim of our work was to evaluate the immediate and long-term results of massive postpartum bleeding. Analysis of the mortality of pregnant women and woman in labor from bleeding indicates certain defects in the organization of the therapeutic and prophylactic process in antenatal clinics and maternity homes, and every seventh of them suffers from bleeding, which in 50% is caused by hypo- or atony of the uterus in the postpartum period. Postpartum hemostasis is a complex and multicomponent process [8,9,10].
2. The Aim of Our Research
- Was to study the effectiveness of modern principles of stopping postpartum obstetric bleedingand restoring the reproductive system.
3. Materials and Methods
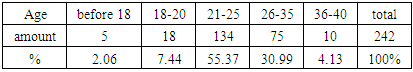
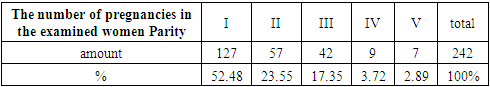
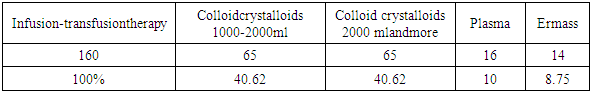
- 242 birth histories with postpartum hemorrhage in the last 6 years (2013-2018) have appeared in the city maternity hospital in Bukhara. Over the past 3 years (2014-2017), 6,400 pregnant women were given birth in the city maternity hospital in Bukhara, more than half of them were threatened with bleeding. Massive blood loss (over 1000 ml) occurred in 127 (1.9%) women.Age characteristics of patients.
|
|
4. Results of Research and Discussion
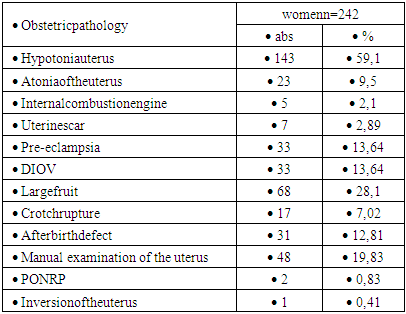
- Analyzing in detail the causes of obstetric pathology leading to bleeding, we can say that the main part is uterine hypotonia - 143 (59.1) and large fruit - 68 (28.1), and preeclampsia and DIOV are equal in number - 33 (13.64). This can be explained by the fact that pregnancy with a large fetus and pre-eclampsia is often complicated by postpartum hemorrhage.
|
|
|
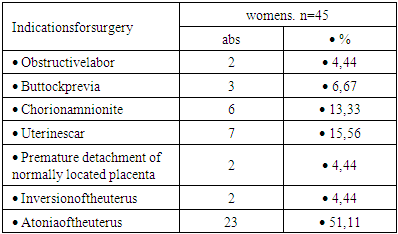
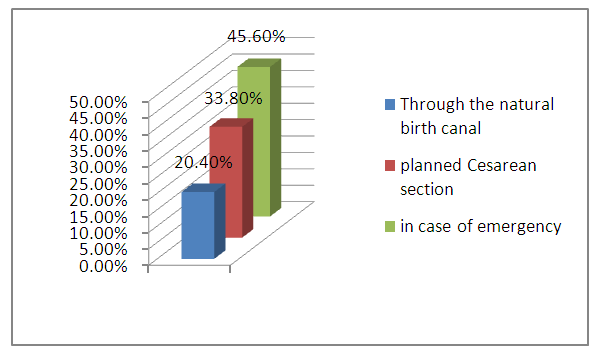 | Figure 1. Analysis of childbirth, wichcomplicated by massive blood loss |
5. Results
- For bleeding after vaginal delivery (26 cases; 20.4% of the number of bleeding), we used the drug method (uterotonic agents), oxytocin 5 units. intravenously - in 12 (9.4%) patients. Manual examination of the walls of the postpartum uterus, with bimanual compression, was performed in 9–7%, administration of misoprostol 800–1000 µg per rectum in 2–1.5%.Removal of the uterus with the ineffectiveness of conservative therapy was performed in 1 (0.7%) women. The deliveries were operational in 101 women, 79.5% of the 127 cases of bleeding. With the development of blood loss was phased ways to stop bleeding.During hemostasis of the bleeding, ligatures were imposed on the ovarian arteries and the ascending branch of the uterine artery for ischemicization of the uterus, which was effective in 30 (30%) women.As a next measure, hemostatic compression stitches on the uterus were used. The principle of their application is - the insertion in the same plane of sagital or transverse subserous blanket absorbable sutures with compression of the uterus. A thick thread is used on the piercing atraumatic needle. This method proved to be effective in 49 puerperas, which is 38.7%.From the remaining 43 women in 30 (23.6%) patients of the most effective organ-sparing intervention was ligation of the internal iliac arteries. It is necessary to note that these manipulations are performed only by highly qualified specialists, sometimes with the participation of vascular surgeons. The uterus was removed in 13 (10.2%) women. Today, we can call the removal of an organ to stop bleeding “the operation of despair”, when other ways of preserving the life of the puerperal woman have already shown their futility. Thus, in 114 (89.7%) women we managed to implement organ-preserving tactics.The next step in the treatment of obstetric hemorrhage is the intravenous administration of fresh frozen donor plasma, the infusion of hydroxyethylatedstarch (HES) preparations, proteolysis inhibitors and calloid - crystalloid preparations, taking into account the volume of hemorrhage.The recovery time of menstrual and generative function after childbirth varies widely and largely depends on the conditions of labor, the amount of blood loss in the postpartum period and lactation. After uncomplicated labor in young primiparous women, there is observed earlier (5-6 weeks after delivery) the resumption of menstrual cycles. However, acute blood loss during childbirth leads to disruption of the hypothalamic-pituitary-ovarian system and affects the formation of menstrual and generative functions. The first menstruation after childbirth were moderate in 45%, abundant in 22.2% and scarce in 12.8% of women, 30.3% of women suffered from amenorrhea, in 66% menstruation was irregular, in 34% - regular. Ovulatory cycles are observed in about 40% of non-lactating and in 20% of lactating women. Of the women we examined, 20% did not protect against pregnancy, the rest used various methods of contraception. Studies have shown that the timing of the resumption of menstrual function in women who have undergone abnormal bleeding occurs much later, sometimes absent. Pathological labor, being a major stress for the body, as it is accompanied by abundant blood loss, adversely affects the central nervous system, directly the menstrual function, which requires the use of hormone replacement and antianemic therapy.Based on retrospective analyzes of the history of childbirth of women who have suffered early postpartum hemorrhage, conclusions can be drawn:1. Previously, postpartum bleeding often occurred in the active reproductive at the age of 26.7 ± 1.2 years.2. Obstetric pathologies leading to bleeding appeared among the investigated cases of hypotonia of the uterus against the background of a large fetus and mild and severe preeclampsia.3. Bleeding requires a lot of costs of infusion-transfusion therapy, further complications associated with the transfusion of blood components are very common on the part of infectious disease specialists.4. When studying the history of childbirth after postpartum bleeding, there are no early rehabilitation measures and recommendations for late rehabilitation.5. The development of early and late rehabilitation measures and the determination of the quality of life of women who have undergone obstetric bleeding is required.Analyzing the history of childbirth of women who have suffered early postpartum hemorrhage, we can say that at the stage of obstetric care, in order to save, the patient’s life and the reproductive organ were carried out painstaking work by obstetrician-gynecologists and resuscitators. But this is clearly not reflected in the history of childbirth, incomplete laboratory tests, insufficient re-examinations of patients before discharge, and the lack of rehabilitation measures prompted us to conduct examinations on the heels of these patients in our further scientific research.
6. Conclusions
- Thus, the use of a modern approach to stopping postpartum hemorrhage and the introduction into clinical practice of adequate surgical tactics make it possible to practically abandon organ-bearing interventions and to achieve the preservation of the menstrual and reproductive functions in patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML