Nazirov F. G., Nishanov M. F., Bozorov N. E., Egamov S. Sh., Khojimetov D. Sh.
Andijan State Medical Institute, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Aim of the study was to improve surgical treatment results in patients with gastric and duodenal ulcers complicated by stenosis, aimed at reducing postoperative complications and reducing mortality to 0%. Material 233 patients with pyloroduodenal stenosis were divided into two groups. A comparison included 147 patients: 141 with duodenal ulcer and 6 with gastric ulcer. The main group was consisted of 86 patients: 82 cases with duodenal ulcer and 4 cases with gastric ulcer. Methods The authors developed a therapeutic and diagnostic algorithm for managing patients with gastric and duodenal ulcers, complicated by stenosis. Results The increase in the share of organ-saving surgeries led to a decrease in the frequency of specific complications from 13.6% (in 20 of 147 patients in the comparison group) to 7.0% (in 6 of 86 patients in the main group), and general complications from 10.2% (in 15 from 147) to 5.8% (in 5 of 86) and mortality from 1.4% (2 in the comparison group) to 0. Conclusion The expansion of the complex of preoperative preparation of patients with pyloroduodenal stenosis due to the inclusion of endoscopic bougienage along with other options (probing, conservative therapy) can improve not only the condition of patients, but also motor-evacuation function of the stomach.
Keywords:
Stomach, Resection, Duodenum, Bougienage, Stenosis, Ulcer excision
Cite this paper: Nazirov F. G., Nishanov M. F., Bozorov N. E., Egamov S. Sh., Khojimetov D. Sh., Duodenal Ulcer Complicated by Piloroduodenal Stenosis: Technical and Tactical Approaches of Treatment, American Journal of Medicine and Medical Sciences, Vol. 10 No. 2, 2020, pp. 96-101. doi: 10.5923/j.ajmms.20201002.05.
1. Introduction
Chronic ulcer of pyloroduodenal localization in 10.0- 17.0% of patients is complicated by stenosis of the output part of the stomach. Among other complications of peptic ulcer disease, pyloroduodenal stenosis is an indication for surgical treatment in 45-47%. [1-2]. Despite the high frequency of this complication, the choice of surgical method based on clinical and laboratory studies of the pathological duodenogastric reflux parameters and its role in the development of pathological syndromes has not been studied enough [3].The choice of the operation method for cicatricial-ulcerative pyloroduodenal stenosis has become a subject of discussion in connection with the widespread use of organ-saving surgeries. The introduction of gentle methods using modern drug anti-ulcer therapy into the wide surgical practice can significantly improve surgical treatment results of ulcerative pyloroduodenal stenosis. However, the fear of the prolonged postoperative atony development of the already stretched stomach wall at ulcerative stenosis causes a rejection of vagotomy in favor of gastrectomy [4-6]. The average age of peptic ulcer disease in women is 9 years older than in men [7–9]. However, in recent decades, there has been a noticeable increase in the incidence of ulcer among women, which is associated with stressful situations, the increasing prevalence of bad habits among women, the more frequent use of non-steroidal anti-inflammatory drugs (NSAIDs), and also with a violation of the hormonal function of the ovaries [10].The relatively high incidence rate of morbidity registering more often among urban residents is explained by the peculiarities of urbanization and environmental pollution. They pay attention to the so-called “sharp” professions: drivers, pilots, operators, conveyor workers, etc. Almost any work, if it is associated with psycho-emotional overload, physical and mental stress, frequent business trips, lack of proper rest is a significant factor predisposing to the occurrence of gastric and duodenal ulcers [11-13].From 1 to 2.5 billion dollars are spent annually to treat patients of this category in North America, and currently costs reach up to 4-5 billion dollars. However, these figures do not provide a complete picture of the true incidence of the disease, since they are mainly based on the patients’ appealability for medical care. Pathological data indicate a high prevalence of peptic ulcer.The presence of ulcers and cicatricial changes in the wall of the stomach and duodenum, indicating ulcer are detected in 8-10% and even 20% of cases in the study of a macropreparation [14-16].Thus, peptic ulcer often causing a temporary and sometimes permanent disability is an important social and economic problem.Aim of the study was to improve surgical treatment results in patients with gastric and duodenal ulcers complicated by stenosis, aimed at reducing postoperative complications and reducing mortality to 0%.
2. Material and Methods
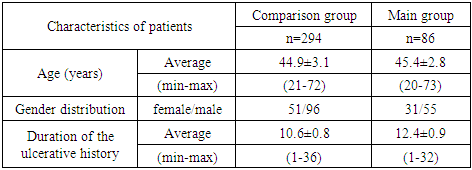
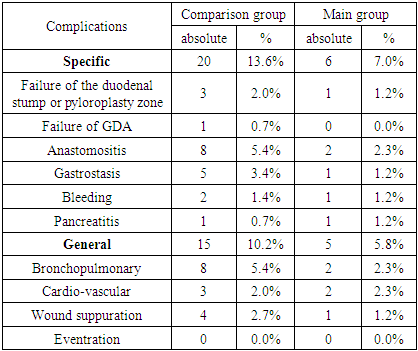
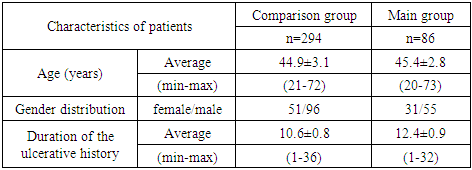
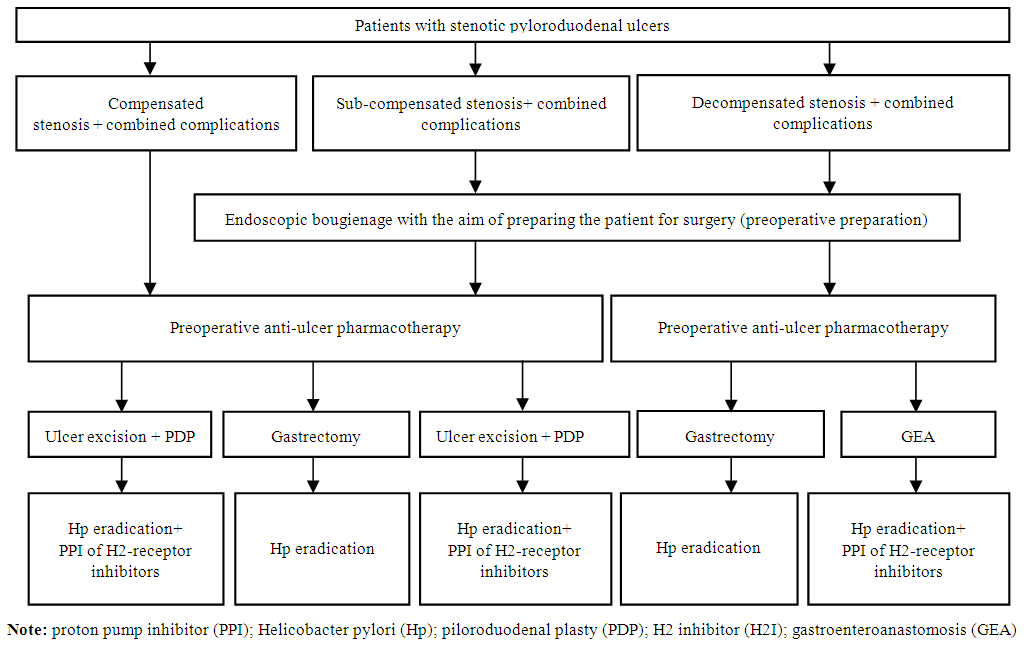
233 patients with pyloroduodenal stenosis received treatment during the study period (2001-2016). All patients were divided into 2 groups: the comparison group (n = 147) and the main group (n = 86). 141 patients were observed with duodenal ulcers and 6 patients – with gastric ulcers in the comparison group. In the main group, duodenal ulcers were noted in 82 cases, gastric ulcers – in 4 cases. Figure 1 presents an algorithm of choosing the treatment tactics for peptic ulcer complicated by pyloroduodenal stenosis. The basis of the algorithm is preoperative endoscopic bougienage with the aim of preparing the patient for surgery and preoperative antiulcer pharmacotherapy for sub-compensated and decompensated stenosis. The quality of preoperative preparation predetermines the further effectiveness of surgical treatment after which the use of eradication therapy of Helicobacter pylori (Hp), a proton pump inhibitor (PPI) of H2-receptor inhibitors is mandatory.The mean age of the patients was 44.9 ± 3.1 years in the comparison group and 45.4 ± 2.8 years in the main group. The duration of the ulcerative history was 10.6 ± 0.8 and 12.4 ± 0.9 years in the comparison group and the main group, respectively (Table 1).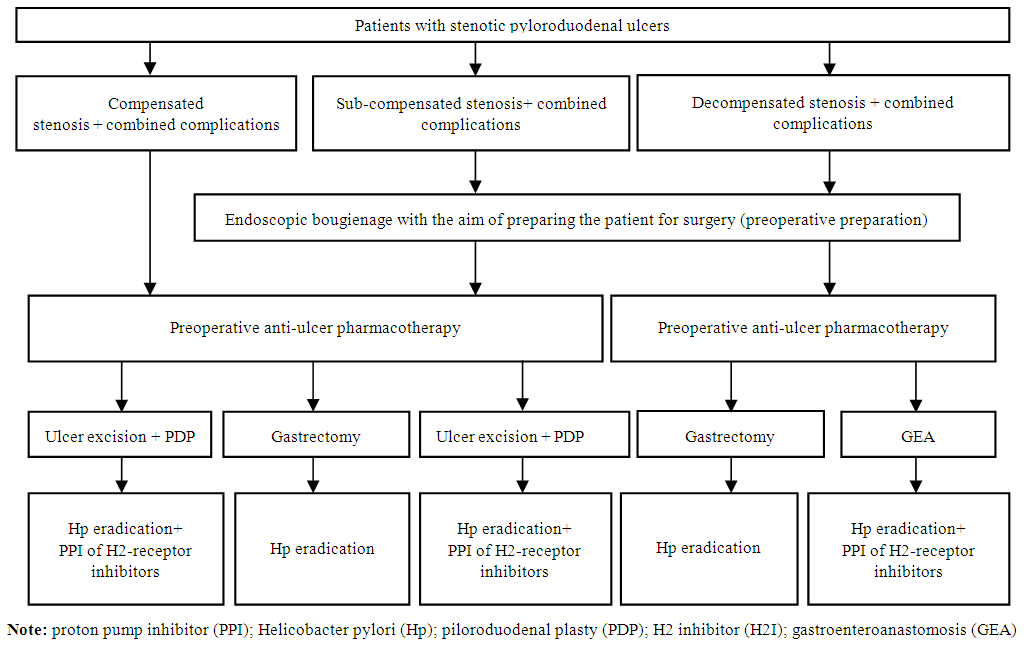 | Figure 1. The algorithm for choosing treatment tactics of peptic ulcer complicated by pyloroduodenal stenosis |
Table 1. General characteristics of patients with stenosis
 |
| |
|
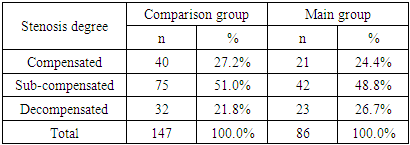
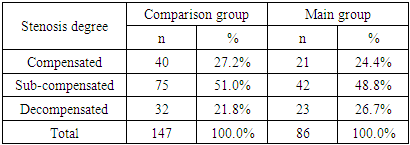
Severe condition of patients on admission were identified in 27.9% (41 of 147) cases in the comparison group and in 30.2% (26 of 86) cases in the main group. According to the stenosis degree of the stomach output part, in most cases sub-compensated stenosis was revealed - 51.0% and 48.8% in the comparison group and the main group, respectively (Table 2).Table 2. The distribution of patients according to the stenosis degree of the stomach output part
 |
| |
|
3. Results and discussion
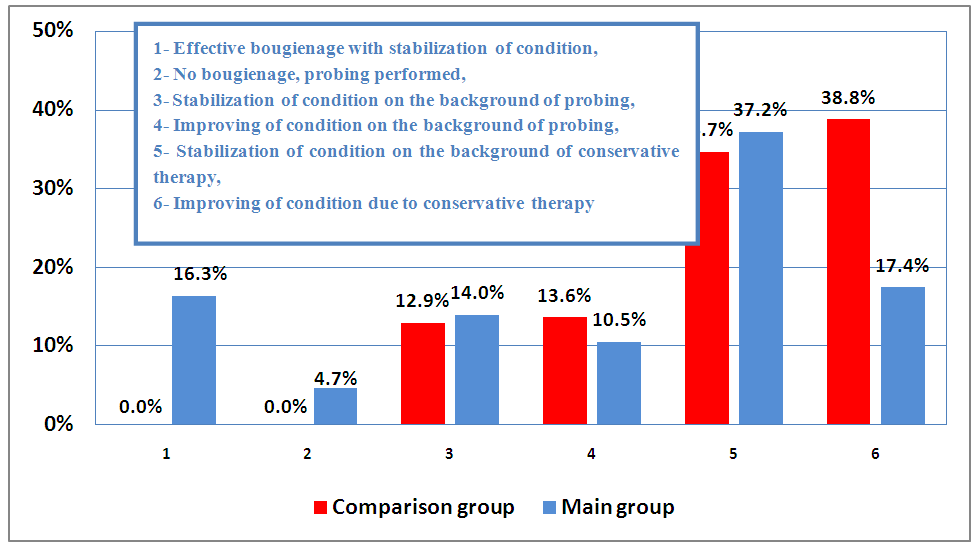
In the preoperative period, effective bougienage with stabilization of the state was noted in 16.3% (14 out of 86) cases of the main group, while in the comparison group they were not observed (Fig.2). Bougienage followed by probing was also performed in 4 patients (4.7%) in the main group. The stabilization of the condition against the background of probing was noted in 12 (14.0%) patients of the main and in 19 (13.6%) patients of the comparison group. In most cases (38.8%; 57 patients) of the comparison group improvement was observed against the background of conservative therapy.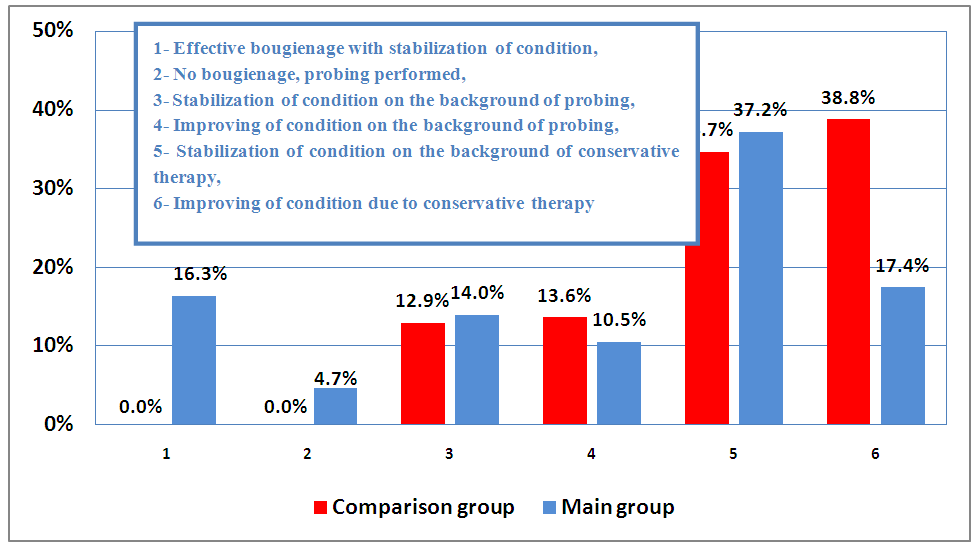 | Figure 2. The quality of preoperative preparation for pyloroduodenal stenosis |
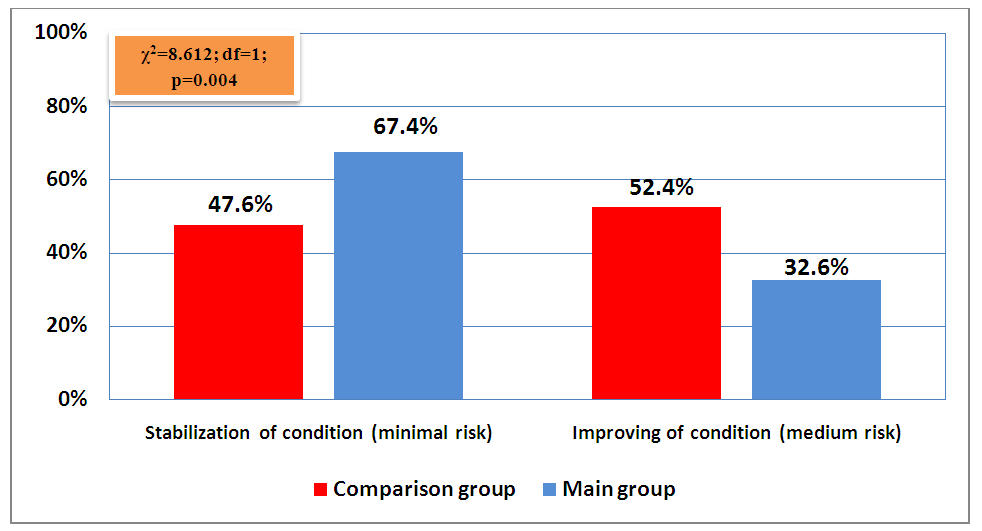
The distribution of patients according to the risk of surgical intervention after preparation is shown in Fig. 3. Thus, stabilization of the state with minimal risk and with a significantly higher frequency was noted in the main group of patients (67.4% versus 47.6%; χ2 = 8.612; df = 1; p = 0.004).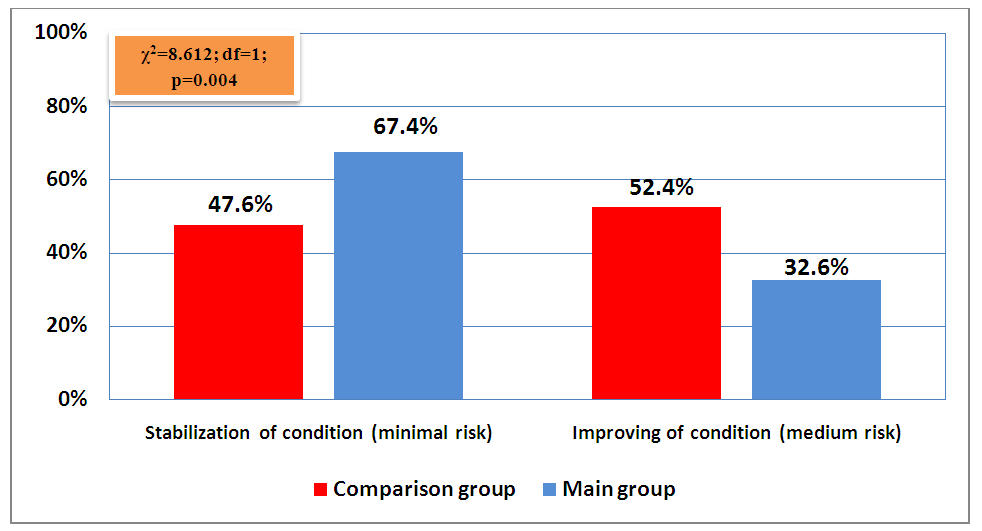 | Figure 3. Distribution of patients by risk of surgical intervention after preparation |
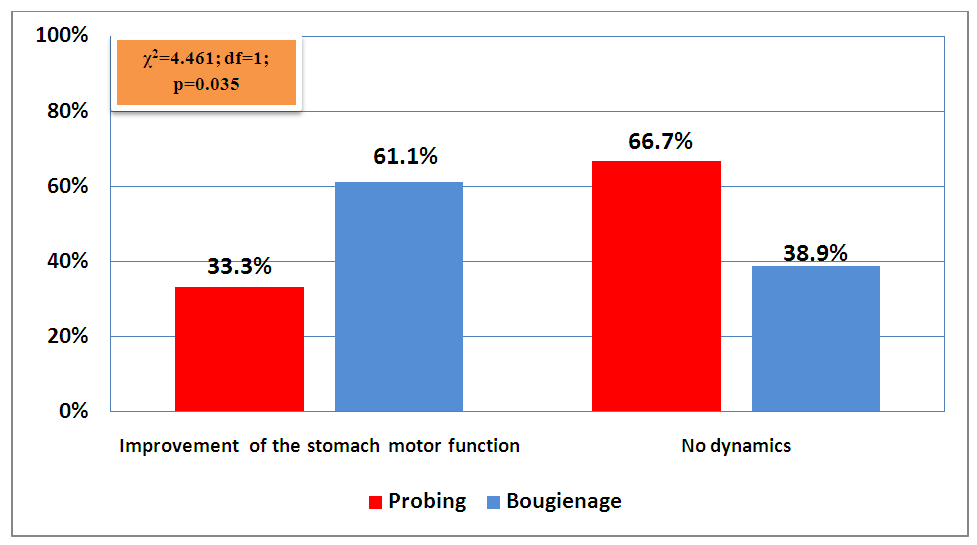
Improvement of motor function at the preparatory stage with gastric probe was noted with a significantly greater frequency in the main group of patients (61.1% versus 33.3%; χ2 = 4.461; df = 1; p = 0.035) (Fig.4).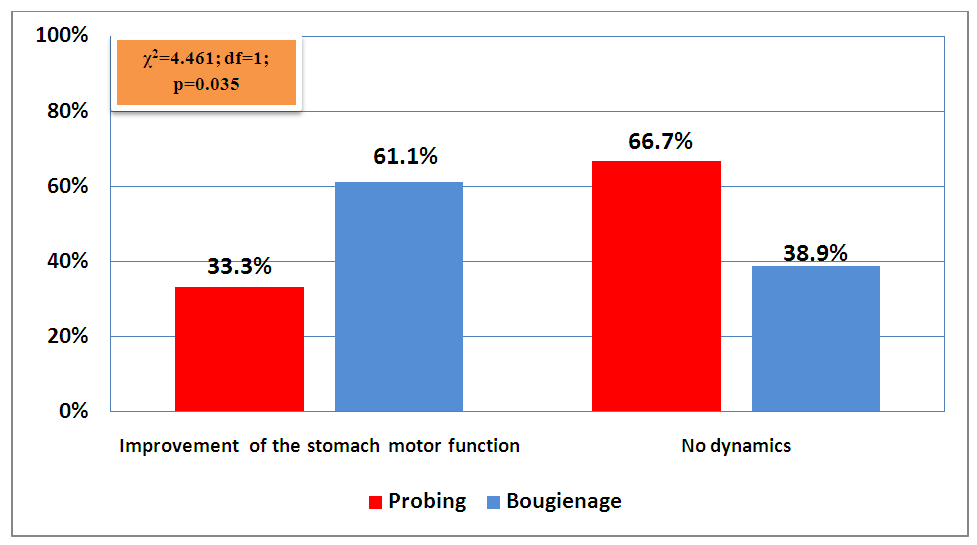 | Figure 4. The influence of the preparatory stage with stomach probing or pyloroduodenal stenosis bougienage |
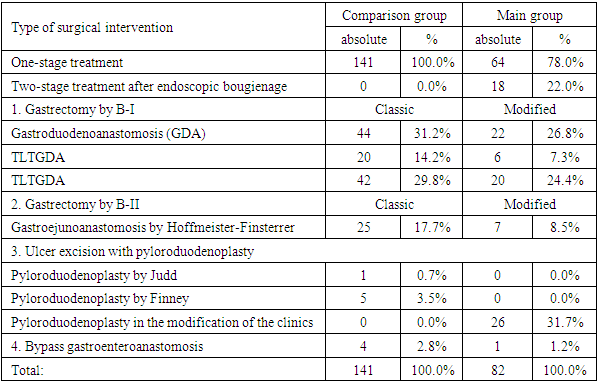
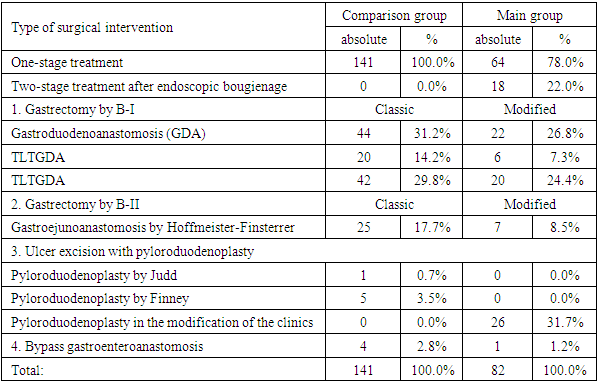
In patients with pyloroduodenal stenosis of duodenal ulcer in the comparison group one-stage surgical interventions were performed in all cases, while in the main group two-stage surgery was also performed, but after endoscopic bougieunage (22.0%; 18 out of 82 cases). In most cases of the comparison groups gastric resection according to B-I with the imposition of gastroduodenoanastomosis (GDA) were performed in 31.2% (44 of 141 cases). Terminolateral transverse gastroduodenoanastomosis (TLTGDA) was performed in 14.2%, terminolateral oblique gastroduodenoanastomosis (TLOGDA) - in 29.8%, and B-II with gastroejunoanastomosis according to the Hoffmeister-Finsterrer was performed in 17.7% (25 patients out of 141). Modified types of surgical interventions were used in the main group of patients, among which ulcer excision with pyloroduodenoplasty was most often performed in the modification of the clinics in 31.7% (26 of 82) cases, ulcer excision according to B-I with GDA in 26.8% (22 from 82) cases and with TLOGDA - 24.4% (Tab. 3).Table 3. Distribution of patients by type of surgical treatment for duodenal ulcer complicated by pyloroduodenal stenosis
 |
| |
|
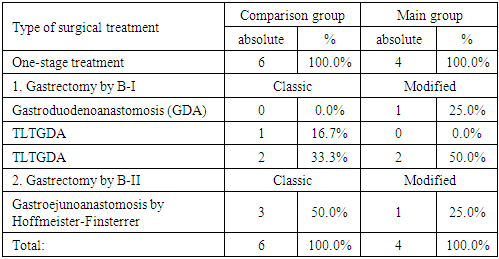
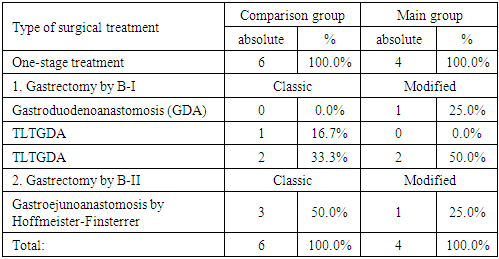
By the type of surgical treatment for gastric ulcers complicated by pyloroduodenal stenosis patients were distributed as follows (Tab. 4): gastric resection by B-I with GDA was performed only in the main group (25.0%; 1 out of 4 observations), with TLOGDA in 2 (50%) cases of the main group and in 2 (33.3%) cases in the comparison group.Table 4. Distribution of patients by type of surgical treatment for gastric ulcer complicated by pyloroduodenal stenosis
 |
| |
|
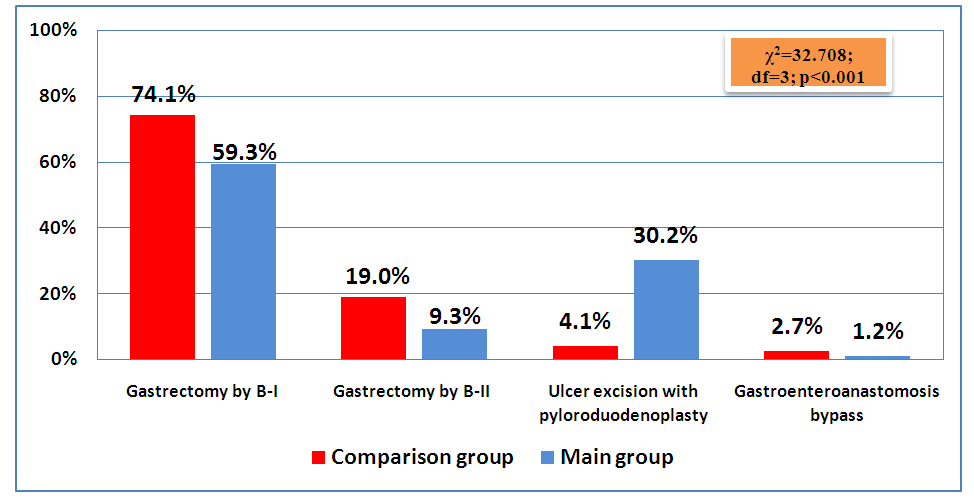
Also, among 6 observations in the comparison group, 3 (50%) patients were performed gastric resection according to B-II with gastroyunoanastomosis by Hoffmeister-Finsterre. As it can be seen from Fig., 5 gastrectomy by B-I was performed in most cases of gastric and duodenal ulcers - 74.1% and 59.3% in the comparison and in the main groups, respectively. 30.2% (26 of 86) of patients in the main group and 4.1% (6 of 147) of patients in the comparison group were performed ulcer excision with pyloroduodenoplasty.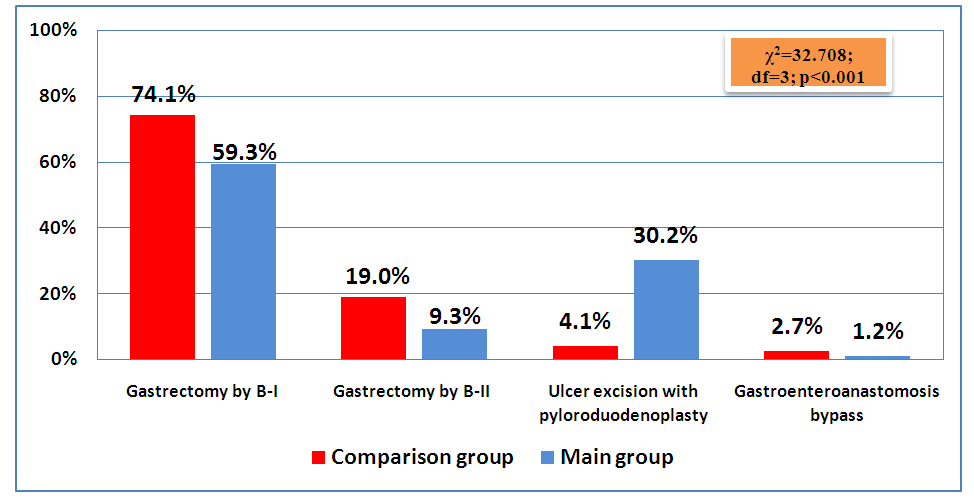 | Figure 5. Type of surgical treatment for gastric and duodenal ulcers complicated by stenosis |
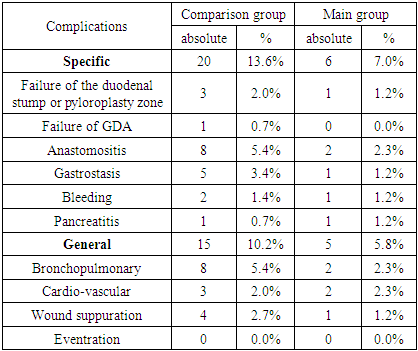
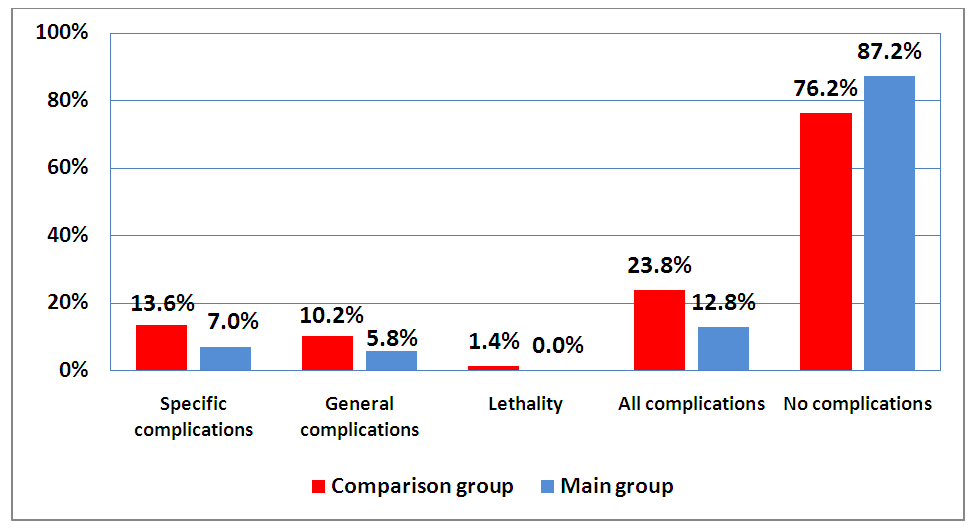
The frequency of specific postoperative complications in the comparison group made up 13.6% (20 observations), in the main group - 7.0% (6 patients) and they were as follows: a failure of the duodenal stump or pyloroplasty zone, GDA failure, anastomositis, gastrostasis, bleeding and pancreatitis. The frequency of general postoperative complications was 10.2% and 5.8% in the comparison group and the main group, respectively, among which bronchopulmonary, cardiovascular complications and suppuration of the wound were registered (Tab. 5).Table 5. The frequency of early postoperative complications in the studied groups
 |
| |
|
As it can be seen from Fig. 6., both specific and general complications were observed with a significantly lower frequency in the main group of patients than in the comparison group (χ2 = 4.158; df = 1; p = 0.042). Mortality in the comparison group was 1.4% (2 cases), but no lethal outcomes were observed in the main group.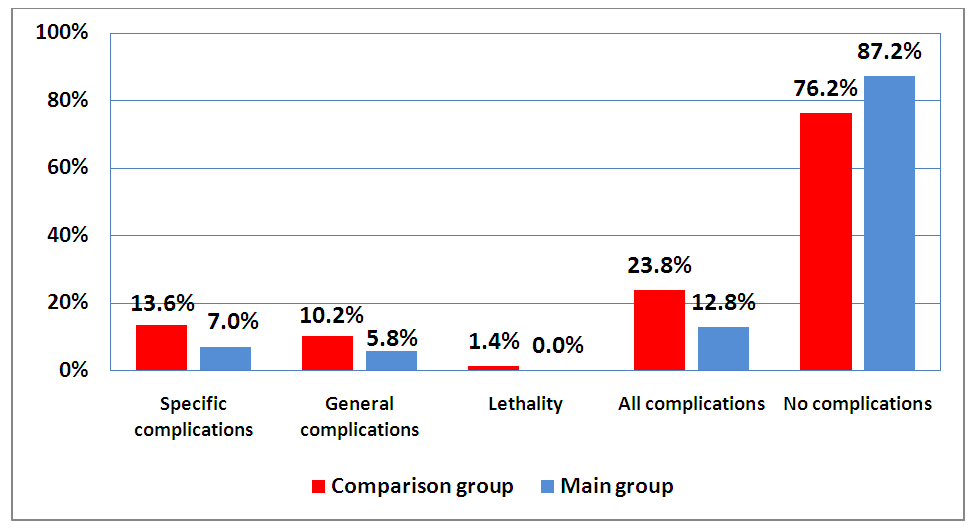 | Figure 6. The surgical treatment results of gastric and duodenal ulcers complicated by pyloroduodenal stenosis |
4. Conclusions
Thus, the inclusion of endoscopic bougienage at the decompensated stage of the process in the complex of preoperative preparation of patients with pyloroduodenal stenosis along with other options (probing, conservative therapy) can reduce the risk of surgical intervention to a minimum in 67.4% of patients (in 58 of 86 patients in the main group) while with standard preparation methods this indicator was 47.6% (in 70 of 147 patients in the comparison group) (χ2 = 8.612; df = 1; p = 0.004), as well as improve motor-evacuation function of the stomach from 33.3% (in 20 of 60 patients with probing) to 61.1% (in 11 of 18 patients with bougienage) (χ2 = 4.461; df = 1; p = 0.035). The expansion of the complex of preoperative preparation in patients with pyloroduodenal stenosis due to the inclusion of endoscopic bougienage along with other options (probing, conservative therapy) can improve not only the condition of patients, but also the motor-evacuation function of the stomach (χ2 = 4.461; df = 1; p = 0.035), which in general, together with an increase in the share of organ-saving surgeries, led to a decrease in the frequency of specific complications from 13.6% (in 20 of 147 patients in the comparison group) to 7.0% (in 6 of 86 patients in the main group), general complications from 10.2% (15 of 147) and 5.8% (5 of 86) and mortality from 1.4% (2 in the comparison group) to 0%. Accordingly, the share of the uncomplicated course of the postoperative period increased from 76.2% (112 in the comparison group) to 87.2% (75 in the main group) (χ2 = 4.158; df = 1; p = 0.042).
References
| [1] | Akzhigitov A.G. Duodenal ulcer complicated by stenosis, pharmacotherapy, indications for surgical treatment: abstract. dis. ... cand. med. sciences / A.G. Akzhigitov. - M., 2009.- P. 28. |
| [2] | Okoyemov M.N. Surgical treatment of ulcerative pyloroduodenal stenosis.: Author. dis. ... doc. med. sciences. - Moscow, 2001.—P.40. |
| [3] | Durleshter V.M. Surgical treatment of decompensated cicatricial ulcer stenosis of the duodenum / V.M. Durleshter, M.T. Didigov // Vestn. surgical gastroenterology. - 2009. - No. 2. - P. 59-67. |
| [4] | Myagkova L.P. Conservative treatment of peptic ulcer / peptic ulcer. Ed. Vasilenko V.Kh. et al. M: Medicine. 2006.P. 207-245. |
| [5] | Nishanov F.N. Organ-saving surgeries for peptic ulcer complicated by pyloroduodenal stenosis: abstract. dis. . doc. med. sciences. - 1987. – P.47. |
| [6] | Adarsh Choudhary et al. Peptic Ulcer: A Review on Epidemiology, Molecular Mechanism of Pathogenesis and Management. IJCPS. 2014; 2(4): 788-796. |
| [7] | Goodwin RD, Talley NJ, Hotopf M, et al. A link between physician-diagnosed ulcer and anxiety disorders among adults. Ann Epidemiol 2013; 23:189. |
| [8] | Pugaev A.B. Treatment of patients with pyloroduodenal stenosis / A.B. Pugaev, M.G. Negrebov, V.V. Sobolev // Surgery. - 2007. - No. 10. - P.26-30. |
| [9] | Rukhlyada N.V., Nazarov V.E., Ermolaev I.A. Diagnositics and treatment of peptic ulcer complicated by stenosis. - St. Petersburg: DEAN Publishing House, 2006. – P.240. |
| [10] | Leeman MF, Skouras C, Paterson-Brown S. The management of perforated gastric ulcers. Int J Surg. 2013; 11(4): 322-4. |
| [11] | Aro P, Storskrubb T, Ronkainen J, et al. Peptic ulcer disease in a general adult population: the Kalixanda study: a random population-based study. Am J Epidemiol 2006; 163:1025. |
| [12] | Behrman S.W. Management of Complicated Peptic Ulcer Disease / S.W. Behrman // Arch. Surg. - 2005. - Vol.140. - P.201-208. |
| [13] | Boyd-Carson H, Doleman B, Cromwell D, Lockwood S, Williams JP, Tierney GM, Lund JN, Anderson ID; National Emergency Laparotomy Audit Collaboration. Delay in Source Control in Perforated Peptic Ulcer Leads to 6% Increased Risk of Death Per Hour: A Nationwide Cohort Study. World J Surg. 2019 Oct 29. |
| [14] | Gilliam A.D. Current practice of emergency vagotomy and Helicobac¬ter pylori eradication for complicated peptic ulcer in the United Kingdom / A.D. Gilliam, W.J. Speake, D.N. Lobo // Br. J. Surg. - 2003. - Vol.90, №1. - P.88-90. |
| [15] | Nagashima K, Tominaga K, Fukushi K, et al. Recent trends in the occurrence of bleeding gastric and duodenal ulcers under the Japanese evidence-based clinical practice guideline for peptic ulcer disease. JGH Open 2018; 2:255. |
| [16] | Ozeki K, Asano M, Furuta T, Ojima T. Relationship between primary eradication of Helicobacter pylori and drinking habits in women: collaborative research between a pharmacy and a clinic. Epidemiol Infect. 2019 Oct 22; 147: e292. doi: 10.1017/S0950268819001730. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML