-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(2): 77-80
doi:10.5923/j.ajmms.20201002.02

Features of the Course of Hypertension Disease in People with Dyslipidemia
D. A. Ochilova1, N. G. Rakhmonkulova2, Sh. H. Sobirov2
1Department of Physiology, (Head of Department-Docent D.A. Ochilova) Bukhara State Medical Institute Named after Abu Ali Ibn Sina Ministry of Health of Uzbekistan
2Assistant of the Department of Physiology Bukhara State Medical Institute Named after Abu Ali Ibn Sina Ministry of Health of Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article describes the distribution of dyslipidemia among patients, one of the most important risk factors for hypertension, and its age and gender characteristics. The results of studies on diurnal changes in blood pressure in patients with arterial hypertension with dyslipidemia, important aspects of correction are also presented. The article provides important practical tips on the treatment of hypertension and blood pressure control for dyslipidemia.
Keywords: Dyslipidemia, Cholesterol, Arterial hypertension, Monitoring
Cite this paper: D. A. Ochilova, N. G. Rakhmonkulova, Sh. H. Sobirov, Features of the Course of Hypertension Disease in People with Dyslipidemia, American Journal of Medicine and Medical Sciences, Vol. 10 No. 2, 2020, pp. 77-80. doi: 10.5923/j.ajmms.20201002.02.
1. Introduction
- Arterial hypertension (AH) and various metabolic disorders are some of the most important problems of modern medical science and healthcare. According to WHO, 20-30% of the world population have hypertension. AH is the second most common cause of death from cardiovascular disease after coronary heart diseases. According to a number of studies conducted in Japan, Uzbekistan and Finland, the development and progress of hypertension are closely related to such important factors as dyslipidemia, nervous stress, excessive salt intake, overweight, age, gender, and disorder of glucose tolerance. In people with hypertension, lipid metabolism disorders are several times more common [1,4].Disorders of lipid metabolism play a major role in the development of cardiovascular complications in patients with hypertension. Many epidemiological studies have found a clear link between hypertension and lipid metabolism disorders [6]. Arterial hypertension is more stable in patients with impaired lipid metabolism. The risk of myocardial infarction (MI) is increased 2,5 times in patients with specific AH, 16 times in patients with impaired lipid metabolism, and 20 times in patients with impaired AH and lipid metabolism [3]. Assessment of the importance of dyslipidemia for the development of hypertension and coronary heart disease in recent years has focused on the lipid triad (hypercholesterolemia, hyper- b-lipoproteinemia, a-hypolipoproteinemia). In some populations, the prevalence of lipid metabolism disorders, especially hypercholesterolemia, reaches 60% [5]. A number of studies have shown that there is a direct relationship between hypercholesterolemia and blood pressure, glycemia and body weight. Currently, the role of dyslipidemia, its regional and age-related features in the choice of origin, development and adequate treatment of arterial hypertension requires a number of scientific studies [2].
2. Materials and Methods
- The study was conducted in 134 patients with arterial hypertension (WHO 1999) aged 20–69 years, receiving treatment in the Bukhara Regional Cardiology Clinic. In all patients, lipid metabolism levels (cholesterol, triglyceride, low density lipoproteins, high density lipoproteins and Klimov's atherogenic index (atherogenic index of plasma smaller than 4 in the norm) were determined. After the examination, the patients were divided into 2 groups: The main group (76 patients) - a group of patients with dyslipidemia. The control group (58) was a group of patients with a normal level of lipid metabolism. Patients in both groups were given daily blood pressure monitoring (DBPM). Based on the results of DBPM, the features of arterial hypertension were studied in patients with dyslipidemia.
3. Results and Their Analysis
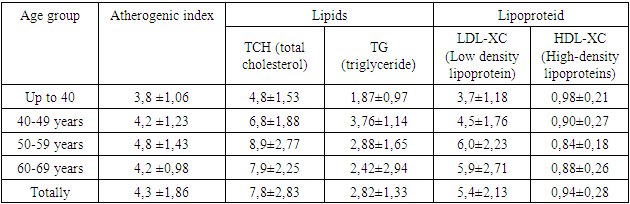
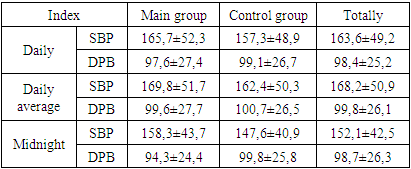
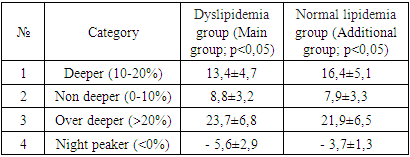
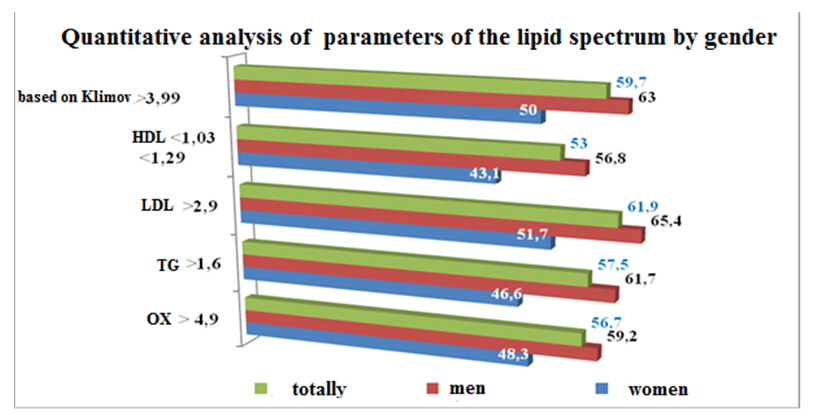
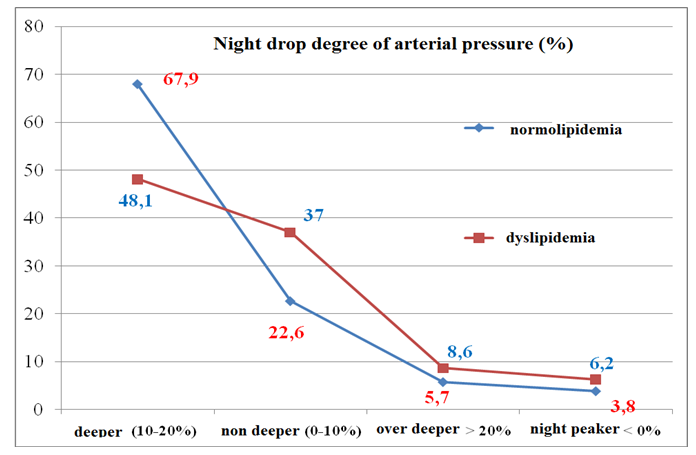
- During the study, 134 patients were treated in the department of arterial hypertension and coronary heart disease and arrhythmia of the Bukhara Regional Cardiology Center. The significance of lipid metabolism disorders in patients (76 men and 58 women) was studied. Among the patients with hypertension, dyslipidemia was 60,4%. (63,2% for men and 56,9% for women). The highest rates were observed for women in the age group of 40–49 years (58,3%) and in the age group of 50–59 years (64%). The incidence of dyslipidemia in different age groups ranged from 44,4% (up to 40 years), 64% (50–59 years), among women 47,4% (60–69 years), 58,3% (40%). 49 years old).In the analysis of hyperlipoproteinemia, the increase in LDL was 65,4% for men, 51,7% for women and 61,9% for all patients. The decrease in HDL was 56,8%, 43,1% and 53%, respectively. Klimov's atherogenic index denoted the degree of was higher than normal in 63% of men, 50% of women, and 59,7% of all patients.In a quantitative analysis of all parameters of the lipid spectrum, one can see an increase in the number of atherogenic fractions (TCH, TG, and LDL). The average TCH content is 7,8 mmol / l (2,9 mmol / l more than normal), the average TG is 2,82 mmol / l (1,12 mmol / l more than normal), the average LDL is 5,4 mmol / l. Ll (2,4 mmol / l more than normal), the amount of HDL (high-density lipoproteins) was 0,94 mmol / l (normally less than 0,34 mmol / l).Studies show that lipid metabolism disorders are significantly higher among patients with Hypertension disease. Although dyslipidemia is more common in men, it increases significantly in women, especially after 50 years (in post-climatic periods).Although one indicator is clearly high in the characteristics of dyslipidemia, the normality of the other indicators was not confirmed in our studies. In most cases, we observed that all parameters of the lipid spectrum deviate identically. An increase in the atherogenic fraction of lipid metabolism products additionally accelerates the development of atherogenesis. Although an increase in TCH of 1,89 times and LDL 2 times than norm was significant after 50 years, it was found that TG increased 2,23 times after 40 years. This requires a deeper approach to the problem and the development of early and effective remedies.To study the effect of dyslipidemia on the correction of blood pressure, we performed daily monitoring of blood pressure in patients. When analyzing the average daily blood pressure of patients, 53,1% of patients diagnosed with dyslipidemia were diagnosed with an AH level of 1, 33,3%, a degree of AH and 13,6% of a 3 degree of AH. In the control group, patients without lipid metabolism disorders reported 62,3% of hypertension of the 1st degree, 28,3% of hypertension of the 2nd degree and 9,4% of hypertension of the 3rd degree.
 | Diagram 1 |
|
|
 | Diagram 2 |
|
4. Conclusions
- 1. It was noted that lipid metabolism disorders were significantly higher among patients with HA.2. In most cases, all parameters of the lipid spectrum deviate, atherogenic fractions of lipid metabolism products – 1,89 times compared with TCH, LDL - 2 times, TG – 2,23 times, require a deeper approach to the problem and the development of early and effective correction methods.3. Dyslipidemia significantly affects negatively to the effective control of blood pressure (especially systolic blood pressure).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML