Kurbaniyazov Zafar Babajanovich, Babajanov Axmadjan Sultanbayevich, Zainiev Alisher Faridunovich, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich
Samarkand State Medical Institute, Uzbekistan
Correspondence to: Davlatov Salim Sulaymonovich, Samarkand State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Material and research methods. The study is based on the results of treatment of 368 patients with thyroid nodular lesions, admitted to the surgical department of the 1st clinic of the Samarkand State Medical Institute from 2005 to 2018. Patients are conditionally divided into two groups. In 2005-2013 operated on 230 patients who made up the comparison group. From 2014 to 2018 under our supervision were 138 patients who entered the main group. The results of the study. Surgical tactics and techniques for performing the main stages of a stumectomy did not differ from the generally recognized. In order to properly carry out the surgical intervention during thyroid nodular lesions and to avoid complications and relapses after the operation, the basic principles of strumectomy were observed. In the main group, the choice of treatment was more differentiated. Factors affecting the choice of treatment were taken into account. As indicated in chapter III in the late postoperative period, the unsatisfactory results in the comparison group were due to the neglect of the cytological conclusion and the choice of surgical tactics. Conclusions. The developed program for the scoring of factors affecting the choice of surgery in patients with thyroid nodular lesions allowed to choose the optimal method of surgery, taking into account the individual characteristics of the body and improved treatment outcomes. To prevent intraoperative complications, one of the innovative solutions in patients in the main group was the use of a modified retractor tool.
Keywords:
Nodular goiter, Thyroidectomy, Relapse, Iodine deficiency
Cite this paper: Kurbaniyazov Zafar Babajanovich, Babajanov Axmadjan Sultanbayevich, Zainiev Alisher Faridunovich, Rakhmanov Kosim Erdanovich, Davlatov Salim Sulaymonovich, Factor Analysis of Relapse of Nodular Goiter, American Journal of Medicine and Medical Sciences, Vol. 10 No. 1, 2020, pp. 59-65. doi: 10.5923/j.ajmms.20201001.13.
1. Relevance
Currently, one of the most urgent is the problem of surgical treatment of patients with nodular goiter. This is primarily due to the development of relapses in the postoperative period. There are supporters of radical and organ-preserving operations. When conducting organ-preserving operations, researchers indicate the need to preserve part of the gland tissue to prevent postoperative hypothyroidism, which will avoid taking thyroid drugs [2]. Supporters of radical surgeries consider organ-preserving surgeries unreasonable, since this increases the risk of a relapse of the disease up to 25-40% [1,4].A number of authors note the occurrence of relapse of nodular non-toxic goiter in 5.8% of cases [7]. In 68% of cases, relapse occurred after the initial surgical intervention, where the volume of the operation did not exceed the resection of one or both lobes of the thyroid gland; in 16% of cases, relapse was detected after radical surgery, but was subsequently associated with a different morphological form of goiter, more severe than initially [5]. Some authors argue that in the pathogenesis of relapse, the main role is played not by the volume of the operation performed, but by the etiology and morphological structure of the nodal formation [3]. The lack of a single point of view on the factors determining the risk of postoperative relapses with nodular goiter served as the basis for the study. that in the pathogenesis of relapse, the main role is played not by the volume of the operation performed, but by the etiology and morphological structure of the nodal formation [3,6].The lack of a single point of view on the factors determining the risk of postoperative relapses with nodular goiter served as the basis for the study. that in the pathogenesis of relapse, the main role is played not by the volume of the operation performed, but by the etiology and morphological structure of the nodal formation [3]. The lack of a single point of view on the factors determining the risk of postoperative relapses with nodular goiter served as the basis for the study.
2. Purpose of the Study
Identification of factors affecting the incidence of recurrence of nodular goiter.
3. Material and Research Methods
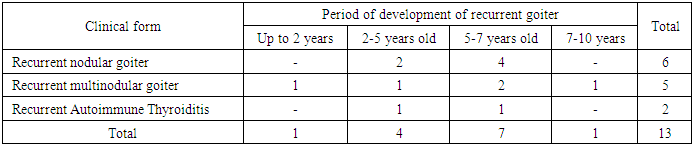
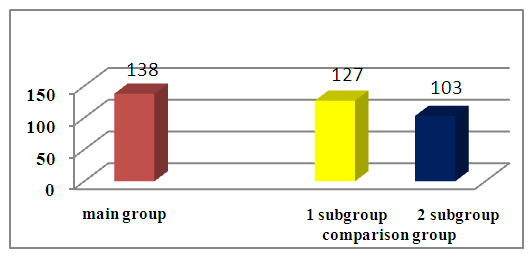
The study is based on the results of treatment of 368 patients with thyroid nodular lesions (ThNL), admitted to the surgical department of the 1st clinic of the Samarkand State Medical Institute from 2005 to 2018.Patients are conditionally divided into two groups. In 2005-2013 operated on 230 (62.5%) patients who made up the comparison group. From 2014 to 2018 under our supervision were 138 (37.5%) patients who entered the main group. Depending on the choice of the volume of surgical intervention, patients of the comparison group are conditionally divided into two subgroups. The 1st subgroup consisted of 127 (55.2%) patients who were operated on from 2005 to 2009. Subgroup 2 comprised 103 (44.8%) patients who were operated on from 2010 to 2013. (Fig. 1.). 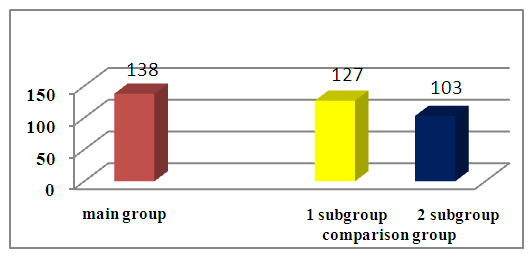 | Figure 1. The distribution of patients in groups (n = 368) |
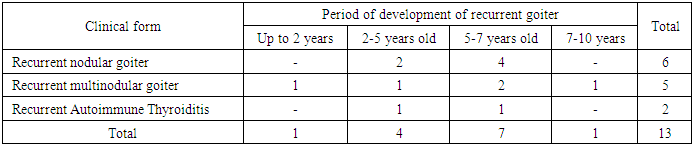
Of 368 patients, 35% (96.5%) of patients with ThNL were diagnosed for the first time and goiter was recurrent in 13 (3.5%) of patients. Of these, 8 patients had a primary relapse. Of 8 patients, 3 patients underwent the first operation in our clinic in different years. 4 patients had a history of two operations, and 1 patient had three operations in another hospital.Postoperative recurrent goiter was detected in the period up to 10 years, with the main number in terms of up to 5 years in 17 (47.2%) patients and from 5 to 10 years in 19 (52.8%) patients (Table 1).Table 1. Distribution of patients depending on the period of development of postoperative recurrent goiter
 |
| |
|
All patients underwent general clinical examination, including palpation of the thyroid gland, auscultation of the heart and blood vessels. When examining the front of the neck, we focused on the external contours and sizes of thyroid formations.All patients underwent a comprehensive examination, including generally accepted laboratory tests (general analysis of blood, urine, biochemical blood analysis, prothrombin index and time, IFA of blood), the level of thyroid harmonics (T3, T4 and ThH) was determined at baseline and at various times after operations. The instrumental diagnostic methods used (chest x-ray, ultrasound, CT, ECG) were used to identify the differential and topical characteristics of the USG. All patients underwent cytology of thyroid formations; histology of the removed preparation was performed to all patients.Successful radical stumectomy largely depends on the right surgical tactics, which significantly affects the course of the operation and has a certain value in the outcome of surgical treatment, is reflected in the course of the rehabilitation period.In the main group, the choice of treatment was more differentiated. Factors affecting the choice of treatment were taken into account. As indicated in chapter III in the late postoperative period, the unsatisfactory results in the comparison group were due to the neglect of the cytological conclusion and the choice of surgical tactics. We evaluated these factors that affected the treatment results on a scale (certificate of state registration of a computer program No. DGU 05147, Intellectual Property Agency of the Republic of Uzbekistan) (Table 2).Table 2. The scoring system for choosing a method for the treatment of pathological thyroid formations
 |
| |
|
Patients with a total score of up to 9 underwent hemithyroidectomy or resection of one lobe of the thyroid gland. This group consisted of patients who, as a rule, had small nodular formations (diameter up to 6 cm) of the thyroid gland without proliferative cells during puncture and rapid biopsies. Patients with the number of points from 10 to 12 s of ThNL were treated with an extremely subtotal thyroid resection. Patients with a scored score of more than 12 who had foci of adenomatosis during puncture and rapid biopsies or underwent total thyroidectomy with varying degrees of thyroid tissue proliferation (Table 3).Table 3. Distribution of patients of the main group depending on gender, age and type of treatment
 |
| |
|
The developed program for the scoring of factors affecting the choice of surgery in patients with ThNL allowed to choose the optimal method of surgery taking into account the individual characteristics of the body and improved treatment results.On the basis of the clinical course of the disease and the program for determining the choice of surgical tactics for ThNL, we have developed and implemented in clinical practice the optimal therapeutic and tactical algorithm for the management of patients with ThNL.
4. The Results of the Study
Surgical tactics and techniques for performing the main stages of a stumectomy did not differ from the generally recognized. In order to properly carry out the surgical intervention during ThNL and to avoid complications and relapses after the operation, the basic principles of strumectomy were observed. Patients were placed on the operating table with a “roller” placed under the shoulder blades in order to hyperextension the neck, in which the goiter sharply protruded (Fig. 2).  | Figure 2. Neck hyperextension with the help of a “roller” placed under the shoulder blades |
Used a classic skin incision according to Kocher (Fig. 3). It was carried out lower, 2 cm above the edge of the sternum handle, along the lower skin fold of the neck. The incision line was indicated by lightly scratching the skin with a needle before the operation itself.  | Figure 3. Kocher skin incision line |
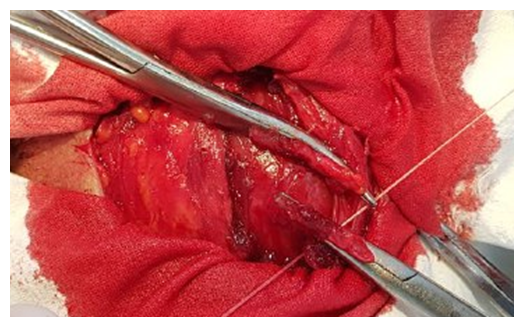
Further, in order to gain wide access to the gland, cervical skin flaps were dissected together with the cutaneous muscle of the neck and saphenous veins up to the thyroid cartilage, and down to the upper edge of the sternum (Fig. 4). Since this maintains lymphatic circulation in the subcutaneous tissue, postoperative edema in skin flaps was avoided.  | Figure 4. Preparation of skin flaps |
Then the third cervical fascia was crossed longitudinally along the midline of the neck, and with the help of two anatomical tweezers, the sternum-hyoid and sternum-thyroid muscles were peeled off. They were dissected high between the two clamps of Kocher, close to the place of their attachment to the thyroid cartilage, which helped to avoid injury to the arteries feeding them and the branches of the hyoid nerves innervating them. This prevented the development of postoperative atrophy of these muscles, which could cause neck deformation. With large sizes and multiple ThNL, the sternum-hyoid and sternum-thyroid muscles were transversely crossed (Fig. 5). 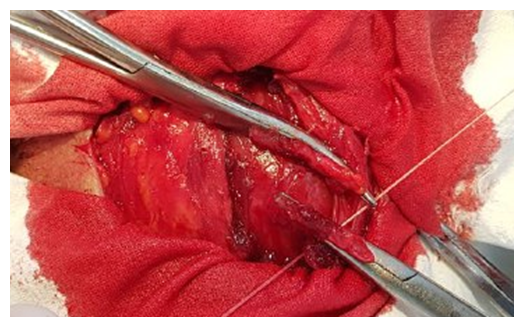 | Figure 5. Transverse intersection of the prethyroid muscles |
In practice, in thyroid surgery, in order to provide access to the gland, the thyroid muscles are removed in the cranial and caudal direction with the help of special dilators - Farabef or Vorobyov’s instrument. This does not allow a full examination of the gland and work more calmly without intraoperative complications.To prevent the above mentioned inconveniences, one of the innovative solutions in patients in the main group was the use of a modified retractor tool (Fig. 6).  | Figure 6. The retractor for thyroid surgery |
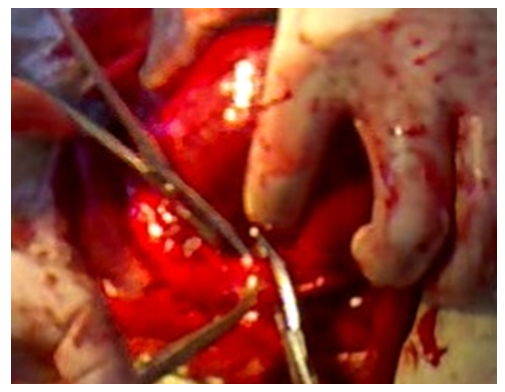
The retractor provided wide access to the thyroid gland, which made it possible to conduct a full examination and work more quietly, without injuring the gland. The surgical instrument we developed created favorable conditions for the detection of all thyroid nodes, avoiding damage to the recurrent nerves and other important vessels and nerves in the vicinity of the gland.The retractor belongs to surgical instruments and is used to provide access to the organs of the neck by abducting and fixing the edges of the wound. The device is a structure consisting of a tetrahedral curved crossbar, on which two sliders with curved brackets rigidly fixed on them are worn. The sliders are equipped with clamping screws for fixing them on the crossbar in the desired position. Two semicircular hooks with a width of 1 cm and a radius of curvature of 1.3 cm are installed on the brackets. The hooks distal from the crossbar are rigidly fixed to the bracket. The proximal hooks on the bracket can be moved along the bracket and rotated around the axis of the bracket. The clamping screws of the hooks allow you to fix them on the bracket in the desired position. The technical result is the provision of a good overview during surgical intervention.The device is simple and easy to use. It is recommended for widespread use in practical surgery, especially in the surgical treatment of ThNL, since contributes to a full review of the surgical wound, without the risk of intraoperative complications, which facilitates the work of the surgeon.Next, they began to isolate the thyroid vessels. The loose connective tissue located in front of the trachea and under the caudal surface of the isthmus of the thyroid gland was pushed out with a swab. As a result, the inferior thyroid veins became visible, which were bandaged and dissected (Fig. 7).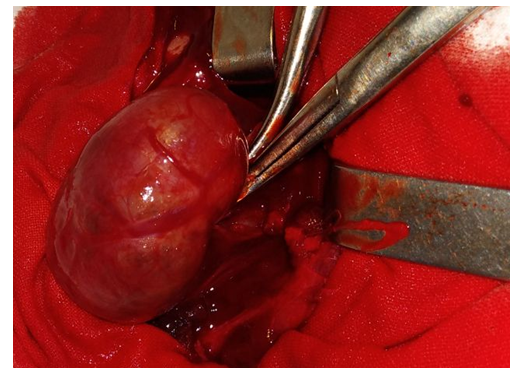 | Figure 7. Bandaging and crossing of the thyroid vessels |
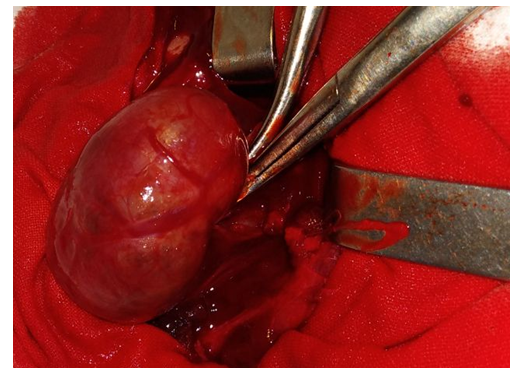
In case of diffuse goiter or multiple ThNL, in order to ensure wide release of the anterior surface of the trachea, the thyroid isthmus was crossed (Fig. 8). | Figure 8. Ligation and intersection of the isthmus of the thyroid gland |
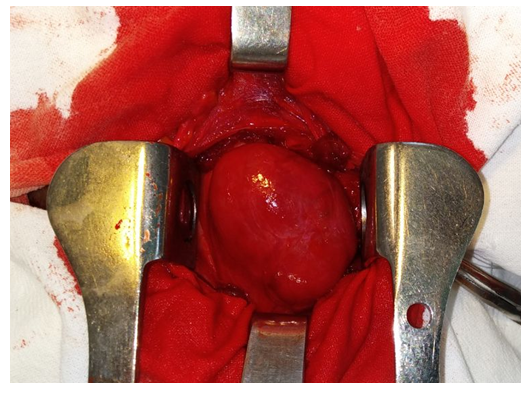
The isthmus was dissected from the trachea by cutting with a scalpel the parietal leaf IV of the cervical fascia in the area between it and the cricoid cartilage, where it condenses and forms the median shield-hyoid ligament. The intersection of this ligament facilitated the separation of the isthmus. To do this, with the help of a Kocher or Pean probe, they carefully entered the space between the trachea and the posterior surface of the isthmus, trying not to injure the parenchyma of the gland, which is bleeding and makes it difficult to prepare.After introducing the probe using a Deschan needle, two silk threads were sequentially drawn between the isthmus and the anterior surface of the trachea. The ends of the threads after flashing the corresponding lobe of the gland were tied on the front surface of the isthmus. It was cut with a scalpel between the two ligatures, and the probe inserted under it protected the trachea from injury.It should be noted that the stages of isolation of the thyroid vessels and the widespread release of the anterior surface of the trachea are one of the difficult stages of a stumectomy. However, the use of the proposed tool greatly facilitated the stages of the operation. As a result, the period of complex stages was reduced from 15.8±0.9 to 6.7±0.5 minutes (p <0.001). Accordingly, the total operation time decreased from 92.7±4.8 to 63.4±3.6 minutes (p <0.001) (Fig. 9). 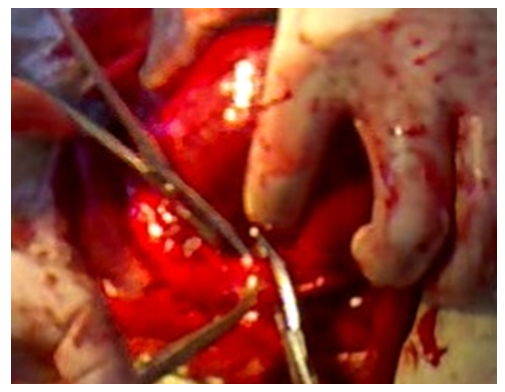 | Figure 9. Thyroid mobilization |
Thus, in almost 40% of cases in thyroid surgery, goiter occurs in a multinodular and diffuse form, while the use of the developed tool made it possible to mitigate the risk of intraoperative complications, such as bleeding, damage to the trachea and recurrent laryngeal nerve.The mobilization of the thyroid gland is an essential stage of a stumectomy, which allows you to free the lobes of the gland, to provide the opportunity for a full view of the entire gland and to decide the scope of the operation. Having liberated the lobes of the gland from the vessels and its connections with the neighboring structural elements of the neck, a thorough examination and palpation of the gland was carried out. A mobilized thyroid gland makes it possible to easily distinguish a multinodular formation from a single adenoma located inside one of its lobes. Thyroid resection was performed at a level where pathological changes in the parenchyma were not felt.After the main stage of the operation, thorough hemostasis was performed. The resected thyroid lobes were flashed with monofilament thread, which contributed to their encapsulation. The cut pre-thyroid muscles were restored in layers (Fig. 10). Then an intradermal cosmetic suture was applied (Fig. 11). | Figure 10. The restoration of the integrity of crossed prethyroid muscles |
 | Figure 11. Intradermal cosmetic suture on the skin |
In the main group, the choice of treatment was more differentiated. Factors affecting the choice of treatment were taken into account. As indicated in chapter III in the late postoperative period, the unsatisfactory results in the comparison group were due to the neglect of the cytological conclusion and the choice of surgical tactics.The results of surgical treatment in the early postoperative periodThe results of surgical treatment of ThNL in patients were evaluated by the following indicators: bleeding during and in the postoperative period, during the postoperative period, the presence of signs of paresis of the recurrent laryngeal nerve, the presence of seizures, the nature of healing of the surgical wound, the length of hospital stay (bed day), duration operations (min), duration of temperature (days), signs of perotracheal and subcutaneous hematomas according to ultrasound, relapses and residual cysts.Improvement of the choice of tactics for surgical treatment of ThNL, the technique of performing surgical intervention, reducing the morbidity of surgical access, and other innovations developed and implemented in the framework of this study, could not but affect the direct results of this category of patients. So, compared with 2005-2008. the incidence of postoperative complications decreased from 29.1 to 5.1%, i.e. 6 times (table. 4). Complications such as bleeding (5 times), paresis of the recurrent laryngeal nerve (3 times), hypoparathyroidism (9 times) were much less common, there were no formidable complications such as persistent paralysis of the recurrent laryngeal nerve and asphyxiation.Table 4. The incidence of postoperative complications in patients with ThNL
 |
| |
|
The expansion of indications for radical interventions, an intraoperative express biopsy, if necessary, the application of cosmetic sutures on the skin did not adversely affect the duration of the surgery. On the contrary, this indicator decreased. The duration of inpatient treatment after surgery decreased by 2 times compared with the 1st subgroup of the comparison group - from 10.2 ± 1.2 to 5.9 ± 0.3 days.Long-term results were analyzed in 268 (72.8%) of the 368 patients operated on for ThNL. Patients were called in an active way, with the help of letters, and the archival material of the 1st clinic of the Samarkand State Medical Institute was also studied. The history of the disease has been carefully studied. Particular attention was paid to the duration of the disease, drug treatment with thyroid hormones after surgery. We studied such indicators as the volume of the operation, complications, outcomes, immediate and long-term results of the surgical treatment of thyroid diseases.Of 268 patients examined at a long time, a relapse of ThNL was observed in 25 (9.3%) patients, while in the group of patients operated on in 2005-2009, this indicator reached 24.1% (Table 5). Subsequently, due to the use of the above innovations and disease prevention measures, the recurrence rate of the disease was reduced in the 2nd subgroup of the comparison group to 4.0%, and in the main group to 0.9% (criterion χ2 = 4.692; p = 0.031).Table 5. Recurrence rate of ThNL
 |
| |
|
5. Conclusions
Improvement of the choice of tactics for surgical treatment of ThNL, the technique of performing surgical intervention, reducing the morbidity of surgical access, and other innovations developed and implemented in the framework of this study, could not but affect the direct results of this category of patients. So, compared with 2005-2008. the incidence of postoperative complications decreased from 29.1 to 5.1%, i.e. 6 times.The developed program for the scoring of factors affecting the choice of surgery in patients with ThNL allowed to choose the optimal method of surgery, taking into account the individual characteristics of the body and improved treatment outcomes.To prevent intraoperative complications, one of the innovative solutions in patients in the main group was the use of a modified retractor tool. The use of the proposed tool greatly facilitated the stages of the operation. As a result, the period of complex stages was reduced from 15.8±0.9 to 6.7±0.5 minutes (p <0.001). Accordingly, the total operation time was reduced from 92.7±4.8 to 63.4±3.6 minutes (p <0.001).
References
| [1] | Boutzios G. et al. Long-term sequelae of the less than total thyroidectomy procedures for benign thyroid nodular disease //Endocrine. – 2019. – Т. 63. – №. 2. – С. 247-251. |
| [2] | Barczyński M. et al. Ten-year follow-up of a randomized clinical trial of total thyroidectomy versus Dunhill operation versus bilateral subtotal thyroidectomy for multinodular non-toxic goiter //World journal of surgery. – 2018. – Т. 42. – №. 2. – С. 384-392. |
| [3] | Mekel M. et al. Negative fine-needle aspiration in patients with goiter: should we doubt it? //World journal of surgery. – 2016. – Т. 40. – №. 1. – С. 124-128. |
| [4] | Sulatanbaevich B. A. et al. Analysis of the results of surgical treatment of patients with thyroid nodules // Voprosy nauki i obrazovaniya. – 2019. – №. 4 (49). |
| [5] | Yusupov S. A. et al. Otdalennyye rezul'taty operativnogo lecheniya uzlovykh obrazovaniy shchitovidnoy zhelezy // Zdobutki clinical and experimental medicine. – 2017. – №. 1. |
| [6] | Yusupov S. A., Kurbaniyazov Z. B., Zayniev A. F. Вузлові утворення щитоподібної залози. стан проблеми (Огляд літератури) //Вісник наукових досліджень. – 2018. – №. 1. |
| [7] | Zatelli M. C. et al. Thyroid nodule recurrence following lobo-isthmectomy: incidence, patient’s characteristics, and risk factors //Journal of endocrinological investigation. – 2018. – Т. 41. – №. 12. – С. 1469-1475. |









 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML