-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(1): 49-54
doi:10.5923/j.ajmms.20201001.11

Using Virtual 3D Modeling in Clinical Application for Orbital Floor and Wallfractures
Sh. A. Boymuradov, Sh. Sh. Yusupov
Tashkent Medical Academy, 2, Farobiy str., Tashkent, Uzbekistan
Correspondence to: Sh. A. Boymuradov, Tashkent Medical Academy, 2, Farobiy str., Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Orbital floor fractures or zygomatic orbital fractures are the most commonly encountered midfacial fractures. The technological advances in 3D printing allow the physical prototyping of 3D models, so it creates an accurate representation of the patient's specific anatomy. Surgical treatment of such fractures with the aid of pre-shaped, customized prosthesis based on the 3D anatomical model resulted in significant aesthetic and clinical improvement. It is possible to build anatomical models based on the computed tomography scan dataset. It is relatively inexpensive and can be used in the repair of the orbital floor and zygomatic orbital fractures.
Keywords: Orbital floor, 3D computed tomography, 3D model, Zygomatic orbital complex
Cite this paper: Sh. A. Boymuradov, Sh. Sh. Yusupov, Using Virtual 3D Modeling in Clinical Application for Orbital Floor and Wallfractures, American Journal of Medicine and Medical Sciences, Vol. 10 No. 1, 2020, pp. 49-54. doi: 10.5923/j.ajmms.20201001.11.
Article Outline
1. Introduction
- Despite the improvement of technologies and modernization of equipment, treatment of fractures of the zygomatic orbital complex occupies the 2nd place after fractures of the lower jaw and 1st place among the injuries of the middle zone of the face. The trauma of the orbit with the involvement of the organ of vision and its auxiliary organs among all injuries of the facial skeleton ranges from 36 to 64% [1-4]. Despite the successes achieved in the prevention and treatment of injuries of the zygomatic orbital complex, blunt trauma of the orbit with damage to its walls remain a topical problem of modern maxillofacial surgery. Injuries to the orbital floor are commonly encountered among surgeons affiliated with trauma centers that treat facial injuries. Creation of computed tomography, development of methods of visualization of various organs and systems of the person have expanded representations of clinicians about their vital topographic anatomy. Introduction to clinical practice of computer diagnostics considerably improved diagnostics, allowed to carry out investigations in case of serious condition of injured in acute period of trauma, to determine localization and prevalence of bone destruction tissue, to reveal the topographic connection of the orbital fracture with the clauses sinuses of the nose and cavity of the skull [2,3,8-10]. Over the past 20 years, advances in radiographic imaging and computer technology have allowed for the application of image-guided surgery in orbital floor reconstruction. One of the perfect methods of diagnosis and treatment planning is 3D-reconstruction, which precisely determines the nature and localization of trauma. The construction of three-dimensional graphics models was based on the receipt at the minimum intervals of time X-ray computer tomograms, allowing to create a textured segmentation and three-dimensional reconstruction of organs. 3D technologies are advanced technologies that fill modern human life. 3d modeling is the basis of 3D technology. Today it is difficult to imagine the work of the designer without the use of 3D models built. Even more widespread 3D modeling has received in connection with the distribution of 3D printers. Now, 3D models are used in all fields of science, technology, medicine, commercial and managerial activities [6,7]. The method of computer-aided three-dimensional modeling of the zygomatic orbital complex taking into account their reference points, deformations, and defects, as well as the necessary grafts is based on the use of computed tomography as a background for modeling nodes three-dimensional lattice. This method of transplant modeling facilitates the reconstruction of the deformed orbit, increases the accuracy of the positioning and the overall efficiency of the operation [1,3].Conversely, volumetric analyses of anatomical structures have been utilized for the design of standardized anatomic implants for orbital reconstruction and custom patient-specific implants (PSI) for orbital floor and zygomatic orbital defects. These advances have allowed for improved efficiency, accuracy, and safety in the surgical management of orbital pathology [5,8,10].
2. The Purpose of the Study
- Improvement of diagnostics, planning and surgical treatment of patients with orbital floor and zygomatic orbital fractures using virtual 3D modeling.
3. Research Materials and Methods
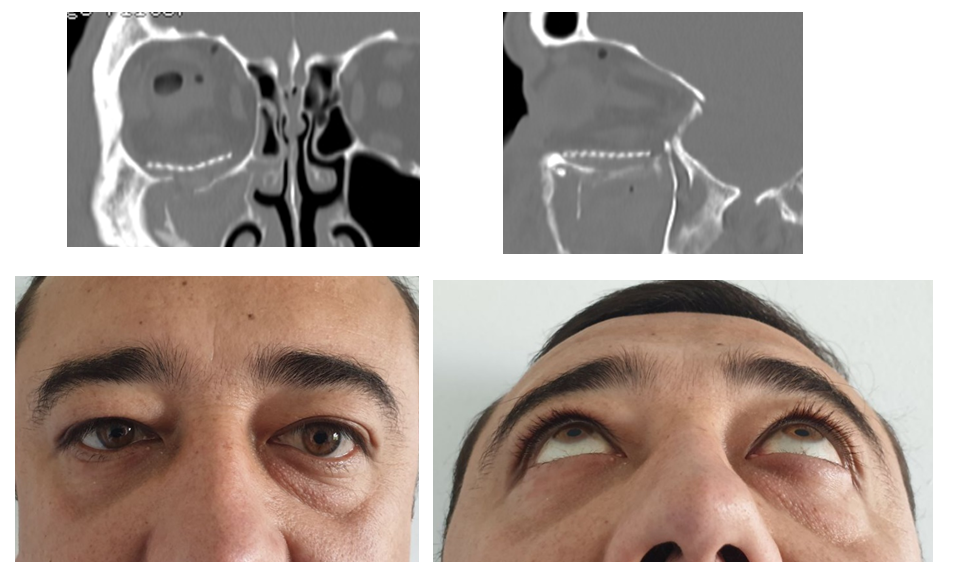
- In the Department of Plastic Surgery of the 2nd Clinic of the Tashkent Medical Academy were operated 36 patients with the fractures of the orbital floor and zygomatic orbital complex (ZOC) in the period from 2015 to 2018. Male were – 24 patients (67%), female – 12 (33%). The age of patients varied from 20 to 50 years. The reason for such injury was road accident in 18 cases (49%), in 6 cases (17%) - street fight, in 6 cases (17%) - injury at work, in 6 cases (17%) - household injury. Orbital floor injuries may occur in isolation or in conjunction with higher-level Le Fort injuries, ZOC fractures, naso-orbital-ethmoid fractures, panfacial trauma, and often occur with fractures of the medial orbital wall. Patients received a comprehensive clinical examination, consultation of related specialists-neurosurgeon, ophthalmologist, otolaryngologist, etc. All patients performed a multi-spiral computed tomography with 3D-reconstruction in three projections. Scanning is carried out in an automatic mode under the special program established in computer support of a tomograph. To determine the defect condition of the orbital floor, sections were taken in all planes with a collimation layer of 0.5 mm, a reconstruction interval of 0.5 mm with a multispiral reconstruction of the images obtained in sagittal and coronary projections (Fig. 1). Planning of surgical elimination of post-traumatic defect of bones of the bottom wall of an orbit is the virtual computer 3D modeling by the special computer program by which it is possible to define precisely character and localization of defect and deformation, simulate a surgical pattern and an individual implant. The primary goal for orbital reconstruction is to restore the premorbid orbital volume. In this regard, image-guidance technology has been useful for the design of anatomic orbital implants.
 | Figure 1. Computer tomography image of the right orbit with coronary and sagittal plane. Damaged orbital floor |
4. Research Results
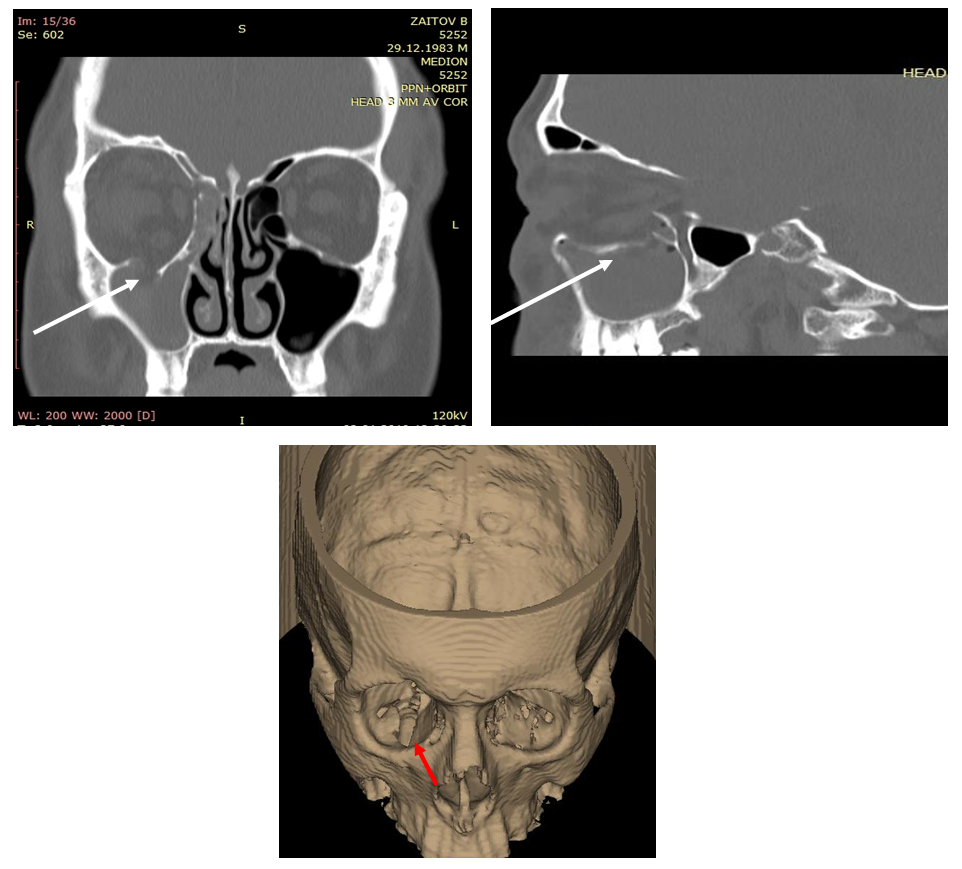
- Post-traumatic deformation of the zygomatic orbital complex with the defect of the orbital floor in 11 cases (30%). Isolated post-traumatic defects of the orbital floor were diagnosed in 25 cases (70%). Fracture prescriptions ranged from 2 weeks to 6 months. All patients in the preoperative period had all the symptoms of posttraumatic deformation of the orbital floor and zygomatic orbital complex (fig. 2). The virtual 3D model of the orbital floor and zygomatic orbital complex with stereolithographic intraoperative template and the implant printed on the 3D printer was made for all patients in the preoperative period. Model production by rapid prototyping: CT data were imported into the specialist software and 3D virtual models were created (fig. 3). The unaffected orbit was mirrored onto the contralateral side i.e. the injured orbit. This model contained numerous artifacts which are typical of CT studies because of the very thin bone structures of the orbit. To create a rigid physical model that would be strong enough to be used as a template, all the empty spaces (air) surrounded the mirrored orbit in the virtual model were filled in. This resulted in a virtual model of the orbit that was surrounded by hard tissue only. Next, the virtual model data were converted to STL format and solid physical models were created from the acrylic resin using a 3D printer. The resulting physical models were stronger and more rigid than if they had been built containing hollow structures i.e. maxillary and ethmoid sinuses. Finally, models were sent to the hospital (fig.4,5).
 | Figure 2. Appearance of face, before treatment of right side blow out orbital fracture |
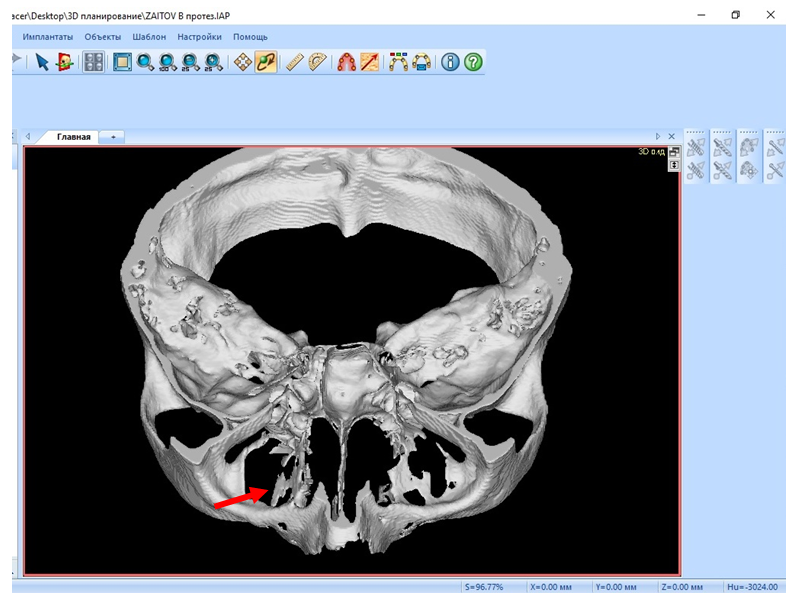 | Figure 3. Virtual model constructed on the basis of DICOM data set |
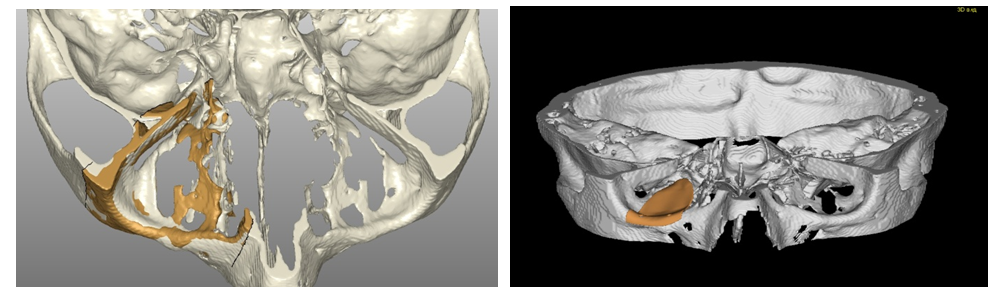 | Figure 4. Determination of the prospective implant’s extent. Implant design |
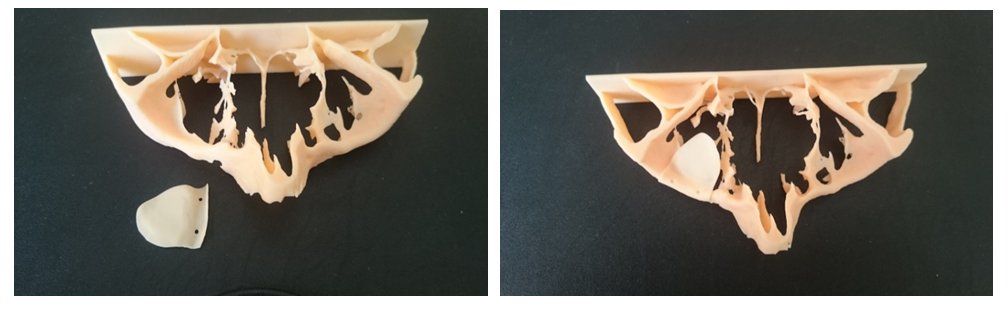 | Figure 5. Solid model of a zygomatic orbital complex with the surgical template |
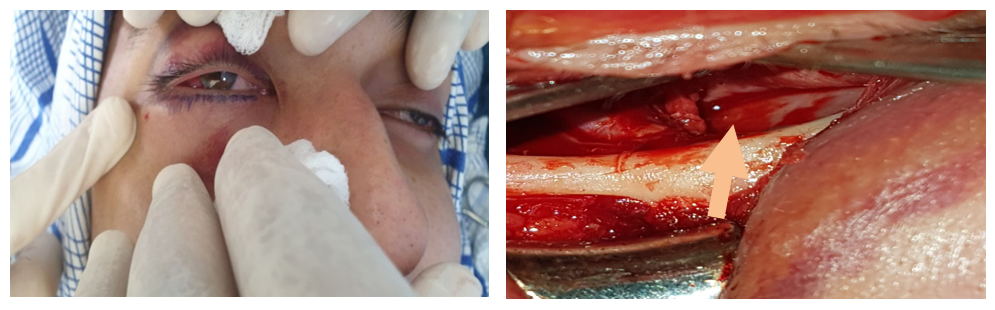 | Figure 6. Subciliary incision. Damaged orbital floor |
 | Figure 7. Solid model of zygomatic orbital complex with individual implant from titanium mesh |
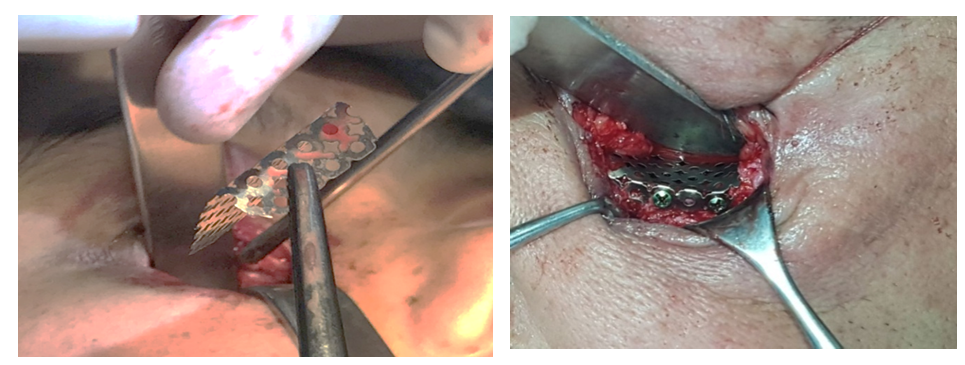 | Figure 8. Right orbital floor reconstructed using individual implant from titanium mesh |
5. Conclusions
- Advances in computer technology and imaging have improved the accessibility and efficacy of orbital reconstruction for defects involving the orbital wall. Due to the complex shape of the internal orbit, proximity of critical soft tissue structures, and small margins of error, the orbital skeleton is an ideal anatomic region for virtual planning. Thus, diagnostics, planning of surgical intervention with the use of computer modeling of defects and deformations of the orbital floor and zygomatic orbital complex with the use of surgical patterns and individual-modeled implants, printed on 3D-printer, reduce the time of surgery and increases the accuracy of planning and implementation of surgical treatment. 3D-planning allows to plan and determine the volume of the operation, selection of the implant, determination of the size and type of the implant, as well as its fixation. This technique helps to reduce the time of surgery and increases the accuracy of planning and implementation of surgical treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML