-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2020; 10(1): 1-4
doi:10.5923/j.ajmms.20201001.01

Efficacy of Newer Surgical Treatment for Purulent Cholangitis
Z. B. Kurbanuyazov, K. B. Saidmuradov
Samarkand State Medical Institute, Samarkand, Uzbekistan
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

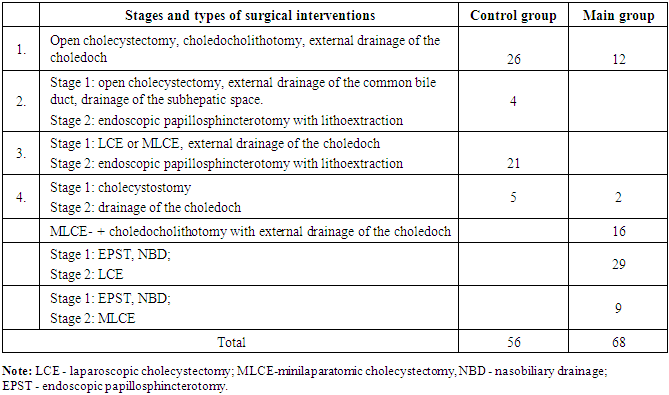
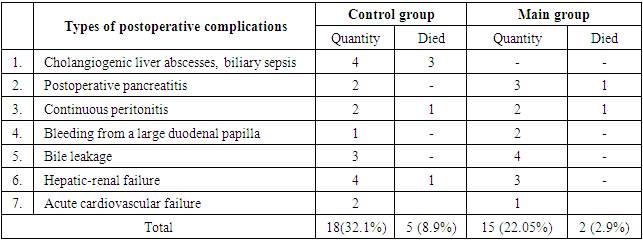
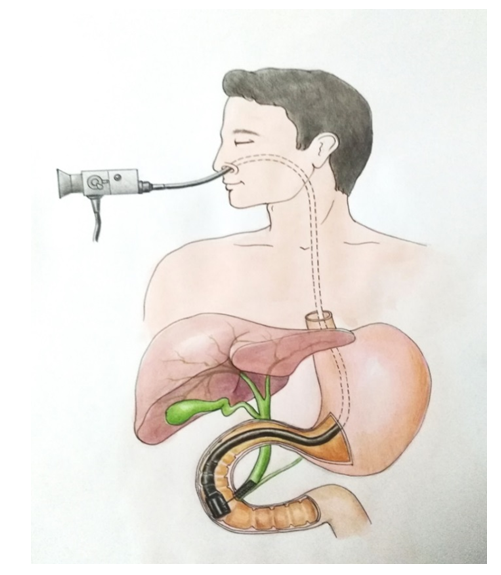
The study was conducted at the clinics of the Samarkand State Medical Institute. We observed 124 patients with cholelithiasis complicated by purulent cholangitis. Most of the patients were women - 95 (76.6%), men were 29 (23.4%). The average age of patients was 45.4 ± 7.3 years. All patients were divided into 2 groups. The comparison group was consisted of 56 patients who received traditional surgical treatment, the main – 68 patients who received the developed surgical treatment. Both groups of patients were approximately the same in age, severity of clinical manifestations and the severity of concomitant diseases. The duration of the biliary system diseases in most patients (78%) was more than 5 years. In the surgical treatment of patients with cholelithiasis complicated by purulent cholangitis, sanitation of the biliary tract with sodium hypochlorite solution helps to prevent the formation of intrahepatic cholangiogenic abscesses and the development of biliary sepsis. A two-stage surgical treatment with sanitation of the bile ducts was used for the successful treatment of patients with cholelithiasis complicated by purulent cholangitis. Endoscopic papillosphincterotomy with lithoextraction and installation of nasobiliary drainage for decompression of the bile ducts was performed as the first stage. Laparoscopic or minilaparatomic cholecystectomy was performed after improving the condition of patients. When the clinic of destructive cholecystitis prevailed, open cholecystectomy and choledocholithotomy were performed with the installation of a drainage tube in the choledoch. For the rehabilitation of the bile ducts in the postoperative period, a 0.06% sodium hypochlorite solution was introduced drop-by-drop through the installed drains. First, an anolyte solution of sodium hypochlorite with pH = 4 was introduced to normalize microflora, then a catholytic solution of sodium hypochlorite with pH = 8. This prevented the occurrence of microabscesses and abscesses of the liver and eliminated inflammation in the bile ducts. Our proposed method allows to stop attacks of cholangitis and favorably affects the postoperative period, helped to reduce postoperative complications from 32.1% to 22.05%, and mortality from 8.9% to 2.9%.
Keywords: Purulent cholangitis, Bile duct sanitation, Microabscesses, Liver abscesses
Cite this paper: Z. B. Kurbanuyazov, K. B. Saidmuradov, Efficacy of Newer Surgical Treatment for Purulent Cholangitis, American Journal of Medicine and Medical Sciences, Vol. 10 No. 1, 2020, pp. 1-4. doi: 10.5923/j.ajmms.20201001.01.
1. Introduction
- Cholangitis is a purulent inflammation of the bile ducts caused by the activation of bacterial microflora that has arisen against the background of the bile outflow violation and is observed in 17-83% of patients with cholelithiasis, Vater papilla stenosis, Mirizzy syndrome. In patients with post-traumatic bile duct strictures and cicatricial anastomotic constriction of biliodigestive anastomoses, cholangitis is detected in more than 80% of cases. Bacteriological studies of bile performed in these cases show that it is infected in 80-100.0% of cases. In this case, gram-negative microflora is most often detected: Escherichia coli, Proteus, blue-green pus bacillus, enterobacteria, etc. Coccal microflora or various associations of microorganisms are more rarely sown [1-5]. The main place in international scientific research on the problems of purulent cholangitis (PC) is occupied by the issues of expanding the medical and diagnostic capabilities of minimally invasive endobiliary technologies. According to many researchers view, a large selection of methods for the treatment of obstructive jaundice of benign origin (OJBO) should reduce the number of postoperative complications and increase the effectiveness of minimally invasive treatment [5-6]. Currently, with the development of non-invasive methods of radiation examination, the use of endoscopic diagnostic techniques is fading into the background, as their implementation can provoke the development of complications such as acute pancreatitis and bleeding. A particular importance is now given to the widespread introduction of magnetic resonance cholangiography, the results of which should dictate further tactics of diagnosis and treatment [6-7]. The development of purulent cholangitis leads to a deterioration in the functional reserve of the liver, multiple organ failure and septic manifestations. These patients require urgent decompression of the biliary tract with the inclusion of reasonable therapeutic measures. Accordingly, patients who have a high risk of surgical treatment should undergo minimally invasive biliary tract (BT) decompression before taking a radical intervention [6-8].The main method of surgical treatment of patients with cholelithiasis complicated by purulent cholangitis is the earliest possible external decompression of the bile duct, by installing drainages and removing stones from the common bile duct [8-9]. It provides the outflow of infected bile to the outside, reducing the severity of obstructive jaundice and endogenous intoxication. Another important element in the treatment of purulent cholangitis is the early administration of antibiotic therapy in accordance with the sensitivity of bile microflora [8-10]. Surgeons prescribe antibiotics both before surgery for drainage of the bile ducts, and in the postoperative period. At the same time, the use of endobiliary administration of drugs as a supplement to them is also known [9-10]. Decompression of the bile ducts, antibiotic therapy and the addition of other antimicrobial effects to it do not exclude the occurrence of complications such as liver abscesses, liver failure and sepsis. Aim of the study is to prove the efficacy of our developed new treatment method for the patients with purulent cholangitis.
2. Material and Methods
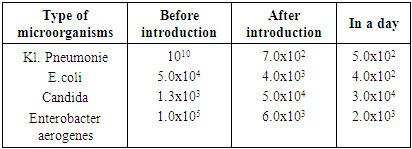
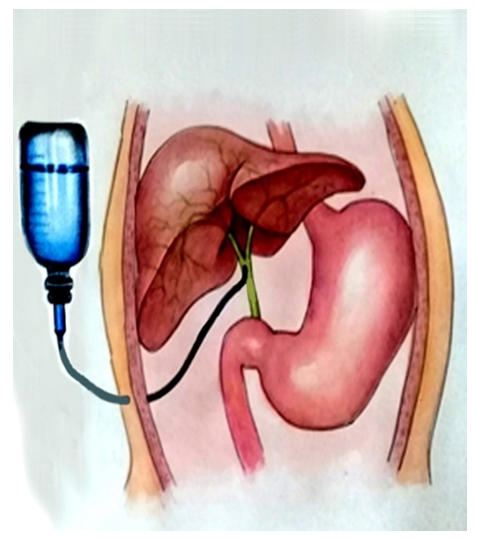
- The study was conducted at the clinics of the Samarkand State Medical Institute. We observed 124 patients with cholelithiasis complicated by purulent cholangitis. Most of the patients were women - 95 (76.6%), men were 29 (23.4%). The average age of patients was 45.4 ± 7.3 years. All patients were divided into 2 groups. The comparison group was consisted of 56 patients who received traditional surgical treatment, the main – 68 patients who received the developed surgical treatment. Both groups of patients were approximately the same in age, severity of clinical manifestations and the severity of concomitant diseases. The duration of the biliary system diseases in most patients (78%) was more than 5 years. The features of surgical treatment of patients in both groups were as follows: the timing, type and extent of the surgery were selected based on the severity of acute cholecystitis signs, local or widespread peritonitis, the presence and severity of obstructive jaundice, signs of cholangitis, the age of patients, the severity of concomitant diseases and the general condition of patients. In case of destructive cholecystitis with peritonitis, emergency surgical interventions were performed after short-term preoperative preparation. During the preoperative preparation, patients received medications that correct the condition of the cardiovascular system, respiratory organs, kidneys, metabolic processes, as well as antibacterial agents, antispasmodics, detoxification drugs and others. At the same time, patients were examined and consulted by doctors of related specialties. The patients with signs of purulent cholangitis, in which obstructive jaundice increased or not decreased were operated urgently.Our developed surgical treatment, in addition to the listed tactical and therapeutic measures, included:- earlier performing urgent surgical interventions (in the nearest 1-2 days);- the use of various combinations of minimally invasive surgical interventions and their phased implementation;- overdrainage sanitation of biliary tracts. Most often, the first stage of surgical treatment was the implementation of endoscopic palillosphincterotomy (EPST) with removal of stones from the common bile duct during choledocholithiasis and the installation of nasobiliary drainage (Fig. 1).
 | Figure 1. Scheme of extrahepatic bile ducts sanitation: nasobiliary drainage after EPST |
 | Figure 2. The scheme of extrahepatic bile ducts sanitation with sodium hypochlorite through Vishnevsky drainage |
|
3. Results and Discussion
- In accordance with the described tactical approaches to treating patients, the following types of surgical interventions were performed in the group of people who received traditional surgical treatment and with the developed surgical treatment (Tab.2).
|
|
4. Conclusions
- In the surgical treatment of patients with cholelithiasis complicated by purulent cholangitis, sanitation of the biliary tract with sodium hypochlorite solution helps to prevent the formation of intrahepatic cholangiogenic abscesses and the development of biliary sepsis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML