-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(2): 519-522
doi:10.5923/j.ajmms.20190912.15

New Method to Reduce Complications after Acute Osteomyelitis of Hip Joints in Children
Jamshid Azamatovich Shamsiev1, Zafar Mamadjanovich Mahmudov2
1Head of the Department of the Faculty of Improvement of Doctors in Pediatric Surgery and Anesthesiology, Samarkand City, Uzbekistan
2Assistant of the Department of Pediatric Surgery of the Samarkand State Medical Institute, Samarkand City, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Despite the achievements of modern surgery, traumatology and orthopedics, many issues of the treatment tactics of acute hematogenous osteomyelitis of the bones that form the hip joint (AHO BHJ) remain debatable. The aim of our work was to improve the results of treatment of acute hematogenous osteomyelitis of the hip joint in children by improving the surgical method. For this, we examined 134 patients treated in a 2-clinic of the Samarkand Medical Institute, which were divided into two groups according to the treatment methodology. In group 1, which was divided into two subgroups, traditional methods were used - Gunther's hip arthrotomy and the use of the Ilizarov apparatus for immobilization. In the 2nd group, the original method of draining osteoperforations of the acetabular roof (DOAR) was applied.
Keywords: Acute hematogeous osteomyelitis of the bones of the hip joint, Surgical treatment, Arthrotomy of the hip joint, Ilizarov apparatus, Draining osteoperforation of the acetabular roof
Cite this paper: Jamshid Azamatovich Shamsiev, Zafar Mamadjanovich Mahmudov, New Method to Reduce Complications after Acute Osteomyelitis of Hip Joints in Children, American Journal of Medicine and Medical Sciences, Vol. 9 No. 2, 2019, pp. 519-522. doi: 10.5923/j.ajmms.20190912.15.
Article Outline
1. Actuality
- According to the World Health Organization, "among acute surgical pathology of childhood, acute hematogenous osteomyelitis is 2.2-10%, and among purulent-septic infections - from 12.5% to 47%" [1]. Due to severe purulent-necrotic lesion of bone tissue "in the long term after treatment in about 15-54% of cases, various kinds of orthopedic disorders are observed (ankyloses, false joints, shortening and deformation of the osteoarticular system), leading to disability" [2,3-5,10]. Despite the achievements of modern surgery, traumatology and orthopedics, many issues of the treatment tactics of acute hematogenous osteomyelitis of the bones that form the hip joint (AHO BHJ) remain debatable. To date, most authors are convinced that in the surgical treatment of AHO BHJ, efforts should primarily be aimed at sanitizing the purulent focus and thorough immobilization of the affected limb [6-9]. It remains an important issue to improve the surgical treatment of AHO BHJ in this patient population by introducing new original techniques.
2. Aim of the Research
- Improving the results of treatment of AHO BHJ in children through the use of a new surgical method.
3. Research Materials
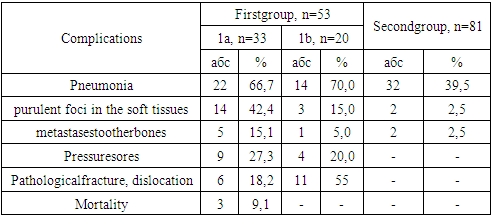
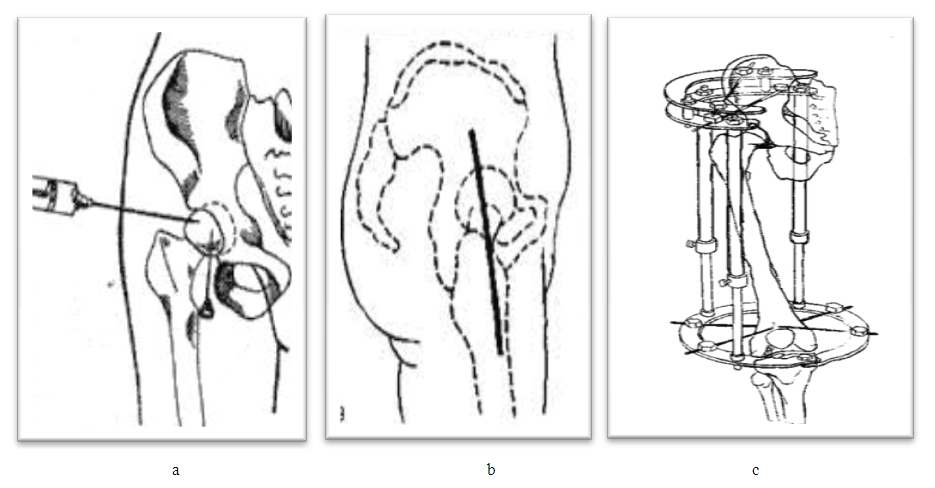
- To achieve this goal, we examined and treated 134 children with AHO BHJ, aged 6 to 16 years, who were hospitalized in the purulent surgery department of the 2 clinic of the Samarkand State Medical Institute from 1991 to 2018. Mostly boys 96 (71.6%) predominated, which is associated with their active lifestyle, the share of girls was 28.4% (38 patients).By the type of surgical procedures performed, the patients were divided into two clinical groups. The first group consisted of 53 (39.6%) children conditionally divided into two groups. 1a, a group of 33 children from 1991 to 2000 who received conventional surgical treatment after a hip joint puncture (Fig. 1a) and if they received a purulent exudate, then went on to produce arthrotomy of the hip joint according to Gunther (front access) (Fig. 1b). Group 1b, to 20 patients from 2000-2003, in the light of the achievement of modern medicine, the next step to prevent orthopedic complications in patients with AHO BHJ, after arthrotomy, the area of the hip joint was fixed using the original technique using the Ilizarov apparatus instead of skeletal traction and immobilization of coxite plaster cast (Fig. 1c).
 | Figure 1. Hip рuncture (а), Gunther access (b) and extrafocal distraction osteosynthesis by Ilizarov apparatus (schemes) |
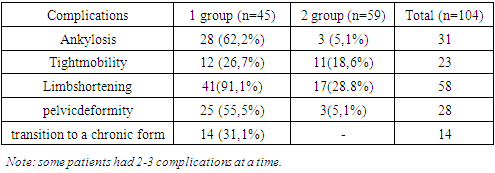
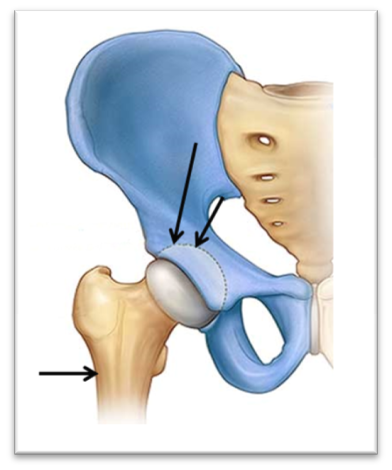 | Figure 2. Draining osteoperforation of the acetabular roof (schemes) |
4. Results
- The analysis of the clinical course showed that the application of the proposed methods of surgical treatment of AHO BHJ allowed to significantly reduce the duration of the period of hyperthermia from 9.36±0.88 to 3.57±0.18 and the length of hospital stay from 43.18±2.96 up to 22.89±0.66 bed days in group 2. Moreover, children from this group were discharged for outpatient treatment without a plaster immobilizing dressing, with completely healed wounds.
|
5. Distant Results
- Of 134 patients with AHO BHJ, long-term treatment results were studied in 104 (77.6%) patients in the period from 1 year to 25 years after discharge from the hospital. Including in 45 (84.9%) patients of the first group (1a group of 26 patients and 1b group of 19 patients), and in 59 (72.8%%) of the second group. The outcomes of treatment of AHO BHJ were traced in terms of 1-2 years in 5.8%, 3-5 years in 9.6%, 6-15 years in 38.5% and 16 years and above in 46.1% of patients.The following parameters served as criteria for evaluating the results of treatment of AHO BHJ: the patient's presence or absence of complaints, examination data, the presence or absence of orthopedic complications (shortening of the lower limb, hip ankylosis, fracture of the femoral neck and pathological dislocation, pelvic deformity), state of limb function. The transition to a chronic form of the disease (the presence of pain, fistula, relapse, etc.) and the clinical and radiological restoration of the bone structure of the affected bones were taken into account.As can be seen from table 2, the comparative analysis showed that the greatest number of complications in the long term after discharge of patients from the hospital was noted in the 1st group, where ankylosis of the hip joint was observed in 62.2% of patients. In the 2nd group, where DOAR was used as a surgical treatment, the percentage of ankylosis was 12 times lower than in the 1st group and amounted to 5%. The same trend was characteristic when comparing other complications: Tight mobility in the hip joint in the 1st group - 26.7%, in the 2nd - 18.6%,; shortening of the affected limb in the 1st group –91.1%, in the 2nd –28.8%, i.e. 3.16 times less likely; pelvic deformity in the 1st group - 55.5%, in the 2nd - 5.1%, i.e. 10 times less often; transition to the chronic form in the 1st group - 31.1%, in the 2nd group - was not detected.
|
6. Conclusions
- The method of draining osteoperforation of the acetabular roof in the treatment of acute hematogenous osteomyelitis of the bones of the hip joint in children, aimed at minimizing the degree of trauma to the massive muscle layer of the surrounding hip joint, ligamentous apparatus and its capsule, providing adequate drainage and sanitation of the lesion, preventing the spread of g as a result, the duration of the patient’s hospital stay decreases from 42 to 23days, mortality from 9.1% to 0%, and validation in remote periods.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML