F. G. Nazirov, A. V. Devyatov, A. Kh. Babadjanov, R. R. Baybekov
Republican Specialized Scientific and Practical Medical Center for Surgery named after acad. V. Vakhidov, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Expanding the spectrum of patients examination with cholelithiasis using modern technologies can improve the quality of diagnosis of subclinical risk factors for surgical treatment associated with the features of the course both the underlying disease and the formation of its complications, as well as a number of other factors that affect the outcome of the surgery. Clinical studies and a detailed analysis made it possible to determine the frequency and degree of significance of various clinical risk factors for the probability of iatrogenic injury in patients with cholelithiasis. Such factors include destructive forms of cholecystitis (35.4% in the structure of all iatrogenia; prognostic significance at confidence limits P = 95% - 1.24 ± 0.43%); infiltrate in the gallbladder neck (28.9%; 4.29 ± 1.87%); Mirizzy syndrome (11.4%; 7.87 ± 5.95%) and “shriveled” gall bladder (5.7%; 3.09 ± 2.18%).
Keywords:
Laparoscopic cholecystectomy, Iatrogenic injury, Bile ducts, Risk factors
Cite this paper: F. G. Nazirov, A. V. Devyatov, A. Kh. Babadjanov, R. R. Baybekov, Iatrogenic Injuries of Bile Ducts: Prognostic Significance of Risk Factors, American Journal of Medicine and Medical Sciences, Vol. 9 No. 2, 2019, pp. 509-514. doi: 10.5923/j.ajmms.20190912.13.
1. Introduction
In modern surgical hepatology, the paces of endovisual technologies development do not tend to decrease, the number of revolutionary developments is progressively increasing, the range of use of minimally invasive interventions is expanding. More recently, the leading in this area laparoscopic cholecystectomy (LCE) has become a routine operation [1-5]. The rapid rehabilitation of patients after minimal surgical trauma and the precision preparation of tissues under optical magnification in the gallbladder region ensured the absolute competition of this type of surgery versus traditional cholecystectomy [6-9]. However, the analysis shows that the objective improvement of indicators is exclusively associated with the rehabilitation aspects, a reduction in the frequency of wound and general complications of the hospitalization period [10-11]. And behind the clear advantage of early rehabilitation is the obvious increase of specific complications connected with the technical features of LCE. The bile ducts (BD) injury is their most complex manifestation [12-14]. The problem of the specifics of the technical implementation of LCE under the conditions of various risk factors for iatrogenia against the background of the complicated course of the main pathology remains acute.Aim of the study was to analyze the prognostic significance of risk factors of iatrogenic injuries of the bile ducts in the aspect of their prevention at laparoscopic cholecystectomy.
2. Materials and Methods
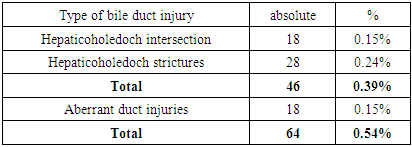
11807 LCEs were performed at the center in 2005-2018. Injuries of the main bile ducts (BD) in the form of complete or partial intersection of hepatico- choledoch (HC) was diagnosed in 18 (0.15%), in the form of strictures of various levels - in 28 (0.24%) patients. Thus, the total number of “fresh injuries” was 46 (0.39%). This is closer to the lower limit of the this indicator statistics range in 0.32 - 0.95%, cited by leading foreign experts [5]. It should be added that in addition to this, there were aberrant BD injuries in 18 of the entire group of operated patients and it raised the total number of duct injuries to 64 (0.54%) (Table 1).Table 1. The frequency of various iatrogenic lesions in the structure of all LCEs
 |
| |
|
In more detail the structure of all iatrogenic injuries of the bile ducts is given in Table 2.Table 2. The structure of bile ducts injuries
 |
| |
|
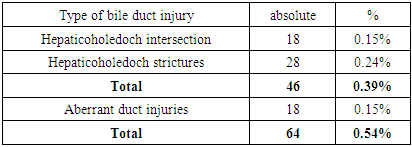
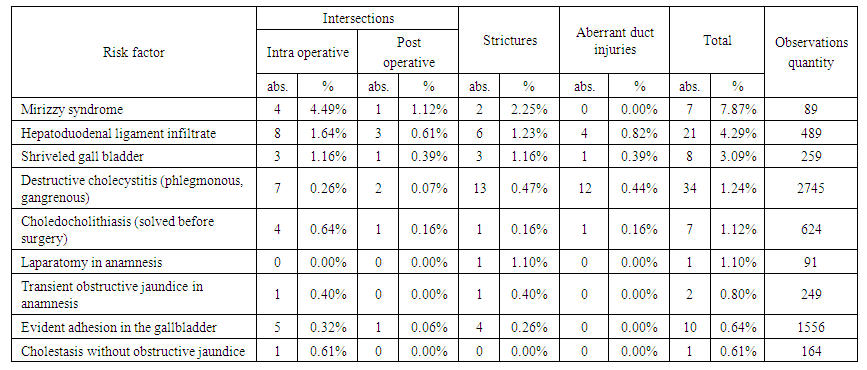
The determination of the total risk of BD injury for all types of iatrogenia depending on various clinical factors showed that the greatest probability of this complication of LCE is in various types of Mirizzy syndrome - 7.87% (in 7 out of 89 patients with this diagnosis; confidence limits at P = 95% - 5.95%). However, this indicator may be subjective in nature, since there is a possibility of covering part of the injury with this complication for other reasons (Tab. 3).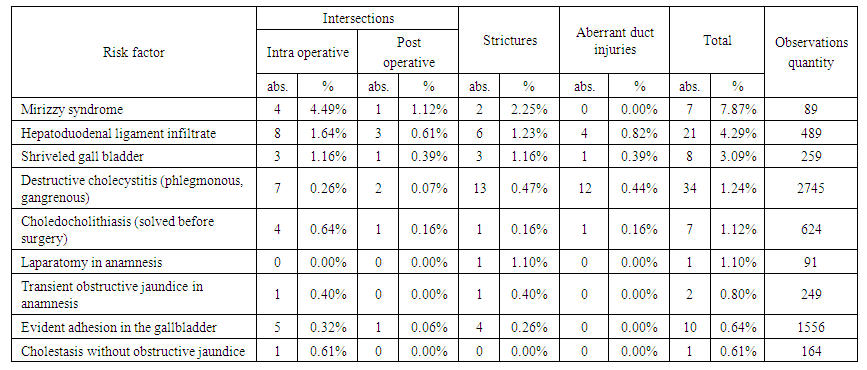 | Table 3. Prognostic value of various risk factors of iatrogenic bile duct injuries |
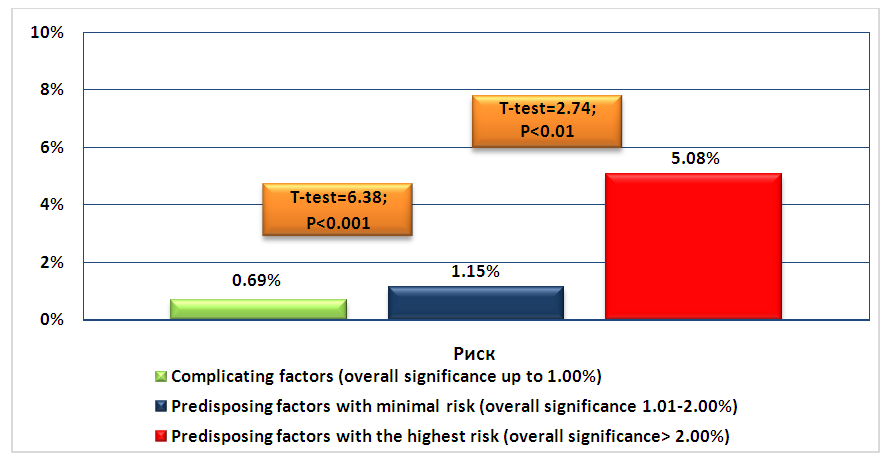
Infiltrate in the hepatoduodenal ligament (HDL) and in the gallbladder neck can lead to BD injuries in 4.29% (± 1.87%) of cases. “Shriveled” gallbladder as a risk factor for iatrogenia was identified in 3.09% (± 2.18%) cases. With the development of destructive cholecystitis, the probability of BD injury was 1.24% (± 0.43%); choledocholithiasis, which was solved endoscopically before surgery - 1.12% (± 0.85%); laparotomy in anamnesis is 1.10% (± 0.47%); evident adhesion in the gallbladder - 0.64% (± 0.41%). Such factors as a transient obstructive jaundice (OJ) in anamnesis (0.80 ±%) and cholestasis without OJ (0.61%) can also cause changes in the normal anatomical ratios of the cystic duct and hepatico- choledoch (HC) against a background of long-term undiagnosed biliary hypertension, which can often be accompanied by cholangitis. Taking into account the prognostic significance, the factors are divided into three groups: complicating factors (up to 1.00%); clinical predisposing factors with minimal risk (1.01-2.00%); clinical predisposing factors with the highest risk (> 2.00%). The average value in the group of complicating risk factors is 0.69 ± 0.06%; in the group of clinical signs with minimal risk - 1.15 ± 0.04% (towards the group of complicating factors: t = 6.38; P <0.001); in the group with the maximum risk - 5.08 ± 1.43% (towards the group with the minimum risk: t = 2.74; P <0.01) (Fig.1).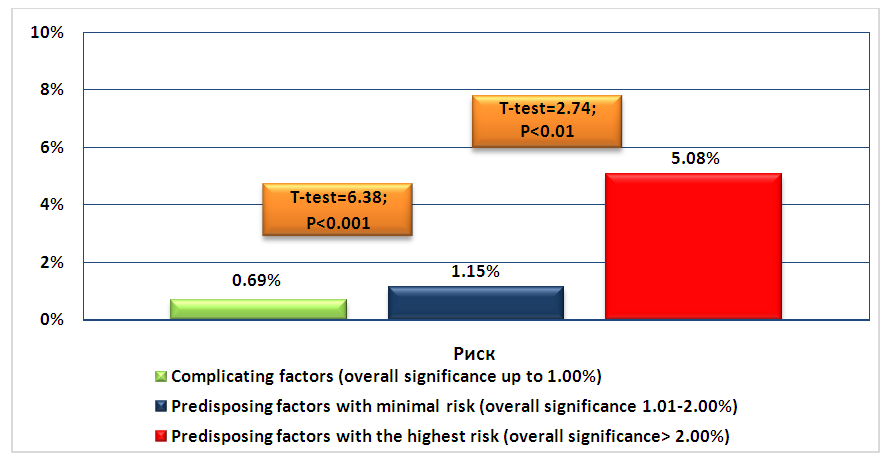 | Figure 1. The distribution and significance of factors by categories |
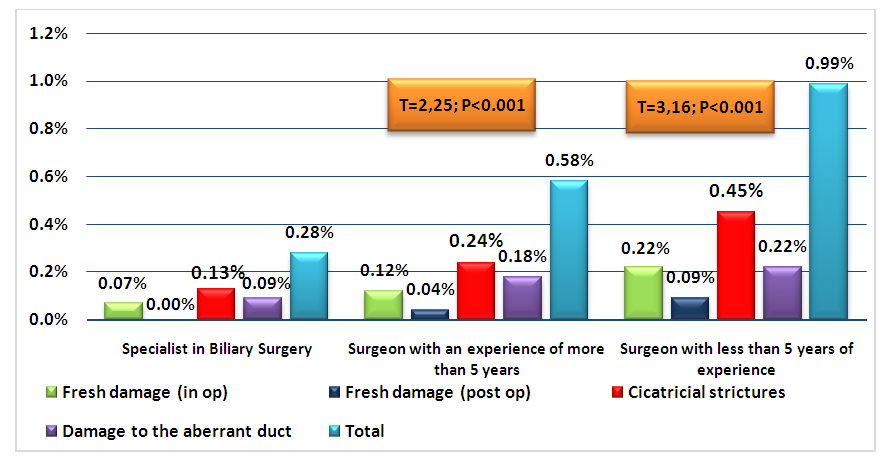
We present an analysis of the of BD injuries frequency depending on the qualifications of the surgeons. We divided them into three categories: specialists in the field of hepatopancreatobiliary surgery performing any operations (4589 LCEs); the surgeons with experience of more than 5 years, performing most types of operations with the exception of complex reconstructive interventions (4987 LCEs); young surgeons with experience of less than 5 years (2231 LCEs). The number of BD intersections in the specialists was 3 (0.07%), all were diagnosed intraoperatively; strictures - 6 (0.13%); injuries of the additional bile ducts - 4 (0.09%). In the surgeons with more than 5 years of experience, the number of BD intersections diagnosed intraoperatively was 6 (0.12%); identified after completion of the surgery - 2 (0.04%); strictures - 12 (0.24%); injuries of the additional bile ducts - 9 (0.18%). In the surgeons with less than 5 years of experience, the number of BD intersections was 5 (0.22%) and 2 (0.09%), respectively; strictures - 10 (0.45%); injuries of the additional bile ducts - 5 (0.22%). In total, 13 injuries were noted among specialists in the field of biliary surgery (0.28%; confidence limits at P = 95% - 0.16%), among young surgeons - 22 (0.99%; confidence limits at P = 95% - 0.42%; t = 3.16; P <0.001 in relation to specialists), and in the surgeons with experience over 5 years - 29 (0.58%; confidence limits at P = 95% - 0.22%; t = 2.25; P <0.05 with respect to specialists) (Fig. 2).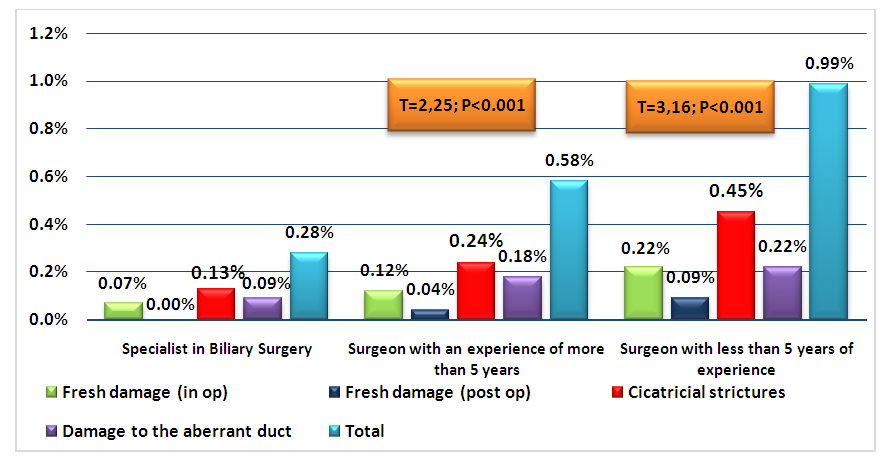 | Figure 2. The dependence of the risk of the bile ducts injuries on the surgeon’s skills |
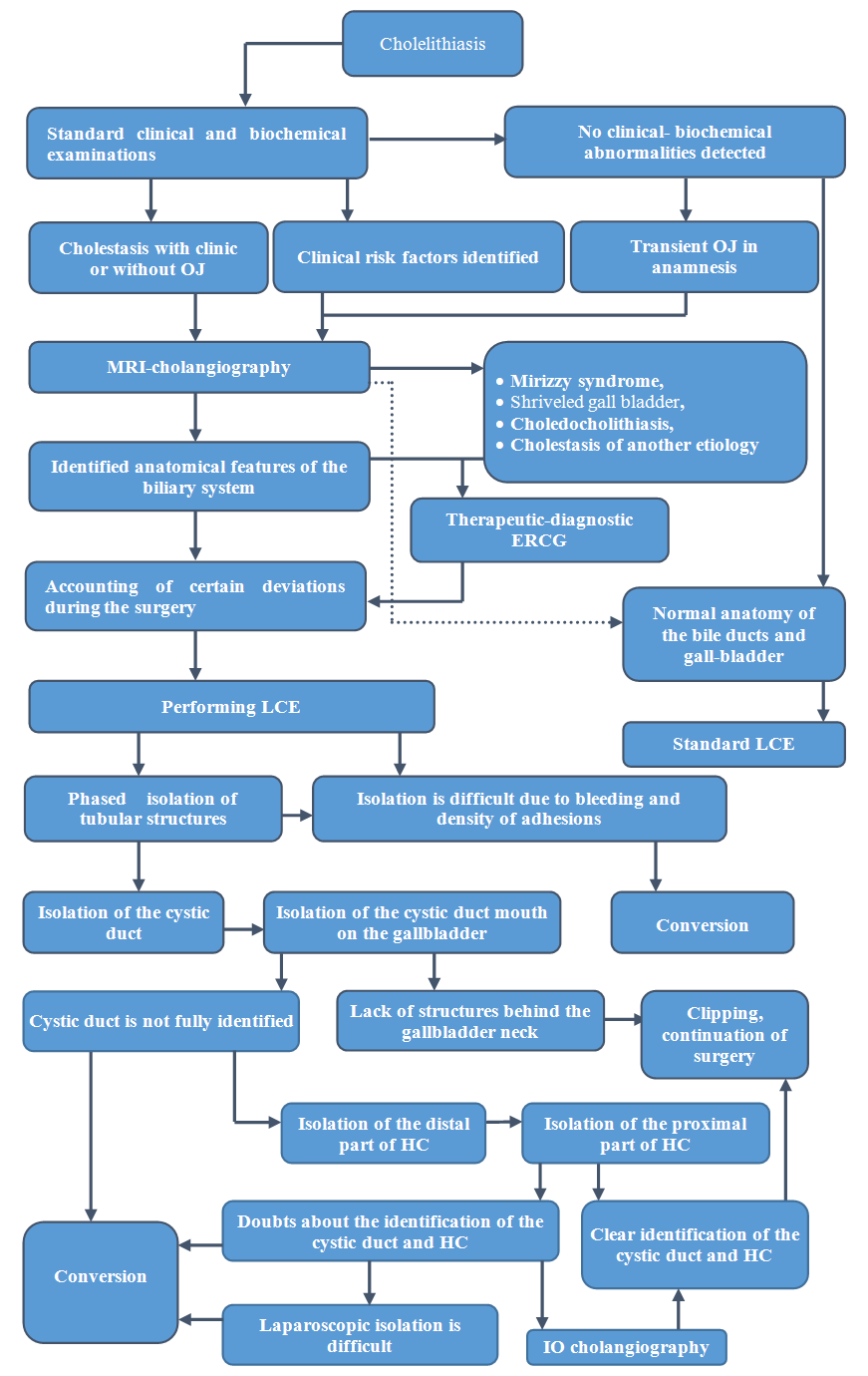
The analysis revealed the main risk factors for BD injuries, taking into account the variant anatomy of the biliary system and the severity of the clinical manifestations of cholelithiasis complications. To reduce their frequency, it is necessary to develop a diagnostic algorithm and tactics for performing LCE based on verification of signs that cause technical difficulties during surgery (Fig. 3).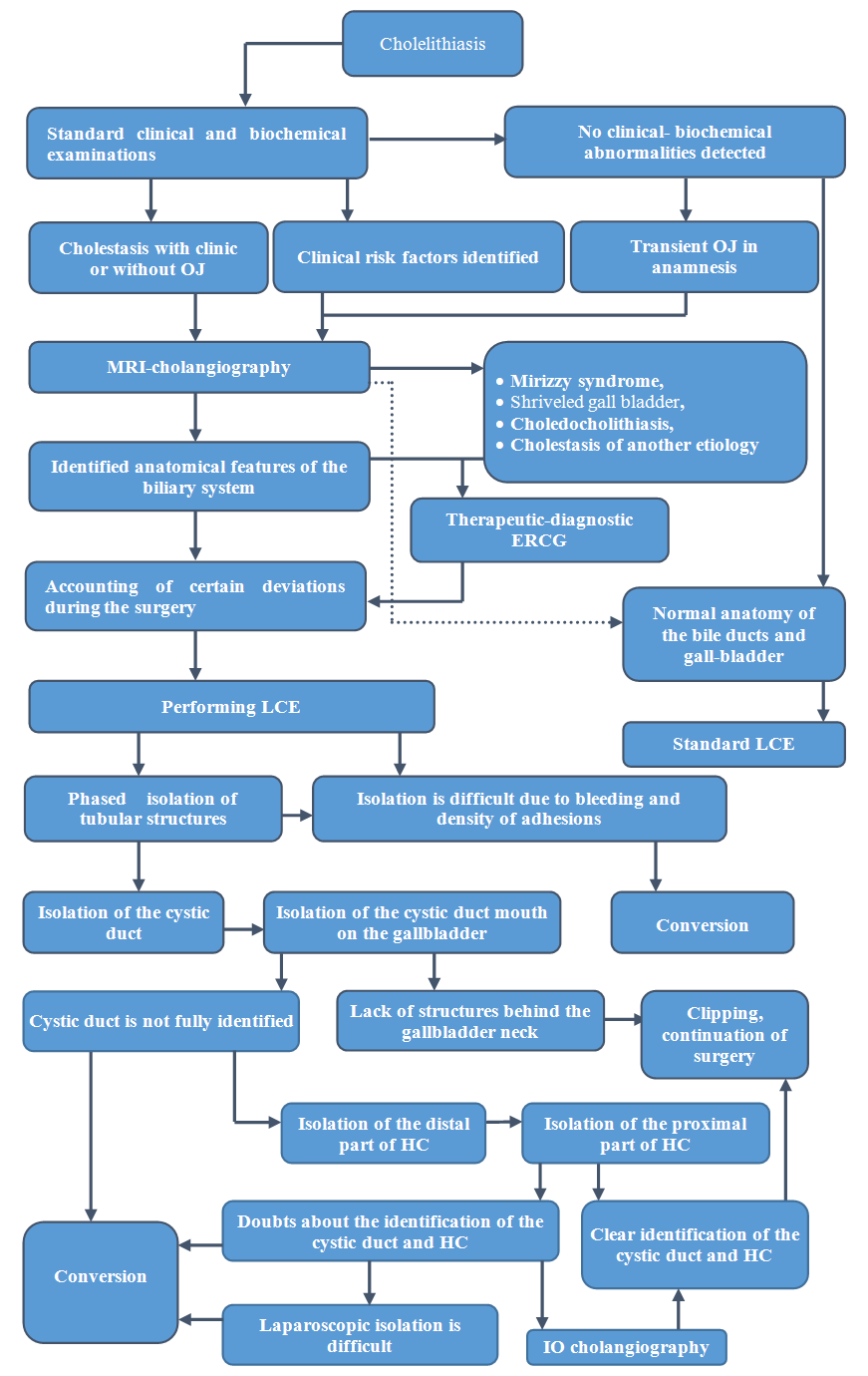 | Figure 3. Algorithm for identifying anatomical and clinical risk factors for iatrogenic injuries of the bile ducts and tactical aspects of LCE |
Patients diagnosed with cholelithiasis should be examined according to the main laboratory and instrumental methods with an emphasis in biochemical analysis on the indicators of bilirubin fractions. An additional examination should be carried out with their increase to identify obstructive jaundice. When verifying cholestasis without clinical manifestations, alkaline phosphatase and gamma-glutamyl transpeptidase indices should be taken into account. An increase of these enzymes is probable against the background of latent choledocholithiasis, stenosing papillitis of the large duodenal papilla (LDP) or other pathology. In these cases, magnetic resonance imaging (MRI) is recommended. If there is a transient obstructive jaundice in anamnesis, an additional MRI-cholangiography should be performed. During verification according to ultrasound investigation data or clinically other predisposing factors, MRI will provide data on the severity of complications and possible deviations in the anatomy of the biliary system. All cases with Mirizzy's syndrome, “shriveled” gallbladder, choledocholithiasis and cholestasis of other etiology should be clarified by endoscopic retrograde cholangiography (ERCG), and if necessary, medical papillotomy (in particular, for lithoextraction or elimination of LDP stenosis). LCE is performed after preparation taking into account data on complications and anatomical features of the biliary system. Any doubts regarding the identification of the main structures of the biliary system should be considered an indication for conversion to open surgery and adequate revision in the intervention area.
3. Discussion
Iatrogenic injuries of the bile ducts are the most serious complication of LCE. Leading importance among the leading causes of injury is given to the various anatomical features of the biliary system structure, in which variant anatomy itself can cause iatrogenia due to the close anatomical relationship between the main structures of the extrahepatic biliary tract. On the other hand, various clinical risk factors associated with a complicated course of cholelithiasis have a significant influence on the change in typical topographic parameters. The development of these predisposing factors causes not only audit difficulties, but also technical difficulties in isolating and identifying elements of the extrahepatic biliary system, which in turn can cause both fresh injury and the formation of cicatricial strictures of the bile ducts in the long-term postoperative period due to thermal or traumatic exposure. It is also appropriate to note another risk factor - the experience of the operating surgeon. Today, endovisual technologies are widely implemented in various parts of the surgical service, and, often, the development of these techniques occurs in the absence of experience of traditional interventions, or surgeons with little experience in laparoscopy perform operations. Of course, in the vast majority of cases, LCE passes without any complications, however, even a minimal percentage of unsatisfactory results against the background of a significant number of such operations in the country contributes to the formation of a large group of patients with various serious complications, which require repeated interventions involving specialists in the field of hepatobiliary surgery. These factors allow us to identify the main directions for reducing the possibility of iatrogenic injury of the bile ducts during LCE.
4. Conclusions
Expanding the spectrum of patients’ examination with cholelithiasis using modern technologies allows not only to improve the quality of subclinical risk factors diagnosis for surgical treatment associated with both the characteristics of the underlying disease and its complications, but also to determine the risks of intervention associated with the high frequency and variety of variant features of the anatomical structure of the hepatobiliary system. Technological progress in this direction can affect the reduction of BD injuries, including with LCE. The conducted analysis made it possible to determine the frequency of various deviations from the typical anatomy of BD, as well as their effect on the probability of iatrogenic injury in combination with various clinical risk factors in patients with cholelithiasis. Factors complicating the course of cholelithiasis include destructive forms of cholecystitis (35.4% in the structure of all iatrogenic; prognostic significance at confidence limits P = 95% - 1.24 ± 0.43%); infiltrate in the neck of the hepatoduodenal ligament (28.9%; 4.29 ± 1.87%); Mirizzy syndrome (11.4%; 7.87 ± 5.95%) and “shriveled” gall bladder (5.7%; 3.09 ± 2.18%).
References
| [1] | Meyer N., Al-Katib S., Sokhandon F. Cholecystohepatic Duct: A Biliary Duct Variant Resulting in Postcholecystectomy Bile Leak. Case Report and Review of Normal and Common Variant Biliary Anatomy // Case Rep Radiol. 2019; 2019: 6812793. Published online 2019 Jun 17. |
| [2] | Pesce A, Palmucci S., La Greca G., Puleo S. Iatrogenic bile duct injury: impact and management challenges // . 2019; 12: 121–128. |
| [3] | Kulikovsky V.F., et al. Bile flow after cholecystectomy. The experience of using minimally invasive treatment methods // Surgery. Journal them. N.I. Pirogov. 2018; (4): 36-40. |
| [4] | Abbasoglu O., Tekant Y., Alper A. et al. Prevention and acute management of biliary injuries during laparoscopic cholecystectomy: Expert consensus statement. Turkish Journal of Surgery. Ulusal cerrahi dergisi. 2016; 32(4): 300-305. |
| [5] | Conrad C, Wakabayashi G, Asbun HJ, Dallemagne B, Demartines N, Diana M, Fuks D, Giménez ME, Goumard C, Kaneko H, Memeo R, Resende A, Scatton O, Schneck AS, Soubrane O, Tanabe M, van den Bos J, Weiss H, Yamamoto M, Marescaux J, Pessaux P. IRCAD recommendation on safe laparoscopic cholecystectomy. // J Hepatobiliary Pancreat Sci. 2017 Nov; 24(11): 603-615. |
| [6] | Lindemann J, Jonas E, Kotze U, Krige JEJ. Evolution of bile duct repair in a low and middle-income country (LMIC): a comparison of diagnosis, referral, management and outcomes in repair of bile duct injury after laparoscopic cholecystectomy from 1991 to 2004 and 2005-2017. // HPB (Oxford). 2019 Aug 16. pii: P 365-182X(19)30623-9. |
| [7] | Kohn JF, Trenk A, Kuchta K, Lapin B, Denham W, Linn JG, Haggerty S, Joehl R, Ujiki MB. Characterization of common bile duct injury after laparoscopic cholecystectomy in a high-volume hospital system. Surg Endosc. 2018 Mar; 32(3): 1184-1191. |
| [8] | Rodrigues G, Pandit SR, Khan A, Veerabharappa B, Jayasankar B, Anaparti R. High insertion of cystic duct at the gallbladder fundus: An undescribed anomaly! // J Minim Access Surg. 2019 Jul-Sep; 15(3): 256-258. |
| [9] | van de Graaf FW, Zaïmi I, Stassen LPS, Lange JF. Safe laparoscopic cholecystectomy: A systematic review of bile duct injury prevention. // Int J Surg. 2018 Dec; 60():164-172. |
| [10] | Spence LH, Schwartz S, Kaji AH, Plurad D, Kim D. Concurrent Biliary Disease Increases the Risk for Conversion and Bile Duct Injury in Laparoscopic Cholecystectomy: A Retrospective Analysis at a County Teaching Hospital. // Am Surg. 2017 Oct 1; 83(10): 1024-1028. |
| [11] | Kara Y, Kalayci MU. Laparoscopic to Open Cholecystectomy: The Risk Factors and the Reasons; A Retrospective Analysis of 1950 Cases of a Single Tertiary Center. // Surg Laparosc Endosc Percutan Tech. 2019 Aug 20. doi: 10.1097/SLE.0000000000000716. |
| [12] | Dili A, Bertrand C. Laparoscopic ultrasonography as an alternative to intraoperative cholangiography during laparoscopic cholecystectomy. Review // World J Gastroenterol. 2017 Aug 7; 23(29): 5438-5450. |
| [13] | de Jong IEM, Matton APM, van Praagh JB, van Haaften WT, Wiersema-Buist J, van Wijk LA, Oosterhuis D, Iswandana R, Suriguga S, Overi D, Lisman T, Carpino G, Gouw ASH, Olinga P, Gaudio E, Porte RJ. Peribiliary Glands Are Key in Regeneration of the Human Biliary Epithelium After Severe Bile Duct Injury. // Hepatology. 2019 Apr; 69(4): 1719-1734. |
| [14] | Cuendis-Velázquez A, Trejo-Ávila M, Bada-Yllán O, Cárdenas-Lailson E, Morales-Chávez C, Fernández-Álvarez L, Romero-Loera S, Rojano-Rodríguez M, Valenzuela-Salazar C, Moreno-Portillo M. A New Era of Bile Duct Repair: Robotic-Assisted Versus Laparoscopic Hepaticojejunostomy. // J Gastrointest Surg. 2019 Mar; 23(3): 451-459. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML