-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(1): 417-420
doi:10.5923/j.ajmms.20190911.02

Transaortic Myectomy without Intervention on the Mitral Valve
Kh. K. Abralov, M. M. Mirsaidov
Republican Specialized Scientific-Practical Medical Center of Surgery Named after Academician V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

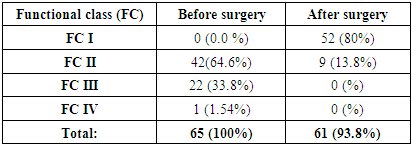
The article gives a retrospective analysis of 65 patients who have been performed a septal myectomy without intervention on the mitral valve for the last 17 years. The operated patients were divided into two groups subject to the degree of mitral insufficiency: the 1st group – 51 patients with mitral regurgitation up to degree I and the 2nd group – 14 patients with mitral regurgitation of degree II and higher. The mean age in the I and II groups was not significantly different and made up 19 ± 17 and 17.5 ± 9 years, respectively (p = 0.655). There were 29 (57%) women and 22 (43%) men in the first group, whereas in the second – 6 (43%) and 8 (57%) respectively (p = 0.631). Mortality was observed in 4 (6.2%) patients, the remaining 61 (93.8%) patients were in functional class I-II of NYHA. Trans-aortic myectomy gives good immediate results: systolic pressure gradient on the output path of the left ventricle and the degree of mitral regurgitation are significantly reduced despite the absence of interventions on the mitral valve.
Keywords: Hypertrophic obstructive cardiomyopathy, Myectomy, Mitral valve
Cite this paper: Kh. K. Abralov, M. M. Mirsaidov, Transaortic Myectomy without Intervention on the Mitral Valve, American Journal of Medicine and Medical Sciences, Vol. 9 No. 1, 2019, pp. 417-420. doi: 10.5923/j.ajmms.20190911.02.
1. Introduction
- Hypertrophic obstructive cardiomyopathy (HOCMP) first described by Teare in 1958 is characterized by genetic disorders in cardiomyocytes and asymmetric left ventricular hypertrophy (LVH), the appearance of the pressure gradient on the level of the left ventricle output tract (LVOT) due to asymmetric hypertrophy of the interventricular septum (IVS) [1,5]. HCMP occurs in 0.2–0.5% of cases in the Europe and the USA (1 case per 500 people). It should be noted that 5% of this number are obstructive and have evident symptoms that are nonresponsive to drug therapy [3]. These patients need surgical treatment which gives long-term improvement in most of them [3]. Hypertrophic obstructive cardiomyopathy (HOCMP) remains the most common cause of sudden cardiac death (SCD) in young people including athletes. HCM accounts for up to 50% of sudden deaths among persons younger than 25 years. The mortality of patients in specialized centers dealing with this pathology is 3-6% per year [2].
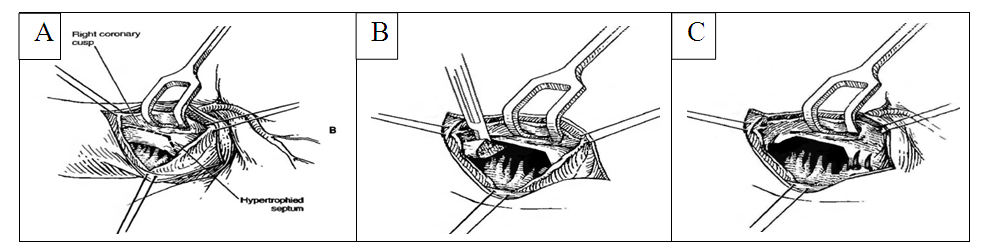
2. Materials and Methods
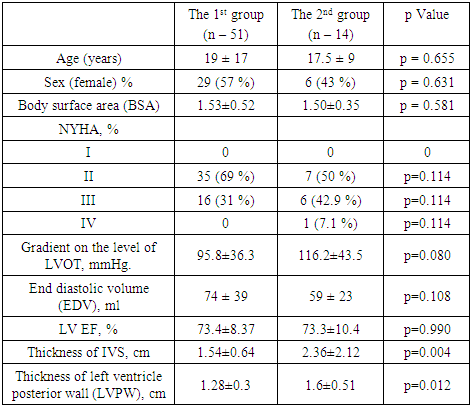
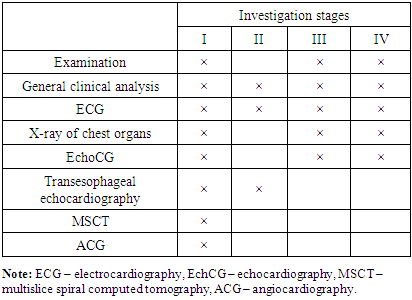
- We retrospectively analyzed 65 patients who underwent septal myectomy without interventions on the mitral valve from 2002 to 2019 at the Republican Specialized Scientific and Practical Medical Center of Surgery named after academician V. Vakhidov. The operated patients were divided into two groups depending on the degree of mitral insufficiency. 51 patients with mitral regurgitation up to degree I were included in the 1st group, the 2nd group – 14 patients with mitral regurgitation of degree II and higher. The mean age in the 1st and 2nd groups was not significantly different and made up 19 ± 17 and 17.5 ± 9 years, respectively (p = 0.655). There were 29 (57%) women and 22 (43%) men in the first group, whereas in the second – 6 (43%) and 8 (57%) respectively (p = 0.631). The rest of anthropometric characteristics are presented in Table 1.
|
|
|
|
3. Results
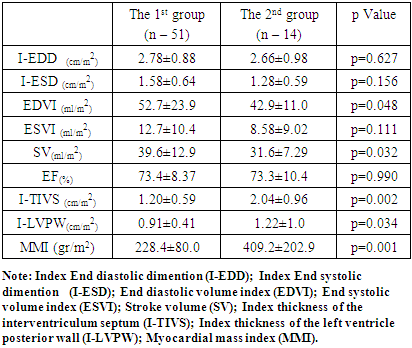
- The average patients stay in the intensive care unit (ICU) varied for the first group of patients from 1 to 8 days (average 1.0 ± 1.0) and in the second group from 1 to 3 days (average 1.5 ± 1.0) and did not differ significantly (p = 0.719). The duration of artificial lungs ventilation (ALV) varied from 160 to 3240 minutes and averaged 590 ± 580 in the first group and from 275 to 3745 minutes (average 532.5 ± 335) in the second group (p = 0.733). Statistical differences were not found when comparing groups for these parameters. Interventricular septum thickness was significantly reduced after surgery in both groups and averaged 2.76 ± 0.99 before surgery and 2.39 ± 0.78 after myectomy (p = 0.026). The systolic pressure gradient at the LVOT was reduced from 95.8 ± 36.3 to 29.6 ± 20.7 (p <0.001) in the first group and from 116.2 ± 43.5 to 42.3 ± 17, 2 (p = 0.002) in the second group respectivel. Iatrogenic defects of IVS after myectomy was not observed in any group. No injuries of the mitral valve or iatrogenic injury of the aortic valve was observed. The duration of cardiopulmonary bypass ranged from 18 to 125 (average 49.5 ± 29 min) in the first group and from 26 to 275 (average 50.5 ± 21min) in the second group (p = 0.826). The duration of cardioplegia varied from 11 to 74 (average 32 ± 23 min) in the first group and from 13 to 177 (average 24.5 ± 25 min) in the second (p = 0.376). 4 (7.8%) patients in the first group and 1 (7.1%) in the second group received permanent pacemakers postoperatively due to a complete AV block. One of these patients in the first group had a complete block of the right leg of the His bundle before the surgery. The appearance of a complete block of the left leg of His bundle is frequent during myectomy. Hemorrhage was noted in one patient from the first group after the surgery and therefore resternotomy and hemostasis were performed. Mediastinitis was developed in one more female patient in the postoperative period. In the dynamics after the treatment the wound was cleansed, secondary sutures were put on the wound. She was discharged in satisfactory condition. Acute heart failure requiring implantation of extracorporeal membrane oxygenation and transferring the patient to intensive care with mechanical support was noted in 1 patient of the 2nd group after the expansion of the aortic root. A fatal outcome was noted in the dynamics of this case. From 14 (28%) patients with mitral valve insufficiency of degree I only 7 (14%) had first-degree mitral insufficiency and in the rest of 7 (14%) patients after myectomy mitral insufficiency regressed postoperatively (p = 0.001). Similarly to the first group, from 14 patients with mitral insufficiency of degree II and III in the second group only 5 (41.6%) had mitral insufficiency II and 5 (41.6%) more cases regressed to mitral insufficiency of degree I (p = 0.461). We analyzed the degree of mitral insufficiency before and after surgery in both groups as a whole and a decrease in the degree of mitral insufficiency in both groups was confirmed with a high degree of confidence (p <0.001). Considering the significant difference in the thickness of the interventricular septum between the groups, we analyzed the correlation of mitral insufficiency degree with the thickness of the interventricular septum and revealed a moderate correlation r = 0.45 with reliability p <0.05.
4. Discussion
- The presence of hemodynamically significant mitral insufficiency (MI) is one of the problems in patients with HOCMP. The development of MI is associated with a number of factors, the main of which is SAM - syndrome (accelerated movement of blood through the narrowed LVOT creates a low pressure zone, resulting in a turbulent flow that picks up the anterior cusp of mitral valve (MV) in the LVOT, which further intensifies the obstruction). An important factor in the development of MI is the anomaly of the chordopapillary apparatus of MV and papillary muscle (PM) hypertrophy. MV deficiency may also be associated with fibrotic changes of the anterior cusp due to prolonged mitral-septal contact at SAM syndrome. Concomitant mitral valve intervention is required in 11–20% of cases in patients undergoing myectomy [12]. In patients with evident lengthening of the anterior mitral valve and / or mitral regurgitation from moderate to severe degree, septal myectomy can be combined with one of several additional procedures, including replacement of the mitral valve, partial excision and mobilization of papillary muscles, plication of the anterior cusp and lengthening with a patch from the pericardium treated with glutaraldehyde, which strengthens the middle part of the anterior cusp of mitral valve [6-7,9-10]. At an elongated anterior cusp of mitral valve preference is given to plastic surgery instead of mitral valve replacement [4]. Surgical mortality in myectomy with intervention on the mitral valve is about 3-4% [8,10-11]. There have been a number of studies in which myectomy is performed without concomitant interventions on the mitral valve with a good result recently.
5. Conclusions
- Trans-aortic myectomy gives good immediate results, and the gradient of systolic pressure in the left ventricular outflow tract and the degree of mitral regurgitation statistically significantly reduced, despite the absence of interventions on the mitral valve.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML