Alimoukhamedova Gulrukh Aibekovna, Khalimova Zamira Yusufovna
Ya. Kh. Turakulov Tertiary Center for the Scientific and Clinical Study of Endocrinology, Uzbekistan Public Health Ministry, Tashkent
Correspondence to: Alimoukhamedova Gulrukh Aibekovna, Ya. Kh. Turakulov Tertiary Center for the Scientific and Clinical Study of Endocrinology, Uzbekistan Public Health Ministry, Tashkent.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The work was initiated to study clinical implications in patients with pheochromocytomas. Materials and methods: Clinical observations among 51 patients (23 men, 45.1%; 28 women, 54.9% and 6 children, 11.8%) with pheochromocytomas undergoing both outpatient and inpatient treatment at the tertiary Center for the Scientific and Clinical Study of Endocrinology, Uzbekistan Public Health Ministry, are at the core of the study. The patients’ age ranged from 13 to 66 years, mean age was 38.7 ± 13.7 years. General clinical, biochemical, hormonal and instrumental methods of investigation constitute the algorithm of the study. Results and discussion: Our study on age-related peculiarities of patients with pheochromocytomas demonstrated presence of pheochromocytomas in all age groups, but predominantly (54.9%; χ2=39.2; р<0.0001) in the young patients (18-44 years). The right localization was found in most patients (62.7%; χ2=5.65; р=0.02), in 13 (25.5%) and 6 (11.8%) the left and bilateral localization was found. Clinical manifestations of pheochromocytoma were highly variable. High arterial pressure observed in all patients (n=51, 100%) was the main symptom of the diversified PHEO clinical picture. Mean age at the first elevation of arterial pressure was 35.4 ± 13.4 years; in 40 patients (78.4%; χ2=30.7; р<0.0001) taking place at the age under 45, that is at the working age, while occurring after 45 in 11 (21.6%). Conclusions: Most pheochromocytomas (54.9%) presented in young people with insignificant predominance of women as compared to men (54.9% versus 45.1%, respectively). Arterial hypertension was registered in 100% of patients being the main clinical symptom of the disease. Arterial hypertension was the mixed one; that is with arterial pressure elevation > 200 mm Hg in the setting of the initially increased arterial pressure. In 15 patients (29.4%) arterial hypertension was constant; sharp rise in arterial pressure in the setting of normal arterial pressure could be seen in 5 (9.8%).
Keywords:
Pheochromocytoma, Adrenals, Arterial hypertension, Adrenalectomy
Cite this paper: Alimoukhamedova Gulrukh Aibekovna, Khalimova Zamira Yusufovna, Clinical-age Characterization of Pheochromocytomas in the Gender Aspect, American Journal of Medicine and Medical Sciences, Vol. 9 No. 0, 2019, pp. 384-388. doi: 10.5923/j.ajmms.20190910.06.
Pheochromocytoma is a hormonally active tumor from the chromaffin tissue producing catecholamines and clinically manifesting with arterial hypertension syndrome of various manifestation rates, as well as with multiple metabolic disorders [1]. The prevalence of PPGLs, that is, of pheochromocytomas (PHEOs) and extra-adrenal paragangliomas (PGLs) is estimated ranging between 1:65000 and 1: 2500, the incidence in the USA varied from 550 to 1600 cases per year [2]. The 4th and 5th decades of life are the most frequent period for the tumors to onset, more frequently in women than in men (55.2% versus 44.8%) [3,4]. A pathological production and secretion of adrenalin, noradrenalin and dopamine resulting in the pronounced lesions of organs and systems is responsible for multiplicity of the tumors’ clinical manifestations.The catecholamine-producing tumors typically present with the diverse and variable manifestations suggestive of many diseases that is why pheochromocytoma is frequently called “great mimic” [2]. Persistently high arterial pressure resistant to a drug therapy and cardiovascular symptoms are a central sign of pheochromocytoma [1]. The incidence of the tumor is estimated ranging from 0.005% to 0.1% in the general population and from 0/1% to 0/2% in the adult population with arterial hypertension. According to some reports, the diagnosis is delayed in up to 70% of cases after many years of life with the uncontrolled or untreated arterial hypertension or posthumously [5]. The uncontrolled (untreated) hormonal activity of pheochromocytoma may have fatal consequences [6]. In a series of patients with PHEOs found posthumously, 75% died of myocardial infarction or the stroke [7]. As the risk of lethal outcome or severe complications is increased, early diagnosis and prompt treatment of the “time bomb” are crucial [8]. Pheochromocytoma and its complications are a cause of disablement and not infrequently deaths of patients of working age [9]; timely diagnosis and adequate treatment are a priority in current clinical medicine. The work was initiated to study peculiarities of clinical manifestations in patients with pheochromocytomas.
1. Materials and Methods
Clinical observations among 51 patients (23 men, 45.1%; 28 women, 54.9% and 6 children, 11.8%) with pheochromocytomas undergoing both outpatient and inpatient treatment at the tertiary Center for the Scientific and Clinical Study of Endocrinology, Uzbekistan Public Health Ministry, are at the core of the study. The patients’ age ranged from 13 to 66 years, mean age was 38.7 ± 13.7 years.General clinical, biochemical, hormonal and instrumental methods of investigation constitute the algorithm of the study. Clinical picture being evaluated, arterial hypertension, its severity, character and duration of the disease were in the focus of the study. The general clinical investigation constituted thorough collection of complaints, medical and life history, assessment of somatic and endocrine statuses, complete clinical examination with arterial pressure measured and body mass index calculated, as well as complete blood count and urine analysis. The biochemical investigation included measurements of the serum potassium, sodium, chlorine, calcium, lipid profile, the fasting glucose and the 2h postprandial glucose, as well as in some cases the oral glucose tolerance test, measurements of the glycated hemoglobin, coagulogram, creatinine, urea and glomerular filtration rate. To study hormonal profile, plasma metanephrines and normetanephrines, plasma aldosterone and aldosterone-to-renin ratio, ACTH and cortisol were measured. The adrenal MSCT with the contrast enhancement in some cases was used as a specific instrumental method. The ECG and ophthalmoscopy were mandatory.To evaluate the peculiarities of clinical manifestations, the mean and standard deviations (M ± SD), as well as the frequency of occurrence was used. Correspondence of numerical data to normal law of distribution was assessed. The differences between mean values of independent and dependent samples were assessed by one-factor ANOVA analysis. χ2 criterion was used to analyze significance of differences between qualitative characters. Significance for all analyses was set up at p<0.05.
2. Results and Discussion
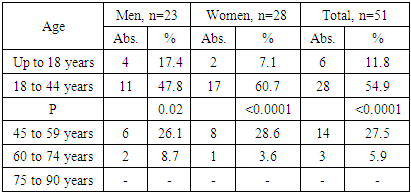
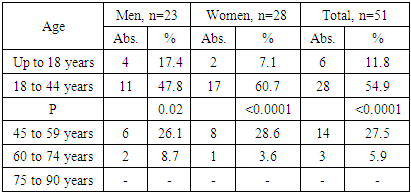
The patients were distributed by age in compliance with the WHO classification (Table 1) to study age peculiarities.Table 1. Characteristics of patients with pheochromocytoma by age and sex (WHO, 2017)
 |
| |
|
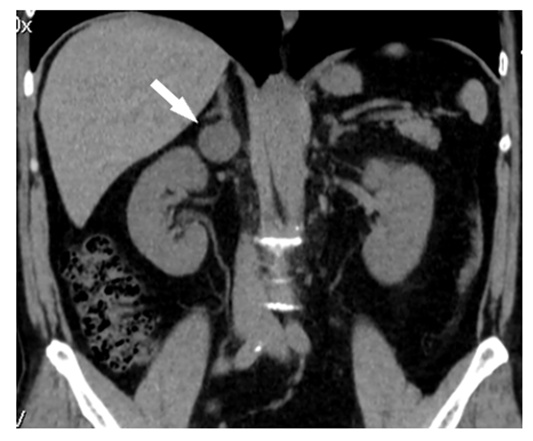
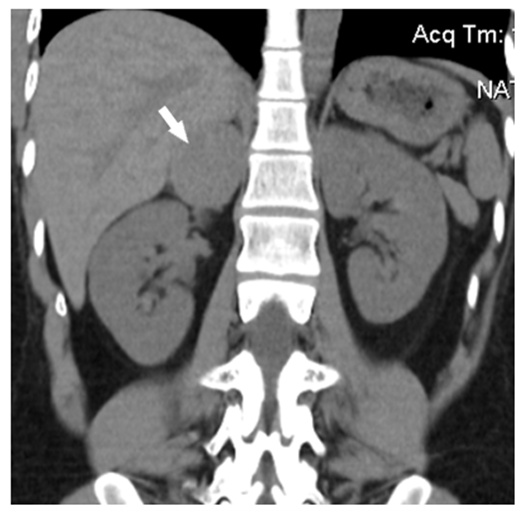
The findings from the analysis demonstrated presence of pheochromocytomas in all age groups, but predominantly (54.9%; χ2=39.2; р<0.0001) in the young patients (18-44 years). As to sex distribution, women were found to predominate (54.9% versus 45.1% of men). Frequency of pheochromocytomas both in men (47.8%; χ2=10.4; р=0.02) and women was significantly high in the age group of 18-44 years (60.7%; χ2=30.9; р<0.0001), after 44 years of age no specific differences between sexes could be seen. There were 6 (11.8%) children, 4 boys and 2 girls among them. The right localization was found in most patients (62.7%; χ2=5.65; р=0.02), in 13 (25.5%) and 6 (11.8%) the left and bilateral localization was respectively found. The familial disease was found in one case (2%). The tumor recurred in 2 (4%) patients, in one male patient in 11 years after primary adrenalectomy, and in one female patient in 2 years after adrenalectomy to the right a tumor in the contralateral adrenal after pregnancy was found (2%). The adrenalectomy for PHEO in medical history was crucial for the right diagnosis in the tumor recurrence. Five patients had a malignant, histologically confirmed pheochromocytoma. Medical history examined, most patients (62.7%; χ2=5.65; р=0.02) did not associate the disease onset with anything, 12 (23.5%) associated it with stress, 3 (5.9%) with pregnancy, 2 (3.8%) with surgeries, 1 (2.0%) with hypothermia and 1 (2.0%) with the childbirth. In 45 (88.2%; χ2=56.6; р=0.0001) the onset of the disease was gradual, while in 6 (11.8%) it was acute, acute cerebrovascular accident and hypertensive crisis occurred in one and in two patients, respectively (n=3,5.9%). Low physical activity (n=17, 33.3%), smoking (n=15, 29.4%), improper feeding (n=15, 29.4%), excessive salt consumption (n=2, 3.9%) were found in the medical histories of the patients. Chronic pyelonephritis (n=20, 39.2%), benign masses (n=13, 25.5%), hypertensive crisis (n=11, 21/6%), ishaemic heart disease (n=9, 17.6%), aortic valve insufficiency (n=9. 17.6%), urolithiasis (n=8, 15.7%), chronic cardiac failure (n=4, 7.8%), obesity (n=4, 7.8%), vascular sclerosis (n=3, 5.9%), stroke (n=2, 3.9%), transient ischemic attack (n=2, 3.9%), chronic myocardial infarction (n=1, 2.0%) and myocardial infarction (n=1, 2.0%) were observed as well. As to familial medical history, cardiovascular disease was found in relatives of 22 men (43.1%) under 55 years of age and of 16 women (31.4%) under 65 years of age; hypertonic disease was found in 30 (58.8%), stroke in 10 (19.6%), IHD in 7 (13.7%), hypertensive crisis in 4 (7.8%), myocardial infarction in 4 (7.8%). Malignancies were registered in 18 cases (35.3%), diabetes mellitus in 8 (15.7%), kidney disease in 3 (5.9%) and pheochromocytoma in 2 (3.9%). Clinical manifestations of pheochromocytoma were highly variable. High arterial pressure observed in all patients (n=51, 100%) was the main symptom of the diversified PHEO clinical picture. Arterial pressure was found to increase up to 213.9±41.5/113.3±17.6 mm Hg in the average. Arterial hypertension duration varied from 6 months to 23 years averaging 3.7 ± 5.1 years. Mean age at the first elevation of arterial pressure was 35.4 ± 13.4 years; in 40 patients (78.4%; χ2=30.7; р<0.0001) taking place at the age under 45, that is at the working age, while occurring after 45 in 11 (21.6%). Because of arterial hypertension, most patients sought for medical help to physicians of various specialties, but none of them were examined for exclusion of secondary arterial hypertension. Primarily, 16 patients (31.4%) were treated by a cardiologist, 8 (15.7%) by a therapist, 5 (9.8%) by a neuropathologist, 2 (3.9%) by a pediatrician, 1 (2.0%) by urologist and 1 (2.0%) by a gynecologist, so that the timely diagnosis was delayed. Only 16 (31.4%) patients saw an endocrinologist primarily, in 2 cases (3.9%) the diagnosis was established by a functional diagnostician. Despite typical clinical manifestations of pheochromocytoma, only 10 patients (19.6%) were diagnosed within the period up to 1 year before first clinical manifestations. The disease was diagnosed within the period from 1 year to 5 years in 28 cases (54.9%) and within the period of more than 5 years in 13 (25.5%) due to late referral to an endocrinologist and treatment by other specialists or prolonged therapy of various antihypertensive agents. In most patients (n=31, 60.8%; χ2=30.4; р<0.0001) arterial hypertension was of a mixed genesis, that is with arterial pressure elevation > 200 mm Hg in the setting of the initially increased arterial pressure. In 15 patients (29.4%) arterial hypertension was constant; sharp rise in arterial pressure in the setting of normal arterial pressure could be seen in 5 (9.8%). Crises, as a rule, either occurred spontaneously or provoked by any factors. 7 patients (13.7%) associated them with physical load, 4 (7.8%) with psychoemotional stress, 2 (3.9%) with food products and 1 (2.0%) with medications. Self-limited crises occurred in 7 cases (13.7%). The frequency of crises varied from once a month to 5-6 times a day. The patients with the repeated vegetative-visceral crises reported on the increased frequency and duration of them over time. In addition to the main complaint, that is, the elevated arterial pressure, most patients had headache (n=96.1%), fatigue (n=45, 88.2%), palpitations (n=38, 74.5%), sweating (n=35, 68.6%), and anxiety and fear (n=31, 60.8%). More than half of the patients complained of fever sensation (n=30, 58.5%), fatigue, anxiety and the shivers (n=29, 56.9%), nervousness (n=29, 56.9%), tremor during the arterial hypertension crises (n=26, 45.1%). Almost half of the patients had vertigo (n=17, 33.3%) and cardialgia (n=23, 45.1%). Weight loss (n=17, 33.3%), sleep disorders (n=12, 23.5%), dry mouth (n=15, 29.4%), lumbar pain (n=12, 23.5%), abdominal pain (n=11, 21.6%), visual impairment (n=10, 19.6%), polyuria )n=10, 19.6%), edema (n=9, 17.6%), pain and numbness in hands and feet (n=8, 15.7%), vomiting (n=8, 15.7%), nocturnal polyuria (n=7, 13.7%) and tinnitus (n=6, 11.8%) were among the complaints. Polydipsia (n=5, 9.8%), muscle weakness (n=4, 7.8%), weight gain (n=3, 5.9%), emotional instability (n=3, 5.9%), urinary incontinence (n=2, 3.9%), dark spots in the vision (n=2, 3.9%) and low sexual vigor (n=2, 3.9%) occurred less frequently. Isolated cases (n=1, 2.0%) of temperature rise, orthostatic hypotension, depression, sleepiness, defective memory, muscle cramps, flush, dysmenorrhea, amenorrhea, physical retardation and neurofibromatosis were reported. As to electrocardiographic changes, the metabolic changes in myocardium and left ventricular hypertrophy were registered in 17 patients (33.3%) and in 16 patients (31.4%), respectively. Dystrophic changes in the myocardium were found in 9 patients (17.6%), low coronary flow in 8 (15.7%) and cardiac conduction defect in 8 (15.7%). One patient had hypertonic angiopathy; one more patient had hypertonic neuroretinopathy. MSCT scans demonstrated round, oval or irregular form of pheochromocytomas with sharp or indistinct regular contours, homogenous or heterogeneous structures with anechogenic areas corresponding to the zones of destruction (Fig. 1 and 2). The sizes of tumors varied from 1.8 to 11.6cm. Analysis of denstitometric characteristics demonstrated that the tumors had high density in the range from 27.9±11.7 to 39.8±14.1 HU. 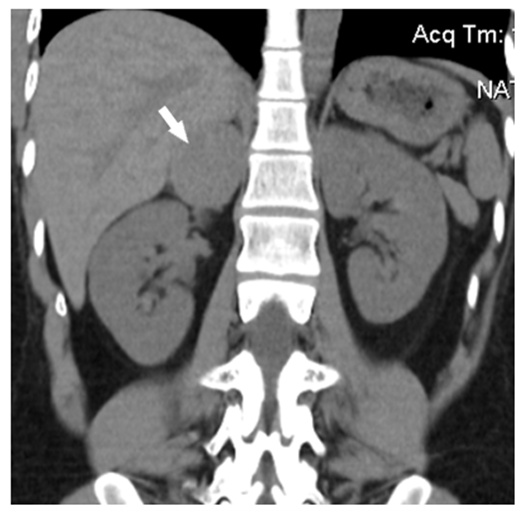 | Figure 1. Pheochromocytoma of right adrenal in a 26-year old woman: a round solid mass with sharp contours (size 4.1 x 3.6 x 4.5 cm, density +43+45 HU) |
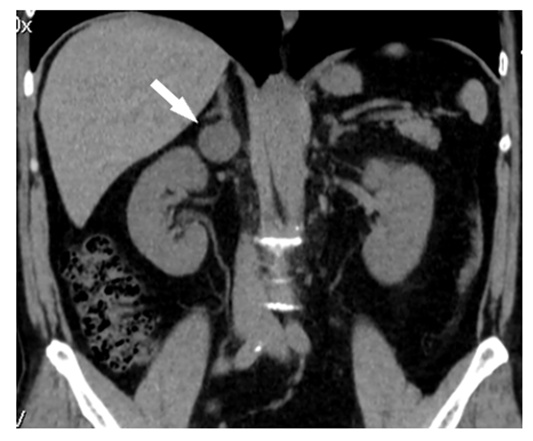 | Figure 2. Pheochromocytoma of right adrenal in a 47-year old man: a round homogenous mass with sharp regular contours can be seen emerging from the medial limb of adrenal gland (density +43+47 HU, diameter 2.6 cm) |
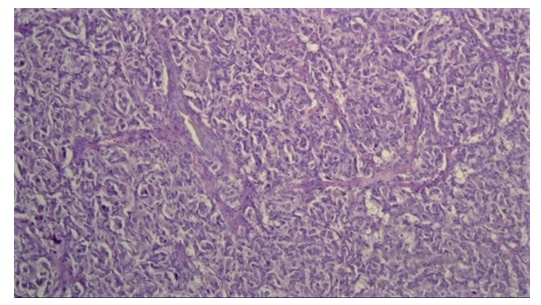
Most patients (82.4%) underwent surgery, 9 (17.6%) refused to be subjected to surgery due to various reasons remaining under observation. 31 patients (68%) underwent conventional laparotomic adrenalectomy, the laparoscopic one was performed in 11 (21.6%). Histological structure of pheochromocytoma can be seen in Fig. 3.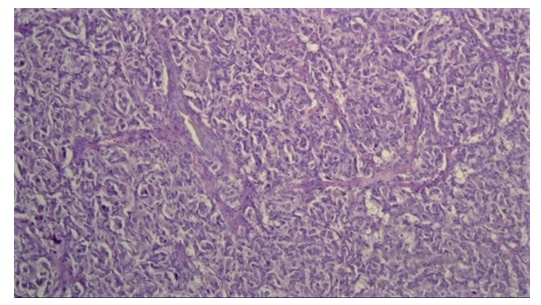 | Figure 3. Hematoxylin and eosin staining of alveolar variant of pheochromocytoma. Multiple alveoli with inner surface consisting of large epithelial, round and polygonal cells with vacuolated cytoplasm can be seen under the thick connective tissue capsule. Nuclei with moderate hyperchromatism and atypism are situated eccentrically. The layers of hyalinized tissue can be seen between alveoli. Foci of gelatinization, as well as an interstitial edema are evident. The cortex is with extensive hemorrhaging foci and decline of lipids in the cytoplasm of adenocytes |
As to bilateral lesions, one-sided adrenalectomy was performed in 3 patients (5.9%), two-sided one by conventional open method was used for another 3 patients (5.9%). Following the surgery, 4 patients (7.8%) developed adrenal insufficiency; thus 3 patients (1 man and 2 women) with bilateral adrenalectomy and one woman with one-sided adrenalectomy are on glucocorticoid replacement therapy at the moment. The removed adrenal tissue grafting was performed in one patient (2%). Prior to diagnosis and surgery, 48 of 51 patients (94.1%) received a drug therapy with various antihypertensive agents, such as alpha-adrenergic blocking agents (n=29, 56.9%), beta-adrenergic blockers (n=28, 54.9%), calcium channel antagonists (n=25, 49%), ACE inhibitors (n=19, 37.3%), diuretics (n=9, 17.6%), and angiotensin receptor blockers (n=4, 7.8%). 9 patients (17.6%) were under monotherapy, the combination of two agents was used for 16 (31.4%), the combination of three agents was used for 21 (41.2%); in 2 cases (3.9%) of malignant hypertension a combination of four antihypertensive agents was used. As to the effect of therapy, no effect was found in 4 patients (11.8%), insufficient effect was seen in 24 patients (47.1%), and effect of antihypertensive therapy was observed in 18 patients (35.3%) additionally receiving alpha-adrenergic blockers.
3. Conclusions
1. Most pheochromocytomas (54.9%) presented in young people with insignificant predominance of women as compared to men (54.9% versus 45.1%, respectively). 2. Arterial hypertension was registered in 100% of patients being the main clinical symptom of the disease. Arterial hypertension was the mixed one in 60.8%, persistent in 29.4% and with sharp rises in blood pressure in 9.8%. Arterial hypertension was found concomitant to vegetative-visceral disorders, such as headaches (96.1%), palpitations (74.5%), sweating (67.6%), fever (58.5%), nervousness (56.9%), tremor during hypertensive crisis (51%) and vertigo (49%).3. Familial medical history is of additional concern, since cardiovascular diseases in relatives of men under 55 years were found in 43.1%, and in relatives of women under 65 years of age in 31.4%; in particular, hypertensive disease (58.8%), stroke (19,6%), IHD (13.7%), hypertensive crisis (7.8%), myocardial infarction (7.8%), in addition to malignancies (35.3%), diabetes mellitus (15.7%), kidney disease (5.9%) and pheochromocytoma (3.9%). Familial disease increases risk of pheochromocytoma in a patient with an adrenal mass. 4. The right localization was found in most patients (62.7%); in 25.5% and 11.8% the left and bilateral localization were respectively found. On MSCT scans pheochromocytomas were rounded, oval or irregular with sharp or indistinct contours, homogenous or heterogeneous structure, sometimes with anechogenic areas corresponding to the zones of destruction. The sizes of tumors varied from 1.8 to 11.6cm. Analysis of denstitometric characteristics demonstrated that the tumors had high density in the range from 27.9±11.7 to 39.8±14.1 HU.
References
| [1] | Dedov II, Bel'tsevich DG, Kuznetsov NS, Mel'nichenko GA. Pheochromocytoma. Moscow: Prakticheskaja medicina; 2005. (In Russian). |
| [2] | Chen H, Sippel RS, O’Dorisio MS, Vinik AI, Lloyd RV, Pacak K; North American Neuroendocrine Tumor Society (NANETS). The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas 39, 775-783, 2010. |
| [3] | Adas M, Koc B, Adas G, Yalcin O, Celik S, Kemik O. Pitfalls in the diagnosis of pheochromocytoma: A case series and review of the literature. J Epidemiol Res 2, 49-55, 2016. |
| [4] | Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, Naruse M, Pacak K, Young WF Jr; Endocrine Society. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99, 1915-1942, 2014. |
| [5] | Iukina MI, Troshina EA, Bel'tsevich DG et al. Pheochromocytoma/paraganglioma: clinical and genetic aspects. Probl Endokrinol (Moscow). 2013; 59(3): 19-26. (In Russian). |
| [6] | Joel T, Goswin Y, Herbert Chen et al. Pheochromocytoma: Current Approaches and Future Directions. Oncologist 2008. |
| [7] | Mittendorf EA, Evans DB, Lee JE, Perrier ND. Pheochromocytoma: advances in genetics, diagnosis, localization, and treatment. Hematol Oncol Clin North Am 21, 509-525, 2007. |
| [8] | Manger WM, Gifford RW. Pheochromocytoma. J Clin Hypertens (Greenwich) 4, 62-72, 2002. |
| [9] | Fernandez-Cruz L.et al. // Pheochromocytoma. - Scand J Surg. - 2004. - Vol. 93, N 4. - P. 302-309. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML