-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(0): 380-383
doi:10.5923/j.ajmms.20190910.05

Diagnostic Criteria for the Character of Generalized Edema in Pediatric Nephrotic Syndrome
B. B. Mamatkulov, A. M. Sharipov, N. K. Zokirov
Department of Emergency Pediatrics, Disaster Medicine, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Correspondence to: B. B. Mamatkulov, Department of Emergency Pediatrics, Disaster Medicine, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The main complaint of patients with nephrotic syndrome (NS) is edema, but the pathogenesis of edema formation is the issue of ongoing controversy. In addition, it is clinically impossible to differentiate patients with severe nephrotic edema with intravascular volume expansion from patients with intravascular contraction. Therefore, despite the possibility of developing quite serious complications, there is a tendency using of albumin with diuretics for the treatment of generalized edema in pediatric practice. The hypoalbuminemia less than 15 g/l and sharply reduced fractional excretion of sodium less than 0.2% are characteristic for most children with nephrotic syndrome for the steroid-sensitive variant of the disease, which correlates with a decrease in renal blood flow and manifestations of the hypovolemic variant of hemodynamics. The expressed hypoalbuminemia (more than 15 g/l) and relatively high fractional excretion of sodium (more than 1.0%) are more characteristic for patients with steroid-resistant NS, which are combined with an increase in renal blood flow and the predominance of hypervolemia. Based on the correlation of hemodynamic parameters and renal sodium retention, we propose the reliable clinical and functional criteria for determining variants of edema syndrome with pathologic mechanisms by type of underfill (refractory edema) and overfill, when sodium retention is primary. This effectively determines the method of treating generalized edema, including infusion therapy with albumin or colloidal solutions on the background of forced diuresis, or use only diuretic therapy.
Keywords: Steroid-resistant and steroid-sensitive nephrotic syndrome, Fractional excretion of sodium, Generalized edema, Edema refractory to diuretics, Hemodynamic disturbances
Cite this paper: B. B. Mamatkulov, A. M. Sharipov, N. K. Zokirov, Diagnostic Criteria for the Character of Generalized Edema in Pediatric Nephrotic Syndrome, American Journal of Medicine and Medical Sciences, Vol. 9 No. 0, 2019, pp. 380-383. doi: 10.5923/j.ajmms.20190910.05.
1. Introduction
- A significant place is occupied by the nephrotic syndrome (NS) in the structure of kidney diseases in children, which is a symptom complex that includes high proteinuria, hypodisproteinemia, hypercholesterolemia, edema. The more expressed excessive fluid accumulation can cause life-threatening complications (pulmonary edema, brain edema). It is necessary to have an idea about the mechanism of development of edema in each specific case for selection more optimal methods treatment and increase the effectiveness of diuretic therapy. Discussions are supported by two theories that characterize the mechanism of sodium retention and the formation of edema in nephrotic syndrome according to the principle of “underfill” or “overfill” [1,2].The theory of “underfill” is based on sodium retention on the background of nephritic hypoalbuminemia, which, according to Starling's principle, leads to a decrease in blood volume and an increase in fluid balance of the extracellular sector, as well as stimulation of neurohumoral pathways leading to sodium and water retention in the kidneys [3]. In turn, a decrease in interstitial colloid osmotic pressure, which accompanied by a decrease in concentration of plasma albumin modulates the loss of intravascular fluid into the interstitial sector in nephrotic syndrome [4].The “overfill” theory states that an increase in plasma volume and sodium retention, leading to the formation of edemas in NS is the result of an internal defect of renal excretion of sodium — increased expression and apical targeting of the epithelial sodium channel (ENaC) in the distal part of the convoluted tubule, the connective tube and collecting ducts of rats’ kidney with puromycin-induced nephrotic syndrome [5,6].Despite the fact that the theory of “underfill” is questioned by the rather important results of clinical and experimental observations confirming the phenomenon of primary sodium retention in NS [7,8], this phenomenon of hypovolemia remains an important component of the pathogenesis of edema, especially in cases of refractoriness to diuretic therapy. Hypovolemia and “underfill” are more expressed in nephrotic subjects with very low levels of serum albumin, especially in children with minimal change kidney disease [9].Currently, it is widely believed that sodium retention develops in all subtypes of NS due to the activation of sodium retention in collecting channels (ENaC) regardless of volemic disturbances [10,11]. Other mechanisms, including supposed an increase in the permeability of blood capillaries [12,13], a decrease in the renal response to atrial natriuretic peptide (ANP), a decrease in the conversion of pro-ANP to ANP in the kidney, and a decrease in the expression of nitric oxide in the kidney [14] likely promote the retention of sodium and the formation of edema in NS. And “underfill” is an additional mechanism for the formation of edema in some nephrotic patients [15].Thus, the determination of the mechanism of edema formation remains difficult, and the time for conducting the required laboratory tests is insufficient, which may affect to accept the efficient corrective actions in the development of generalized edema.
2. Material and Methods
- The results of analysis of 120 children with nephrotic syndrome aged 2 to 15 years, with a disease duration of 2 weeks to 10 years were used in the current study. There were 52 girls and 68 boys among the examined patients. 74 children had a steroid-sensitive variant nephrotic syndrome (SSNS), 46 children had a steroid-resistant variant nephrotic syndrome (SRNS). The separation of patients into steroid-resistant and steroid-sensitive variants of NS was carried out in accordance with the response to the standard course of steroid therapy (prednisolone 60 mg/m2 /day). A steroid-resistant variant of NS was stated in inefficiency of therapy for 8 weeks or within 4 weeks and subsequently three-times intravenous administration of methylprednisolone in a dose of 20 mg/kg (but not more than 1 g per administration). Before beginning of study, verbal assent was obtained from parents of children.A standard study of clinical and functional parameters was conducted in all children with NS. Additional studies in all children included: the determination of fractional excretion of sodium (FENa), Echocardiographic examination to study the following indicators: Strike Index (SI), Cardiac Index (CI), Diastolic Index (DI), and Doppler study of the inferior vena cava and renal vein.The received results were subjected to the statistic processing with the using of standard software package Excel on method of variation statistics with an estimation of the statistical significance of indicators (M±m). P<0.05 was considered significant.
3. Results and Discussion
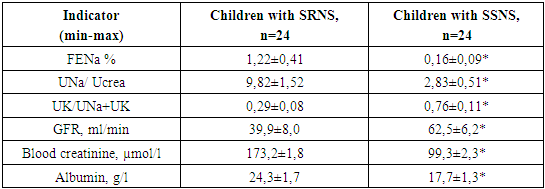
- The obtained results of study of the character of generalized edema in two main groups showed that in the group of children with SSNS, mostly observed critical conditions associating with expressed generalized edema, including anasarca in 74% of cases, hypovolemic shock (18%) and pure nephrotic crisis with a picture of acute abdomen (8%). In the group of children with SRNS, there was a different picture of the frequency of critical conditions. Anasarca was diagnosed in almost half of cases, and hypovolemic shock developed much less frequently (16% of cases). However, in every third case, the SRNS was complicated by acute renal injury (ARI) and hypertensive crisis (32% of cases).When analyzing the indicators of renal retention in children with nephrotic syndrome for SSNS variant of disease, there were abruptly reduced fractional excretion of sodium (0.16 ± 0.09%), low sodium to urinary creatinine ratio (2.83 ± 0.51) and high content of potassium in the urine relative to the range of potassium and sodium (UK/UNa + UK = 0.76 ± 0.11). These changes proceeded on the background of critical hypoalbuminemia and insignificant decrease in the filtration capacity of the kidneys. For children with SRNS as a whole were characteristic relatively higher fractional excretion of sodium more than 1.2%, a high sodium/creatinine ratio of 9.82 and a low Ucrea /UNa + Ucrea=0.29 ratio compared to the group of children with SSNS. At the same time, there was a disturbances of the filtration ability of the kidneys with hypoalbuminemia (table 1).
|
|
|
4. Conclusions
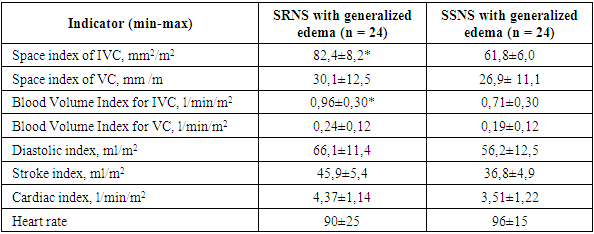
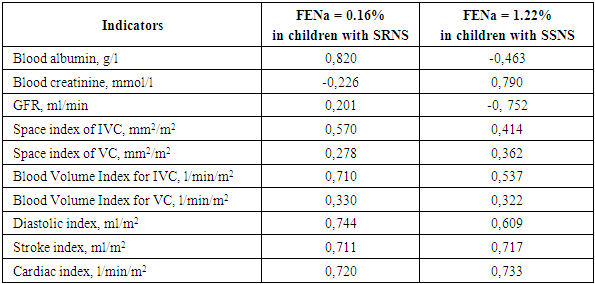
- The results of our study, in cases of generalized edema in children with SSNS and SRNS, allowed us to establish clinical and functional criteria for the character of causes of development of edema. Wherein, a group of patients (in 11 cases - 45%) with refractory edema were mainly children with SSNS. Critical hypoalbuminemia (less than 15g /l in plasma) and sodium renal retention (FENa <0.2%) was determined in this group, which reliably correlated with intravascular fluid volume reduction (hypovolemia: a decrease in average indices of the area IVC index, volumetric blood flow in the inferior vena cava and renal veins on the background of a decrease in the diastolic index of the left ventricle, stroke and heart indices). The structure and frequency of development of critical states was determined in children with nephrotic syndrome, depending on the course of the disease by the steroid-sensitive and steroid-resistant variants. The first variant characterized by generalized edema with anasarca (in 74% of cases), hypovolemic shock (in 38%) or nephrotic crisis (19%), and for the second - severe edema proceeded with anasarca (49%), acute kidney injury, hypertensive crisis (in every third case) and more frequent infectious complication (sepsis and pneumonia).Consequently, based on the correlation of hemodynamic parameters and renal sodium retention, we propose the reliable clinical and functional criteria for determining variants of edema syndrome with pathologic mechanisms by type of underfill (refractory edema) and overfill, when sodium retention is primary. This effectively determines the method of treating the generalized edema, including infusion therapy with albumin or colloidal solutions on the background of forced diuresis, or use only diuretic therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML