-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(0): 372-379
doi:10.5923/j.ajmms.20190910.04

The Value of Neutrophil to Lymphocyte Ratio in the Prediction of Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Zeinab Helmy El Sayed1, Zeinab Adawy2, Samia Taher Ali1
1Department of Internal Medicine, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
2Chest Diseases Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
Correspondence to: Zeinab Helmy El Sayed, Department of Internal Medicine, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

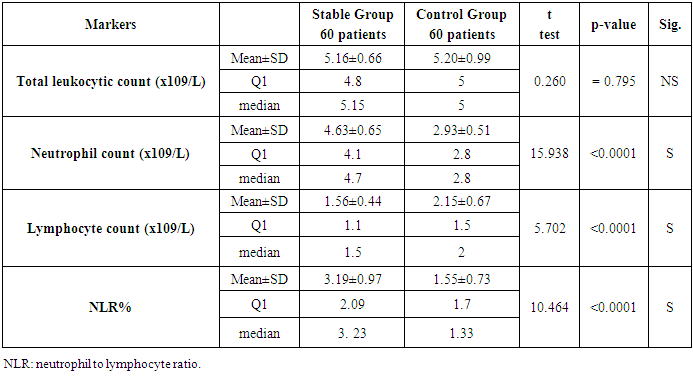
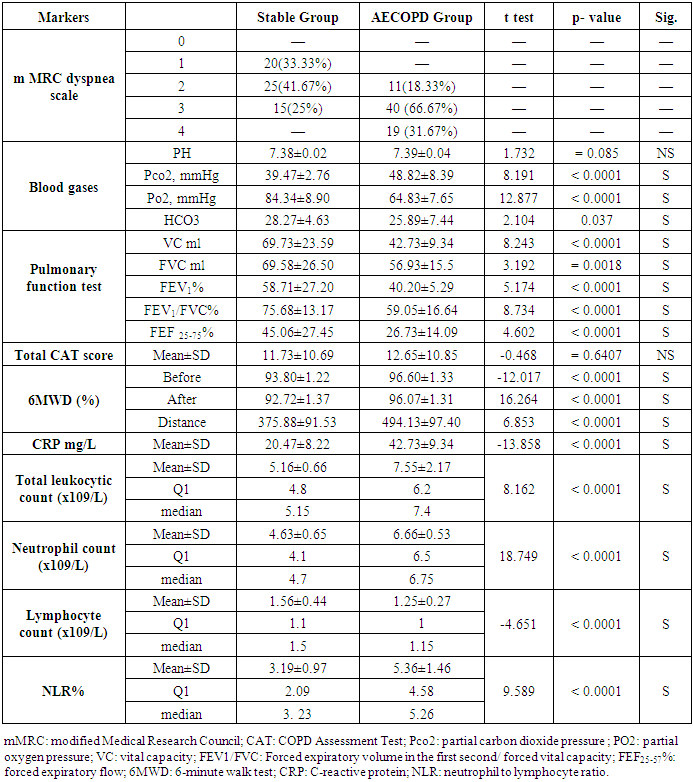
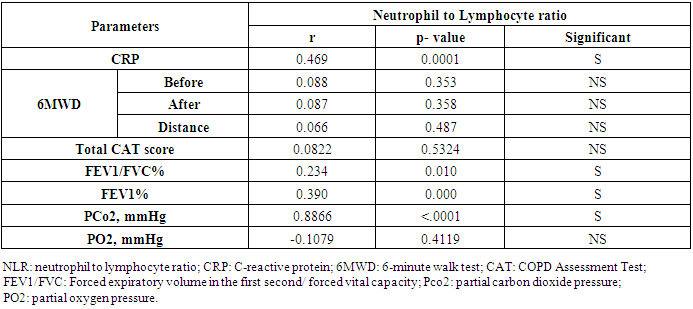
Background: Chronic obstructive pulmonary disease (COPD) is associated with the pulmonary and systemic inflammatory response. Neutrophil to lymphocyte ratio (NLR) was considered as a prognostic inflammatory marker in many inflammatory diseases. We aimed to assess the value of Neutrophil to Lymphocyte ratio in the prediction of Chronic Obstructive Pulmonary Disease. Method: One hundred and twenty COPD patients (do not receive systemic corticosteroid in the last three months before conducting the study) divided into two groups: 60 stable COPD patients as a group I and 60 acute exacerbated COPD patients as a group II were included in this study. Other 60 apparently healthy subjects served as a control group.). We evaluate NLR according to neutrophil count and lymphocyte count in complete blood count, C Reactive protein (CRP), Spirometry was done at least three times for all patients. Results: We found that the neutrophil count and NLR were significantly elevated in stable COPD (4.63±0.65, 3.19±0.97), respectively, than Healthy control (2.93±0.51, 1.55±0.73), respectively, and also, in AECOPD group (6.66±0.53, 5.36±1.46) than stable COPD group. However, there was no significant difference of total leukocytic count between the all studies groups. NLR was inversely correlated with forced expiratory volume in the 1 second (FEV1) (r= -0.390, p= 0.000) and FEV1/FVC (r= 0.234, p= 0.010). There was a significant positive correlation between NLR and CRP (r=0.469, p=0.0001). But there was no correlation with NLR and total CAT score (r= 0.0822, p= 0.5324). Conclusion: Our finding suggested that the neutrophil to lymphocyte ratio can be used as a good marker for prediction and detection of the acute exacerbation of COPD also for assessment and follow up the treatment.
Keywords: Acute exacerbation, Chronic Obstructive Pulmonary Disease, Neutrophil to Lymphocyte ratio
Cite this paper: Zeinab Helmy El Sayed, Zeinab Adawy, Samia Taher Ali, The Value of Neutrophil to Lymphocyte Ratio in the Prediction of Acute Exacerbation of Chronic Obstructive Pulmonary Disease, American Journal of Medicine and Medical Sciences, Vol. 9 No. 0, 2019, pp. 372-379. doi: 10.5923/j.ajmms.20190910.04.
Article Outline
1. Introduction
- Acute exacerbation is one of the characteristic features of chronic obstructive pulmonary disease (COPD). It is characterized by a progressive decline in pulmonary function [1]. The pathological hallmark of COPD is a chronic inflammation of the lung and airways, this inflammation is increased during an acute exacerbation [2]. The acute exacerbated COPD is usually associated with a high rate of morbidity and mortality [3].The accepted traditional method to evaluate the COPD progression and severity is pulmonary function test particularly forced expiratory volume in the first second (FEV1). However, the FEV1 measurement is poorly correlated with the presence of specific symptoms and not actually reflects the severity of COPD or its acute exacerbation [4]. Therefore we need another cheap and easily measurable biomarker to evaluate and predict the acute exacerbation of COPD.Indeed, besides the presence of chronic pulmonary inflammation in COPD, it is accompanied by persistence low-grade systemic inflammation at a stable stage of COPD and increased during exacerbation [5]. The systemic low-grade inflammation can be evaluated by measuring the C-reactive protein, serum fibrinogen, and leukocyte count [6]. There are many hematological markers considered as a reliable index of systemic inflammation. One of these markers is circulating neutrophil levels and the ratio between neutrophil to lymphocyte can predict the severity of some chronic inflammatory diseases as [7-9].Therefore, we aimed to assess the value of Neutrophil to Lymphocyte ratio in the prediction of acute exacerbated Chronic Obstructive Pulmonary Disease in comparison to stable COPD and healthy control.
2. Material and Methods
- Our study was carried out in Al- Zahraa University hospital, during the period between March 2018 and December 2018. The current study included a total of 120 COPD patients were admitted to Chest disease and Internal Medicine departments. We excluded the COPD patients who had pneumonia, bronchiectasis, tuberculosis, malignancy or any other inflammatory diseases. All patients had been receiving optimum medical treatment in the form of inhaled long-acting B2 stimulant, anticholinergic drugs, and an inhaled corticosteroid. Also, all patients do not receive systemic corticosteroid in the last three months before conducting in our study. Informed consent was taken from all subjects in this study. Our study was done according to the ethical committee of the Faculty of Medicine, Al Azhar University, and was conducted in accordance with the Declaration of Helsinki. All patients underwent full medical history taking and full clinical examination.The diagnosis of COPD patients were based on modified criteria by GOLD 2017 guideline [10]. All COPD patients had post-bronchodilator forced expiratory volume in the first second (FEV1) less than 80% of the predicted value, and FEV1/FVC (Forced vital capacity) not more than 70%. They had an increased FEV1 less than 200 ml or less than 12% of the baseline value, 15-20 minutes after puffs of inhaled salbutamol that was given via a metered-dose inhaler to differentiate between bronchial asthma and COPD.The COPD patients were classified according to the definition of acute exacerbation which, defined as a development of acute worsening of patients respiratory symptoms into stable COPD group and AECOPD group [4].All participants were classified into three groups:Group I: 60 Stable COPD patients, their age ranged between 40 – 63 years.Group II: 60 acute exacerbated COPD patients, their age ranged between 35 – 67 years.Group III: 60 Healthy individuals as control group, their age ranged between 42 – 65 years.The all COPD patients and control group were subjected to the following: (all routine clinical tests were performed in the clinical pathology department and pulmonary function tests were done Respiratory department at Al Zahra hospital): Complete blood count, C Reactive protein, Erythrocyte sedimentation rate, Fasting and postprandial blood glucose level, Arterial blood gases, Plain X-ray chest, ECG, Transthoracic echocardiography, Pulmonary function tests (Vital capacity (VC), Forced expiratory volume in 1 s (FEV1%), Forced vital capacity). We calculated the neutrophil to lymphocyte ratio by dividing the absolute count of a neutrophil by the absolute count of lymphocyte. The resting arterial blood gases were done by using blood gases analyzer Rapid Lab 248. The following parameters were recorded pH, arterial O2 tension (PaO2), arterial CO2 tension (PaCO2), and HCO3.Complete blood count (CBC), C- Reactive protein (CRP) and Erythrocyte sedimentation rate (ESR) were measured from peripheral venous blood samples at clinical pathology department in Al- Zhraa University hospital. The Neutrophil to Lymphocyte ratio was calculated according to the neutrophil and lymphocyte counts from CBC.The lung function tests were carried out using Spirosift Spirometry 5000 FUKUD a NENSHI. Spirometric- indices were calculated using best of three technically satisfactory trials in accordance with the recommendation of American Thoracic Society [11]. The following parameters were recorded (FVC%, FEV1%, FEV1/FVC%, Peak expiratory flow rate, forced expiratory flow (FEF) 25-75%).The severity of the symptom was determined by the Modified Medical Research Council breathlessness score (mMRC). We used the COPD assessment test (CAT) score to assess patient life.
3. Statistical Analysis
- SPAA for Windows used in the interpretation of data. Quantitative data were presented as the mean and standard. The 95% confidence interval was calculated when suitable. ANOA was used to test the significance of the changes in the measured variables across time point. Qualitative data were presented as number and percent. A p-value of 0.05 or less was considered statistically significant.
4. Results
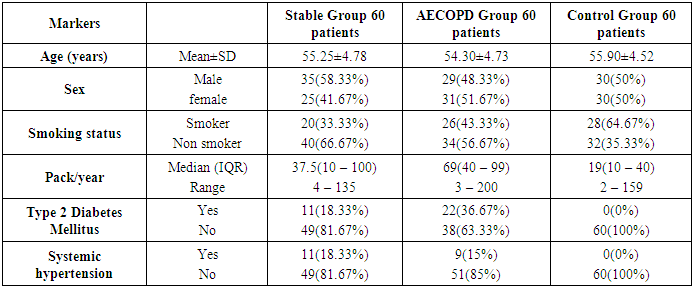
- Table 1 shows the demographic data of the study groups. A total of 120 COPD patients were included in the current study and other 60 healthy individuals served as a control group. Approximately, thirty-three percent of stable COPD patients were smokers and twenty-six percent were smokers in AECOPD, but there were twenty-eight percent smokers in the control group. There were eleven patients had type 2 diabetes mellitus and eleven had systemic hypertension in stable COPD group but there were 22 patients had type 2 diabetes mellitus and nine patients had systemic hypertension in AECOPD group.
|
|
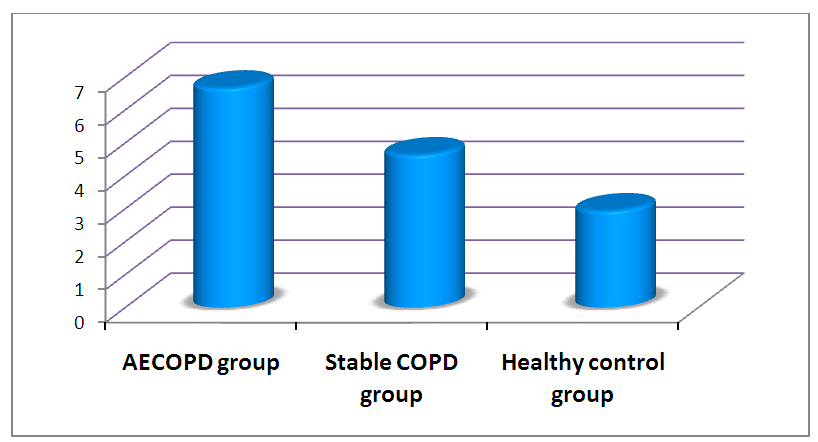 | Figure 1. Comparison the Mean of Neutrophil count in AECOPD group, Stable COPD group, and Healthy control group |
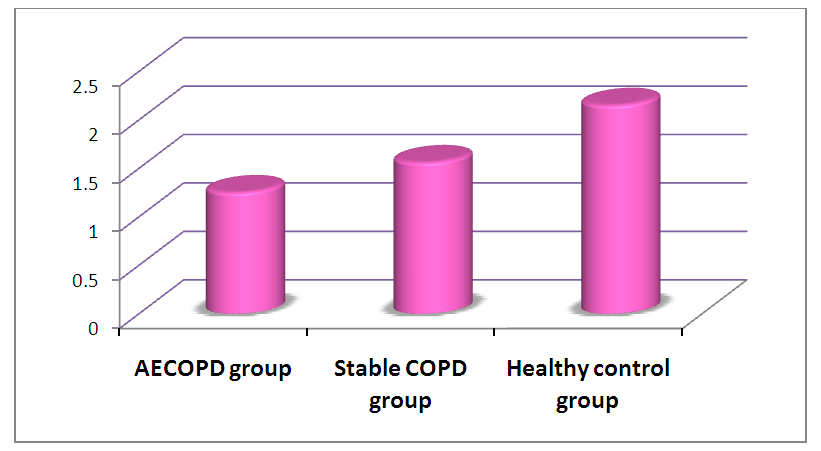 | Figure 2. Comparison the Mean of Lymphocyte count in AECOPD group, Stable COPD group, and Healthy control group |
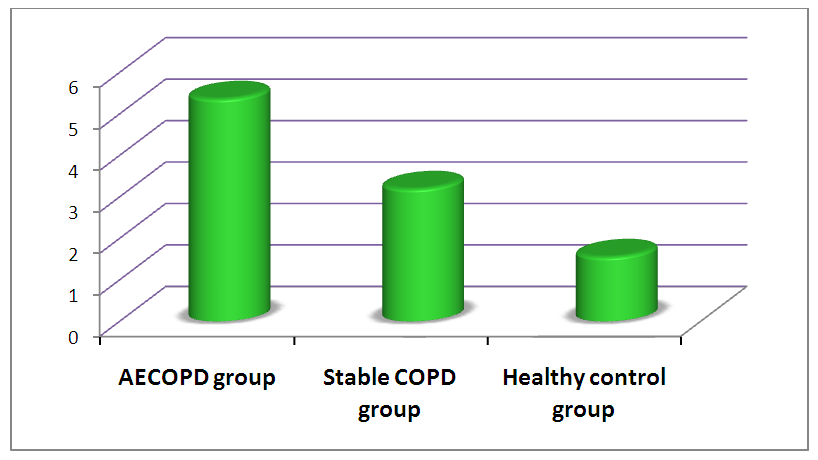 | Figure 3. Comparison the Mean of Neutrophil to Lymphocyte Ratio in AECOPD group, Stable COPD group, and Healthy control group |
|
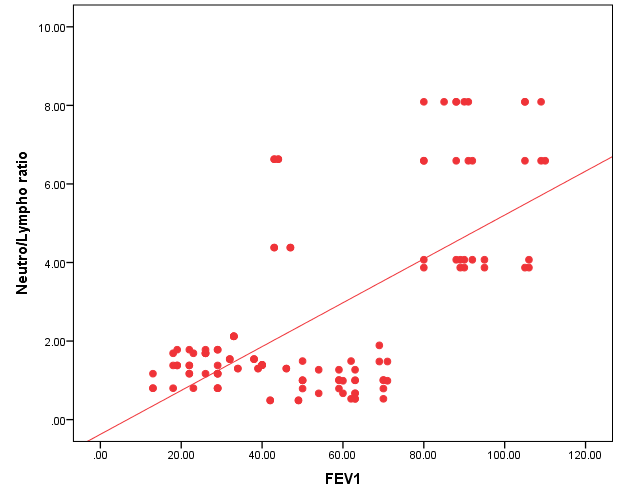 | Figure 4. The correlation between Neutrophil to Lymphocyte ratio and Forced expiratory volume in the first second (FEV1%) |
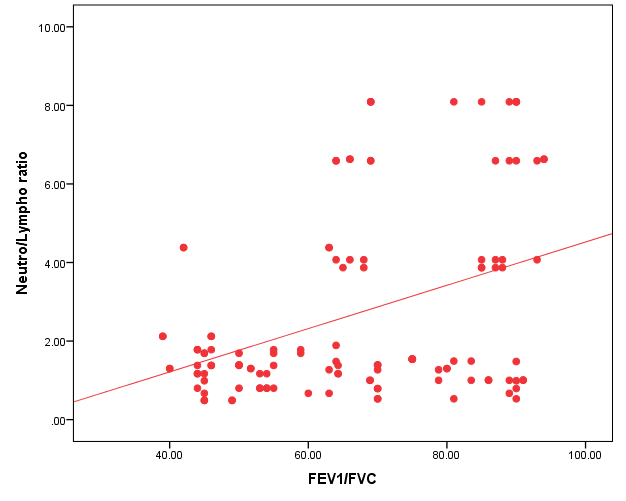 | Figure 5. The correlation between Neutrophil to Lymphocyte ratio and Forced expiratory volume in the first second/ forced vital capacity (FEV1/FVC%) |
5. Discussion
- The acute exacerbation of COPD is the most important event in the clinical course of the disease that requires hospitalization and usually associated with an increased mortality rate. In previous studies, it has been established that the decline of lung functions in COPD has been linked to low-grade systemic inflammation besides the pulmonary inflammation. Additionally, there are many biomarkers can predict the presence of low-grade systemic inflammation as leucocytic count, acute phase proteins, and many other inflammatory markers [6]. Indeed, the reducing frequency of AECOPD is the goal of management of COPD. So we need an easily measurable, cheap and non-invasive chemical biomarker to detect the acute exacerbation as early and for follow up the course of the COPD.In our study, we demonstrated a significant elevation in the mean (SD) of neutrophil to lymphocyte ratio in acute exacerbated COPD patient group when compared to stable COPD patient group. Taylan and his colleague 2017 [12] reported that the neutrophil to lymphocyte ratio was elevated in AECOPD. Aksoy and his colleague study 2018 [13] demonstrated that the neutrophil to lymphocyte ratio can be used to predict the severity of exacerbation of COPD. Also, Rahimirad et al., 2017 [14] found that the elevation of neutrophil to lymphocyte ratio was an independent prognostic biomarker for hospital mortality in AECOPD. In addition, other studies reported that the neutrophil to lymphocyte ratio was decreased in AECOPD patients after recovery of the exacerbation than before [12,15]. Likewise, we found a significant elevation of the mean (SD) of neutrophil to lymphocyte ratio in stable COPD patient group than healthy control group. This result was in agreement with In et al., 2016 study [16], who demonstrated that there was an increase in the neutrophil to lymphocyte ratio in a stable COPD group when compared with the healthy control group. Also, we found a significant elevation of circulating neutrophil count in AECOPD than stable COPD in contrast to circulating lymphocyte count which it has a significant reduction in AECOPD than stable COPD. A study by Jaroenpool et al 2016 [17] demonstrated a significantly increased of circulating neutrophil percentage with decrease of phagocytic functions in heavy smoker COPD patients in contrast to circulating lymphocyte percentage which decreased in COPD patients.In the current study, we found a significant elevation in the levels of circulating total leukocytic count, neutrophil count, and neutrophil to lymphocyte ratio, but significantly decreased of lymphocyte count in stable COPD patients than in the healthy control group. This result was in agreement with a study done by Günary et al 2014 [6]. Şahin et al 2019 [18] recognized a lower circulating lymphocyte count in COPD patients with acute exacerbated than those in a stable stage or healthy control and in lower also in stable COPD patients than in healthy control. These result suggested that there is an ongoing mild degree in stable COPD patients.In this study we found the neutrophil to lymphocyte ratio was significant correlated with CRP in AECOPD patients. This result in agreement with In et al., 2016 [16], and Farah et al. 2017 [19] studies, they reported a significant positive correlation between neutrophil to lymphocyte ratio and CRP.We found a slight elevation of total CAT score but not significant in AECOPD group of patients when compared to the stable COPD group of patients. Previous studies have found that the CAT score worsen with the COPD severity and was correlated with the disease progression [20].Hence, our results suggested that the neutrophil to lymphocyte ratio was increased when the severity of COPD was progressed. A similar finding was reported by Yousef and Alkhiary study 2017 [21] who found that neutrophil to lymphocyte ratio was elevated with the severity of COPD. A previous study also showed that the neutrophil to lymphocyte ratio increased with the severity of airflow obstruction and emphysematous change, suggesting that the neutrophil to lymphocyte ratio may reflect the extent of airflow obstruction [22-24].In our study, there was a significant inversely correlation between neutrophil to lymphocyte ratio and airflow limitation expressed by FEV1, and FEV1/FVC. Our result was similar to the finding of Lee et al. study 2016 [25] and Furutate et al. study 2016 [22] they found that the neutrophil to lymphocyte ratio was a significant inversely correlated with FEV1%. Also, Karatas et al. 2019 [26] showed the same result which found a negative correlation between neutrophil to lymphocyte ratio and FEV1. Furthermore, another study reported that the circulating neutrophil count was inversely correlated with FEV1% [27]. In contrast, a study found that the neutrophil to lymphocyte ratio was not correlated with FEV1. However, there was a significant correlation between neutrophil to lymphocyte ratio and mMRC, and also between neutrophil to lymphocyte ratio and 6MWT [25]. Rhee et al. 2018 [28] found the circulating neutrophil count was not correlated with FEV1% or the severity of asthma.Based upon the previous results, the neutrophil to lymphocyte ratio is superior to circulating neutrophil count alone or circulating lymphocyte count alone for the assessment of the severity of COPD [18].
6. Conclusions
- The neutrophil to lymphocyte ratio can be used as a follow-up inflammatory marker for acute exacerbation of COPD patient and also to assess the progression and the severity of the disease. Particularly, it is an easily done and cheap inflammatory marker.
ACKNOWLEDGMENTS
- We would like to thank full all the professors in the Clinical Pathology department.
References
| [1] | Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu Let al. The nature of small airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350: 2645–53. |
| [2] | Schmidt SA, Johansen MB, Olsen M, Xu X, Parker JM, Molfino NA, et al. The impact of exacerbation frequency on mortality following acute exacerbation of COPD: a registry-based cohort study. MJ Open. 2014;4: 12 e006729. |
| [3] | Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet 2009;374:733-43. |
| [4] | Jones PW, Agusti AG. Out comes and markers in the assessment of chronic obstructive pulmonary disease. Eur Respir J. 2006;27 (4): 822–32. |
| [5] | Suiss S, Dwll’ Anillo, Ernst P. Long-term natural history of chronic of chronic obstructive pulmonary disease: severe exacerbation and mortality. Thorax.2012; 67:957-963. |
| [6] | Günary E, Sarinc Ulasl S, Akar O, Ahsen A, Günary S, Koyuncu T, et al Neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease: a retrospective study. Inflammation. 2014; 37:374-380. |
| [7] | Balta S, Celik T, Mikhailidis DP, Oturk C, Demirkol S, Aparci M, et al, The relation Between Atherosclerosis and the Neutrophil-to-lymphocyte ratio. Clin Appl Thromb Hemost. 2016; 22: 405-411. |
| [8] | Paliogiannis P, Fois AG, Sotgia S, Mangoni AA, Zinnellu E, Pirina P, et al, Neutrophil-to-lymphocyte ratio and Clinical outcomes COPD: recent evidence and future perspective. Eur Respir Rev. 2018; 27: 170113. |
| [9] | Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The Platelet-to-Lymphocyte Ratio as an Inflammatory Marker in Rheumatic Diseases. Ann Lab Med. 2019; 39:345-357. |
| [10] | Vogelmeier CF, Criner GJ, Martine FJ, Anzueto A, Barnes PJ, Bourbeau J, et al., Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017 1;195: 557-582. |
| [11] | Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates, et al., SERIES “ATA/ERS TASK FORCE: STANDARDISATION OF LUNG FUNCTION TESTING” Number 2 in this Series Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. |
| [12] | Taylan M, Demir M, Kaya H, et al. Alterations of the neutrophil-lymphocyte ratio during the period of stable and acute exacerbation of chronic obstructive pulmonary disease patients. Clin Respir J. 2017;11:311–317. |
| [13] | Aksoy E, Karakurt , Gungor S, Ockli B, Omen I, Yildirim E, et al., Neutrophil to lymphocyte ratio is a better indicator of COPD exacerbation severity in neutrophilic endotypes than eosinophilic endotypes. Int J Chron Obstruct Dis. 2018;13:2721-2730. |
| [14] | Rahimirad S, Ghaffary MR, Rahimirad MH, Rashidi F. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease. Tuberk Toraks. 2017;65:25-31. |
| [15] | Kumar P, Law S, Sriram KB. Evaluation of platelet lymphocyte ratio and 90-day mortality in patients with acute exacerbation of chronic obstructive pulmonary disease. J Thorac Dis. 2017; 9:1509-1516. |
| [16] | İn E, Kuluöztürk M, Öner Ö, Deveci F. The Importance of Neutrophil-to-Lymphocyte Ratio in Chronic Obstructive Pulmonary Disease. Turk Thorac J. 2016;17:41-46. |
| [17] | Jaroenpool J, Pattanapanyasat K, Noonin N, Prachongsai l. Aberrant neutrophil function among heavy smokers and chronic obstructive pulmonary disease patients. Asian Pac J Allergy Immunol. 2016 Dec;34:278-283. |
| [18] | Fün Sahin, Ayse Filiz Kosar, Aslan Buru Aslan, Burcu Yiğitbas Uslu. Serum biomarkers in patients with stable and acute exacerbation of chronic obstructive pulmonary disease: a comparative study. J Med Biochem. 2019; 38: 1–9. |
| [19] | Farah R, Ibrahim R, Nassar M, Najib D, Zivony Y, Eshel E. The neutrophil/lymphocyte ratio is a better addition to C-reactive protein than CD64 index as a marker for infection in COPD. Panminerva Med. 2017;59:203–209. |
| [20] | Tu YH, Zhang Y, Fei GH. Utility of the CAT in the therapy assessment of COPD exacerbations in China. BMC Pulm Med. 2014;14; 42. |
| [21] | Yousef AA, Alkhiary W, Role of Neutrophil-to-lymphocyte ratio in prediction of acute exacerbation of chronic Obstructive Lung Disease. Egyptian Journal of Chest Diseases and Tuberculosis.2017; 66, 43-48. |
| [22] | Furnutate R, Ishii T, Motegi T, Hattori K, Kusunoki Y, Gemma A, et al., The Neutrophil to Lymphocyte Ratio Is Related to Disease Severity and Exacerbation of Patients with chronic obstructive pulmonary disease. Intern Med. 2016;55: 223-229. |
| [23] | Kalemci S, Akin F, Sarihan A, Sahin C, Zeybek A, Yilmaz N. The relationship between hematological parameters and the severity level of chronic obstructive lung disease. Pol Arch Intern Med. 2018;128:171-177. |
| [24] | Teng F, Ye H, Xue T. Predictive value of neutrophil to lymphocyte ratio in patients with acute exacerbation of chronic obstructive pulmonary disease. PLoS One. 2018; 13:e02 04377. |
| [25] | Lee SJ, Lee HR, Lee TW, Ju S, Lim S, Go Sl et al., Usefulness of neutrophil to lymphocyte ratio in patients with chronic obstructive pulmonary disease. A prospective observational study. Korean J Intern Med. 2016; 31: 891–898. |
| [26] | Karatas M, Gündüzöz M, Özis TN, Özakinci OG, Ergün D. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as hematological indices of the inflammatory response in ceramic workers' silicosis. Clin Respir J. 2019;13: 159-165. |
| [27] | Barnes PJ, Celli BR. Systemic manifestation and comorbidities of COPD. European Respiratory Journal. 2009; 33: 1165-1185. |
| [28] | Rhee H, Love T, Harrington D. Blood Neutrophil Count is Associated with Mass Index in Adolescents with Asthma. JSM Allergy Asthma. 2018; 3: 1019. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML