-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(9): 332-336
doi:10.5923/j.ajmms.20190909.05

Long-Term Outcomes of Patients Undergoing Living-Related Kidney Transplantation
Feruz Gafurovich Nazirov, Ravshan Aliyevich Ibadov, Fazliddin Shamsitdinovich Bakhritdinov, Zokhidjon Turdaliyevich Matkarimov, Sardor Khamdamovich Ibragimov
Republican Specialized Scientific-Practical Medical Center of Surgery named after Academician V.Vakhidov, Tashkent, Uzbekistan
Correspondence to: Sardor Khamdamovich Ibragimov, Republican Specialized Scientific-Practical Medical Center of Surgery named after Academician V.Vakhidov, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

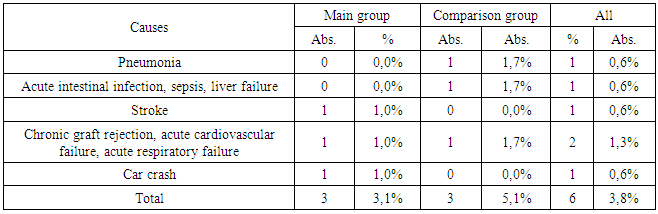
Objective: this study aimed to assess long-term outcomes of living-related kidney transplantation. Methods: We analyzed the long-term outcomes of 159 patients undergoing living-related kidney transplantation from 2010 to 2018 in Republican Specialized Scientific-Practical Medical Center of Surgery named after Academician V.Vakhidov (Tashkent, Uzbekistan). New optimized method was performed for the main group (n=98) observed since February 2018, the comparison group included 61 cases from 2010 to February 2018 operated in the traditional way. Results: Graft rejection was observed in 5 (5.2%) recipients of the main group and in 6 (10.2%) recipients from the comparison group. Post-transplantation diabetes mellitus developed in 13 (8.3%) recipients out of the total, in 8 (8.2%) and 5 (8.5%) cases of the main and comparison groups, respectively. Pulmonary tuberculosis observed in the comparison group in 2 (3.4%) cases. Acute respiratory failure reported in 3 (3.1%) recipients of the primary and 5 (8.5%) recipients of the comparison group. The most frequent cause of death (1.3%; 2 cases) in the late postoperative period was chronic graft rejection with the development of acute respiratory and cardiovascular failure. Pneumonia, as the cause of death, was observed in 1 (0.6%) case of the comparison group. Acute intestinal infection, sepsis and liver failure was observed in 1 (0.6%) recipient from the comparison group. Brain stroke caused death in 1 (1.0%) case in the main group. Conclusion: The development of a national protocol including recommended international guidelines for management of patients with end-stage renal failure and improving of tactical and technical aspects reduced the incidence of complications in the long-term period from 47.5% to 22.7% and the mortality rate from 8.2% to 4.1% (P=0.029).
Keywords: Kidney transplantation, Living-related renal transplant recipients, Long-term outcomes
Cite this paper: Feruz Gafurovich Nazirov, Ravshan Aliyevich Ibadov, Fazliddin Shamsitdinovich Bakhritdinov, Zokhidjon Turdaliyevich Matkarimov, Sardor Khamdamovich Ibragimov, Long-Term Outcomes of Patients Undergoing Living-Related Kidney Transplantation, American Journal of Medicine and Medical Sciences, Vol. 9 No. 9, 2019, pp. 332-336. doi: 10.5923/j.ajmms.20190909.05.
1. Introduction
- Kidney transplantation is characterized by optimal results in terms of the duration and quality of life of patients and, accordingly, is considered the gold standard of renal replacement therapy [1-3]. Organ transplantation of living donors has a lower incidence of graft rejection, as well as more satisfactory patient survival rates. Kidney transplantation from a related donor is a pre-planned operation, which in some cases completely avoids dialysis therapy [4,5]. Recently observed increasing of living kidney donors. Laparoscopic donor nephrectomy has a shorter duration of disability and fewer days of hospitalization, will further increase the number of living donors [6,7].In the conditions of the national health care system, kidney transplantation, as a radical form of treatment of chronic renal insufficiency, is at the stage of dynamic improvement. In this connection, the main the main aim was to assess long-term outcomes of living-related kidney transplantation.
2. Methods
- We analyzed the long-term outcomes of 159 patients undergoing living-related kidney transplantation from 2010 to 2018 in Republican Specialized Scientific-Practical Medical Center of Surgery named after Academician V.Vakhidov (Tashkent, Uzbekistan). Modern principles of diagnosis and treatment were used then laboratory and instrumental studies handled to follow up the immediate and long-term results of related kidney transplantation. The main group consisted of 98 cases observed since February 2018, in which kidney transplantation was performed according to a new optimized method, the comparison group included 61 cases from 2010 to February 2018 operated in the traditional way.Among the recipients of both groups, patients aged from 20 to 44 years prevailed. Male recipients were 135 (84.9%) cases.The main cause (95.6%) of renal failure was chronic glomerulonephritis, chronic pyelonephritis was detected in 1 (0.6%) case, 1 recipient (0.6%) suffered from type I diabetes, in 2 (1.2%) of the cases had urolithiasis, in 1 (0.6%) of the patient - chronic renal disease of unknown etiology, and in 1 (0.6%) of the cases polycystic kidney disease was detected.
3. Results
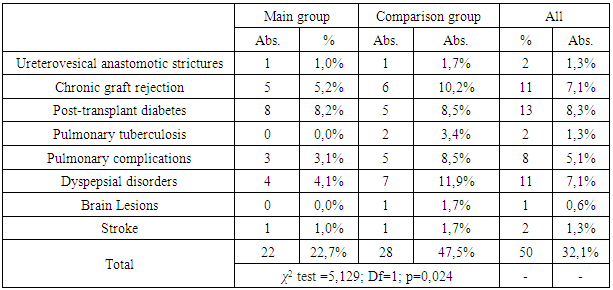
- So, total complications in the late postoperative period were observed in 50 (32.1%) cases out of the total number of recipients studied, 22 (22.7%) in the main group and 28 (47.5%) in the comparison group (P=0.024).We observed chronic graft rejection in 5 (5.2%) recipients of the main group and in 6 (10.2%) recipients from the comparison group. Post-transplantation diabetes mellitus, as the most frequent long-term complication, developed in 13 (8.3%) recipients out of the total, in 8 (8.2%) and 5 (8.5%) cases of the main and comparison groups, respectively. Pulmonary tuberculosis was observed only in the comparison group in 2 (3.4%) cases. Pulmonary complications with the development of acute respiratory failure were reported in 3 (3.1%) recipients of the primary and 5 (8.5%) recipients of the comparison group.Dyspepsial disorders were relatively frequent complications of the long-term period after kidney transplant and accounted for 7.1% (11 cases) of the total number of recipients.Among the treatments taken in transplanted kidney function failure, hemodialysis, graft removal and retransplantation can be distinguished. In the late postoperative period 3 recipients from the main group and the comparison group needed hemodialysis. Retransplantation was carried out only in the comparison group in 2 (3.4%) cases. Removal of the graft in violation of its function was performed in 2 (2.1%) cases of the main one and also in 2 (3.4%) cases of the comparison group (Fig. 1).
|
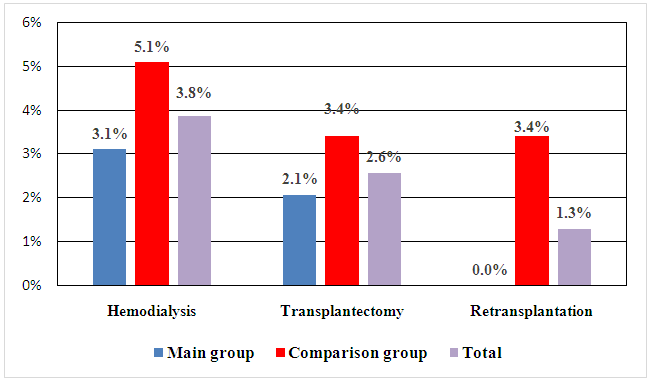 | Figure 1. Types of treatment taken for transplanted kidney function failure |
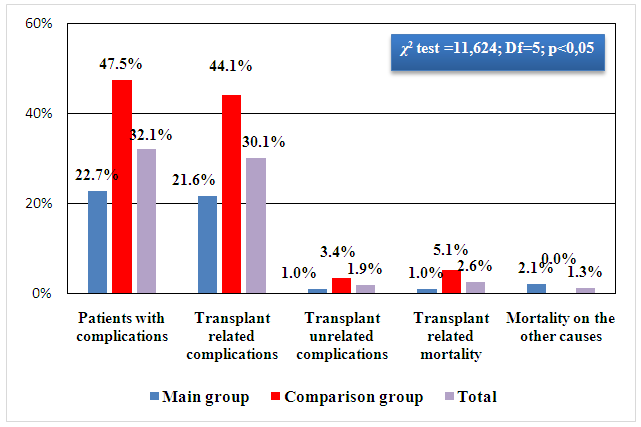
 | Figure 2. The distribution of patients according to the characteristics of complications |
|
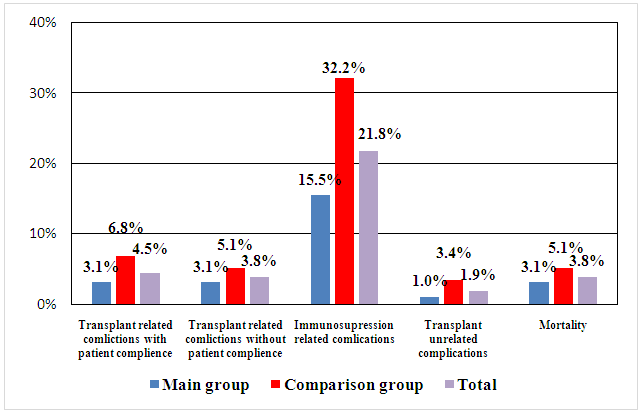
 | Figure 3. The frequency of complications and mortality, depending on the cause |
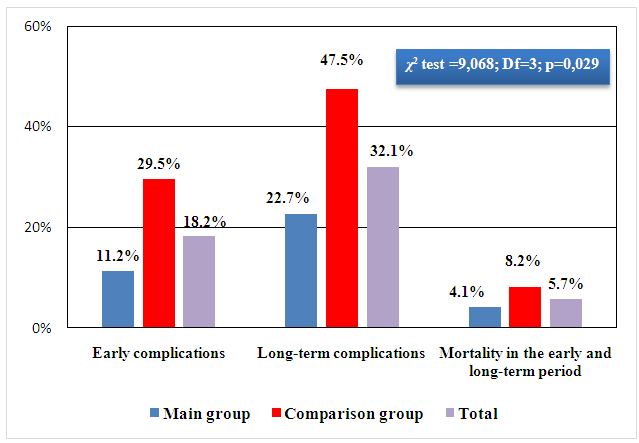 | Figure 4. Composite data of complications and mortality in the early and long-term periods after kidney transplantation |
4. Conclusions
- The development of a national school of live-related kidney transplantation, protocol of diagnosis and management of patients with end-stage renal failure for surgery including recommended international guidelines, as well as improving of tactical and technical aspects of surgical intervention, reduced the incidence of complications in the near postoperative period from 29.5% to 11.2% in the long-term period from 47.5% to 22.7% and the mortality rate from 8.2% to 4.1% (P=0.029).
ACKNOWLEDGEMENTS
- This work was supported by Republican specialized scientific–practical medical center of surgery named after academician V.Vakhidov, Tashkent, Uzbekistan.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML