-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(9): 329-331
doi:10.5923/j.ajmms.20190909.04

The Role of Immunohistochemical Markers at Metastasis of Breast Cancer in the Lungs
Alimkhodjaeva L. T., Shadmanova D. S., Zakirova L. T., Khodjayev A. V., Nigmanova N. A., Norbekova M. Kh., Zakhirova N. N., Yusupova N. B., Mirzaeva N. T.
Republican Specialized Scientific-Practical Medical Center of Oncology and Radiology Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Breast cancer is a serious medical and social problem for most developed countries of the world. Immunohistochemical studies were performed on primary tumors of 62 breast cancer patients with lung metastases. Immunohistochemical study allows to evaluate the indicators in connection with the tumor cell cycle. Knowledge of immunohistochemical markers allows developing an optimal model for assessing the risk of breast cancer metastasis.
Keywords: Breast cancer, Tumor, Metastases, Immunohistochemical markers
Cite this paper: Alimkhodjaeva L. T., Shadmanova D. S., Zakirova L. T., Khodjayev A. V., Nigmanova N. A., Norbekova M. Kh., Zakhirova N. N., Yusupova N. B., Mirzaeva N. T., The Role of Immunohistochemical Markers at Metastasis of Breast Cancer in the Lungs, American Journal of Medicine and Medical Sciences, Vol. 9 No. 9, 2019, pp. 329-331. doi: 10.5923/j.ajmms.20190909.04.
1. Introduction
- In spite of the significant achievements of the last quarter of a century in understanding the biology and clinic of the disease, as well as fundamental changes in the approach to treatment, the problem of breast cancer continues to be highly relevant, especially in the Republic of Uzbekistan, where, upon initial detection, 75% of women already have stage 4 of breast cancer with distant metastases. Another depressing factor is the rejuvenation of the disease in our Republic. The disease occurs not only at the age of 25-30 years but also in girls of younger age (19-20 years). There is no single laboratory for immunohistochemical research in the Republic, except for private sectors. And we know that personalized and modern treatment cannot be of high quality and effective without determining biological subtypes.A number of molecular markers are important for determining the prognosis and choice of therapy for metastatic breast cancer in the lungs [8,10]. Many studies have obtained evidence of the large prognostic value of such immunohistochemical markers as epidermal growth factor HER2-neu, tissue markers of proliferation and apoptosis. A breakthrough in the field of practical use of these markers occurred after the appearance of the drug Herceptin which is a humanized antibody to HER2-neu, one of the tyrosine kinase receptors of the erbB family. This is one of the most important regulatory systems for mitogenic signal transmission. Blocking of HER2-neu can significantly slow or stop tumor growth depending on such stimuli [1-5,9]. Numerous studies have been devoted to the study of the role of the p-53 gene – a suppressor which is localized in the 17th chromosome. Mutation in this gene leads to dysregulation of the cell cycle and apoptosis. Laboratory studies have shown that cells with p53 mutation are resistant to radiation and chemotherapeutic agents that usually cause apoptosis. There are some reports of a negative effect of p-53 on relapse-free and overall survival [6,7].Ki-67 is a nuclear antigen expressed in the proliferative phase of the cell cycle. A correlation between the number of cells expressing Ki-67 and the degree of tumor malignancy, as well as the mitotic index was established [6,8,9].The aim of the study was to study the data of immunohistochemical studies at metastasis of breast cancer in the lungs.
2. Materials and Methods
- Immunohistochemical studies were performed on primary tumors of 62 breast cancer patients with lung metastases. Immunohistochemistry (IHH) of archival material was conducted in a private laboratory “Premium Diagnostics LTD” on the equipment Dako Denmark A / S, Dania Dakoproduktionsvej 42, DK-2600 Glostrup Denmark. Evaluation of the results of treatment began with a statistical analysis of the prognostic values of the signs that affect the outcome of the disease, which was based on three main types of contingency tables:- The dependence of the disease progression and the negative response to the conducted treatment on the severity of a separate prognostic factor;- The dependence of the distribution of the some sign’s evidence degree from the another sign’s evidence degree;- The dependence of the disease progression in patients from a combination of several factors evidence degrees.The basis of evidence-based statistics was as follows: factor analysis with the determination of the specific weight of each trait influencing the outcome of the disease for the highlight of common factors; nonparametric (rank) correlation analysis by the method of Kendall (Rk) for determining the relationship between indicators; the criterion of the angular Fisher transformation (F*), the criterion of compliance (consent) of Pearson (x2), the criterion of relative risk (RR and 1 / RR) for detection of the differences. Four main levels of statistical significance were adopted to determine the differences: high - p <0.001, average p <0.01, low (marginal) p <0.05, insignificant (unreliable) - p> 0.05. The main verifiers of the differences reliability were the results of the multifunctional (universal) Fisher’s methods. The IBM SPSS 18 program was used for statistical processing. 4-5 micron thick sections were made from each paraffin block of a cancerous breast tumor using a Leica SM 2000R microtome (Sliding Microtome for Routine Applications) and then processed by standard methods. Antibodies to estrogen, progesterone, androgen receptors, oncoprotein, Her2 / neu, Ki67 of the DAKO company were used.
3. Results and Discussions
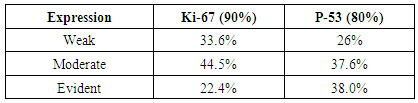
- Occurrence frequency of tumors with HER2-neu hyperexpression made up 58%, while tumors with a negative HER2-neu status were observed in 15% of cases. The expression of HER2-neu as a prognostic factor is statistically correlated with the expression of estrogen receptors (ER) and progesterone receptors (PR). When assessing the hormonal status by an immunohistochemical method positive expression of estrogen receptors was detected in 35% of observations: weak was observed in 57.9% of observations, moderate – in 28.7%, evident – in 14.5% of observations.The expression of progesterone receptors was noted in 45% of cases: evident expression was detected in 22.8% of cases, moderate – in 22.4% and weak – in 55.6% of cases (Fig. 1). The expression of HER2-neu was noted in 70% of studies: evident positive expression was observed in 35.7% of cases, moderate – in 50.8% of observations, weak – in 14.4% of cases. An increase of HER2-neu expression is accompanied by a decrease of ER expression in 75% of observations and a decrease of PR expression in 80% of observations (P <0.05).
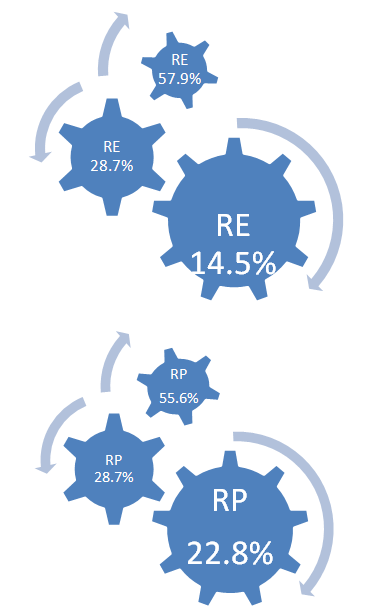 | Figure 1. Expression of progesterone and estrogen receptors |
|
4. Conclusions
- Thus, when comparing the expression level of the markers as the tumor progresses, an increase of expression in the metastatic node in the lungs is observed in compare with the expression of the markers in the primary tumor. However, it is impossible to assess the role of these markers in metastasis of breast cancer in the lungs in isolation. When analysing the prognostic factors for metastasis to the lungs and pleura, it is necessary to take into account, such tumor indicators as the morphological structure of the tumor, the degree of malignancy, the degree of differentiation of the tumor cell and, of course, its receptor status along with immunohistochemical progression markers.Molecular biological phenotypes of breast cancer on the territory of Uzbekistan are not sufficiently studied, primarily due to the small number of patients who underwent immunohistochemistry (IHC) which is necessary for developing tactics of effective treatment in each specific case of breast cancer, which is associated with the lack of routine practice of IHC of tumor research in terms of reference laboratory of oncologic institutions. The obtained data will allow us, oncologists, to identify heterogeneous biological subtypes of the mammary gland tumor, which is the main one in modern oncology in the choice of treatment strategy. This field is not sufficiently studied in the Republic of Uzbekistan and that is why our results will be of great help for practitioners.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML