-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(9): 325-328
doi:10.5923/j.ajmms.20190909.03

Diagnostic Significance of Molecular Genetic Markers in the Prognosis of the Breast Cancer Clinical Course
Alimkhodjaeva L. T., Narzieva D. F., Zakirova L. T., Khodjaev A. V., Nigmanova N. A., Norbekova M. Kh., Zakhirova N. N., Yusupova N. B., Mirzaeva N. T.
Republican Specialized Scientific-Practical Medical Center of Oncology and Radiology, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

From year to year the awareness of the female population about the need for self-examination and clinical examination is increasing, diagnostic equipment is being improved and optimal diagnostic and treatment algorithms are being developed. The result of the work, ultimately, is a progressive improvement treatment results. Standard prognostic factors that predict the course of breast cancer include the following parameters: patient's age, tumor size, change in lymph and peripheral lymph nodes, histological type of tumor, degree of malignancy, estrogen and progesterone receptors.
Keywords: Estrogen, Progesterone, Breast cancer, Tumor, Lymph node, Receptor
Cite this paper: Alimkhodjaeva L. T., Narzieva D. F., Zakirova L. T., Khodjaev A. V., Nigmanova N. A., Norbekova M. Kh., Zakhirova N. N., Yusupova N. B., Mirzaeva N. T., Diagnostic Significance of Molecular Genetic Markers in the Prognosis of the Breast Cancer Clinical Course, American Journal of Medicine and Medical Sciences, Vol. 9 No. 9, 2019, pp. 325-328. doi: 10.5923/j.ajmms.20190909.03.
1. Introduction
- The morbidity of breast cancer (BC) in recent years has been steadily increasing [1,2]. The histological form of the tumor is one of the traditional morphological factors of the prognosis of the clinical course of breast cancer. Various morphological forms of breast cancer differ in the aggressiveness of the clinical course [11]. For example, it is known that the medullary breast cancer is characterized by a more favorable prognosis compared with other forms of breast cancer and an invasive lobular breast cancer metastasizes less frequently than an invasive ductal one [10]. According to the WHO data the most common histological form of breast cancer is invasive ductal. It occurs in 59% of cases. The second most frequent breast cancer is invasive lobular breast cancer which makes up 25% of cases [3,9,11]. The leading factor in the mechanism of malignant cells transformation, in the biological behavior of already arisen tumors, is the increased proliferative activity of the tumor cells themselves [4-8,12]. The existing methods of risk assessment in patients with breast cancer are ineffective and insufficient. The significance of individual markers identified by immunohistochemistry remains controversial. The prognostic role of immunohistochemical methods of diagnosis in assessing the effectiveness of therapy and determining the prognosis of the disease after antitumor treatment requires clarification.The aim of the study was to identify the expression of molecular genetic markers and determine their diagnostic value for prognosis the clinical course of breast cancer.
2. Material and Methods
- 200 patients with breast cancer of stage I-II admitted to the Department of Mammalogy of the Republican Specialized Scientific-Practical Medical Center of Oncology and Radiology were included in the examined group. All patients underwent a comprehensive examination in the center. A cor-biopsy and histological examination were performed to clarify the nature of the mammary gland neoplasm. An avidin-biotin antibody imaging method was used for immunohistochemistry. Antibodies by “DAKO” company (Denmark) were used. ABC-Kit (universal) was used as a visualization system. DAB by Pharmingen was used to identify the color staining of the reaction result.
3. Results and Discussion
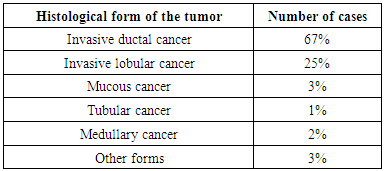
- The predominant histological form of breast cancer in our study was invasive ductal cancer which occurred in 67% of cases. Invasive lobular cancer was detected in 25% of cases. Mucous cancer was detected in 3%, tubular cancer - in 1%, medullary - in 2% of cases. Other forms made up 3% (Tab. 1).
|
 | Figure 1. Hyper-expression results of HER2-neu, ER and PR receptors |
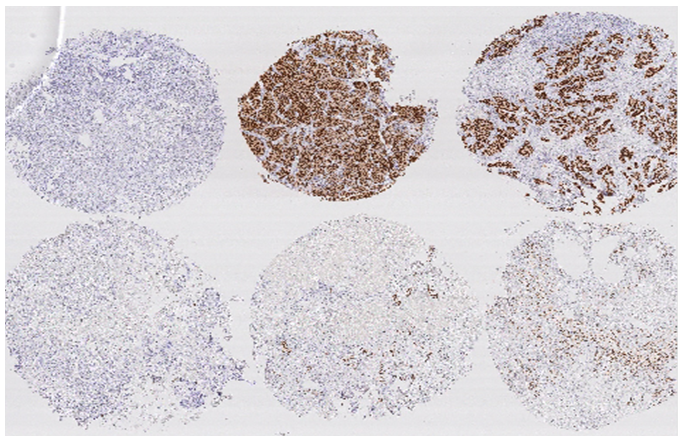 | Figure 2. Fragment of the matrix stained with antibodies to estrogen receptors (ER) |
4. Conclusions
- Thus, tumors with reduced PR expression are characterized not only by high expression of the HER2-neu oncoprotein, but also by an increased level of cells proliferative activity. In this study we showed that the content and expression level not only of ER is an important prognostic factor of the breast cancer clinical course, but also the content and expression level of PR are key points in predicting the breast cancer course and can also serve as a predictive criterion for antitumor therapy. The prognostic value of the content and expression level of PR (especially its decline) as a marker of an unfavorable prognosis and the breast cancer course is confirmed in the result of an integrated approach to this problem. The results of the study also confirm that the hyper-expression of the HER2-neu oncoprotein is an independent factor of a poor prognosis of the disease and is associated with the tumor high metastatic potential.The lack of data on the biological heterogeneity of breast cancer in patients on the territory of Uzbekistan, the absence of a full-fledged laboratory for immunohistochemical research makes it difficult to create effective screening and treatment programs. It is, of course, a huge social and economic problem in our region. The data on molecular genetic studies allow us to single out the heterogeneous biological phenotypes of this disease, which is the main one in modern oncology in choosing a treatment strategy in each specific case. The biological subtypes of the tumor exactly determine the tactics of treatment and the outcome of the disease. The biological heterogeneity of breast cancer remains insufficiently studied in Uzbekistan. The problem of breast cancer treatment is now becoming increasingly important due to the growth in the incidence rate which is proportional to the increase in life expectancy of the population of our country. This fact is aggravated by the late treatment of many patients. The issue of choosing a method of special therapy for this pathology, especially depending on the biological types of the tumor, remains controversial up to now. At the breast cancer there remains an unresolved question of risk stratification in patients depending on the presence and absence of prognostic significant clinical, biological, genetic factors, there is no clear data on the immediate and long-term results of treatment. Taking into account all mentioned above, this article is relevant, and the proposed development has a certain scientific interest, theoretical significance and importance for our further researches.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML