J. A. Rizaev, Yunuskhodjayeva M. K.
Department of Faculty Therapeutic Dentistry, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Yunuskhodjayeva M. K., Department of Faculty Therapeutic Dentistry, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The prevalence of inflammatory periodontal diseases is extremely high and reaches, according to various authors, from 70 to 98%. In this regard, the improvement of methods of diagnosis and treatment of these diseases is a serious problem of dentistry. Currently the least studied pathology remains aggressive periodontitis (AP), during which the active destruction of the supporting tissues of the teeth begins at the young age and in relatively short a period of time leads to massive loss of teeth. The ordinary clinical examination data and X-ray picture in patients with AP leads to late diagnosis diseases that dictates the need to use molecular biological and immunological diagnostic methods, which are extremely useful and highly informative for early diagnosis of AP, clarification of the nature, degree of activity and depth damage of periodontal tissues.
Keywords:
Generalized aggressive periodontitis, Dental, Periodontal disease, Paraclinical diagnostic methods
Cite this paper: J. A. Rizaev, Yunuskhodjayeva M. K., Features of the Aggressive Forms of Periodontitis Course, American Journal of Medicine and Medical Sciences, Vol. 9 No. 8, 2019, pp. 311-313. doi: 10.5923/j.ajmms.20190908.08.
1. Introduction
Inflammatory periodontal diseases are the serious problem of modern dentistry due to the high prevalence, complexity of diagnosis, treatment and rehabilitation of patients. Currently the least studied pathology remains aggressive periodontitis (AP), during which the active destruction of the supporting tissues of the teeth begins at the young age and in relatively short a period of time leads to massive loss of teeth. The purpose of research was to study the clinical features of the aggressive form of periodontitis.
2. Methodology
During the clinical examination, the data of 34 patients with AP were assessed, the history of the patient’s complaints was taken into account, specifying the factors that in each case determined the occurrence of aggressive periodontitis and its course: hereditary burdens, bad habits, anatomical topographic features of the oral cavity.During studying the data of the anamnesis, aggravated family heredity in relation to periodontal diseases, when one or several immediate relatives suffered from periodontal diseases, was found in 20 (66.7%) patients with AP. The presence of such bad habits as smoking, adversely affecting the state of periodontal tissues, was noted in 14 (46.7%) patients with AP.Evaluating the age of periodontitis, 3 (10.0%) patients indicated that the first signs of the disease appeared less than three years ago, 11 (36.7%) - from 3 to 5 years, 16 (53.3%) - more than 5 years. It should be noted that most patients learned about their diseases already in the presence of severe destructive phenomena in the tissues periodontal, when teeth mobility appeared. According to the patients, they periodically noted an exacerbation of periodontitis, which was accompanied by the appearance of periodontal abscesse, an increase in tooth mobility, the occurrence of bleeding of the gums and painful feelings when eating.The frequency of exacerbations on average was 1 every 3-4 months. During the period of exacerbation of AP 9 (30.0%) patients noted the deterioration of the general condition of the body.
3. Result and Discussion
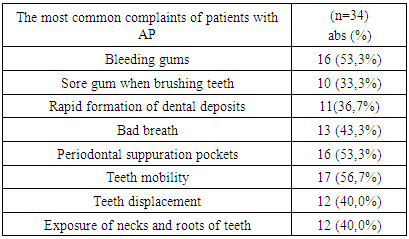
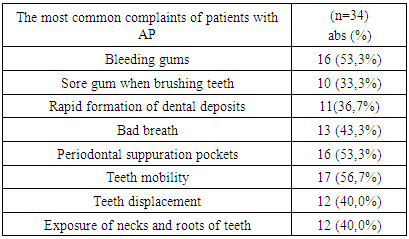
Treatment of periodontitis, which consisted of the removal of dental deposits, opening abscesses, antiseptic treatment of the oral cavity, systemic antibiotic therapy was performed previously in 6 (20.0%) patients with AP.According to the patients, in most cases the treatment was ineffective, the positive effect was short-term and lasted no more than 4-5 months, only 3 (10.0%) reported that they had periods of remission and disease with a duration of 6-8 months.During the survey, patients with AP most often show complaints of gingival bleeding and pain when brushing teeth, abscess formation, rapid formation of dental deposits, bad breath, periodically occurring suppuration from periodontal pockets, mobility and movement of teeth, exposure of the necks and roots of teeth and, as a result, increased sensitivity of teeth to temperature and taste irritants (Table 1).Table 1. The most common complaints of patients with AP
 |
| |
|
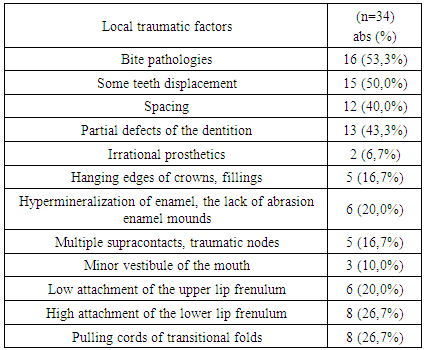
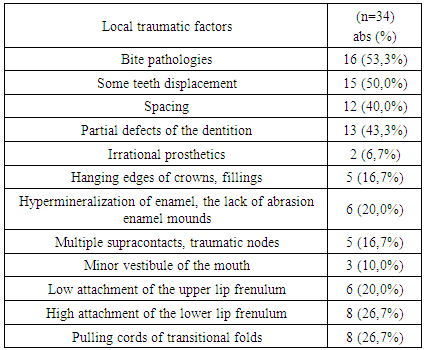
As it turned out from the survey, only 13.3% of patients in both groups were motivated for regular oral care and only a few were trained in the technique of cleaning teeth and interdental spaces. All patients noted a significant deterioration in the quality of life, as a result of significant destruction of periodontal tissues and teeth mobility and loss, the chewing function was disturbed and cosmetic defects of dental arches appeared.During the examination of the oral cavity, various local traumatic factors, and often a combination of several of them were found (table 2).Table 2. The prevalence of local traumatic factors in patients with AP
 |
| |
|
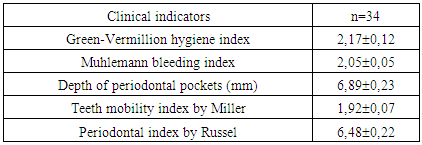
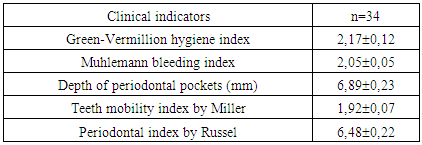
It should be noted that in 18 (60.0%) patients with AP during the examination there were no marked signs of acute inflammation of the mucous membrane of the gingival margin - hyperemia and edema. 12 (40.0%), who turned in the period of exacerbation, on the contrary, revealed severe edema and hyperemia of the gingival margin, a large amount of soft dental deposits and tartar, severe bleeding of the gums, tooth mobility, pain on palpation, periodontal abscesses.An objective examination in all patients revealed a generalized loss of periodontal attachment, a change in the configuration of the gingival papillae, significant recession.The severity of the destruction of periodontal tissues throughout the dentition, as a rule, was uneven. In patients, the most significant changes were found in the area of the anterior teeth of the lower jaw, the process was more common, marked destruction of periodontal tissues was observed in both the frontal and posterior teeth.Despite the severe destruction of periodontal tissues, oral hygiene of most of the examined patients was satisfactory. It should be noted that mild plaque is almost always combined with the tartar of a particular location. The greatest amount of dental plaque found on the anterior teeth of the lower jaw, in periodontal deep pockets, near teeth with high degree of mobility and with destruction of bone tissue in the area furcations of multiroot teeth. For an objective assessment of the hygienic condition of the oral cavity and the severity of the inflammatory-destructive process in periodontal tissues an index evaluation has been performed.Total hygiene index by Green and Vermillion, taking into account both the amount of plaque and tartar, was in average 2.17 ± 0.12.Table 3. Indicators of the index assessment of periodontal tissue in patients with AP (M ± m)
 |
| |
|
The severity of inflammation of periodontal tissues was assessed using the bleeding index by Miihlemann. This index has diagnostic value not only to identify the initial stages damage to periodontal tissues, but also with significant destructive changes in the periodontal complex. Average index value bleeding by Miihlemann was 2.05 ± 0.05.The depth of the periodontal pockets in patients with AP ranged from 5 to 10 mm, in some cases reached 12 mm or more. Average periodontal pockets depth was 6.89 ± 0.23 mm. When probing periodontal pockets, serous or purulent exudate was obtained, and in 9 (30.0%) patients, purulent discharge from periodontal pockets was noted even against the background of satisfactory oral hygiene and the absence of signs of acute inflammation in periodontal tissues.Taking into account the identified signs of tissue damage, the periodontal periodontal Russell index in all patients with AP was more than 4, which indicated a severe degree of damage. Refinement of the degree of spread of destructive changes from gum tissue on the marginal bone sections of the alveolar processes, as well as assessment of the nature, degree of their activity and the depth of bone destruction tissues were performed using X-ray.According to orthopantomography, it was revealed that all patients with AP have moderate and severe defeat of the bone base of the periodont that characterized by the almost complete disappearance of the compact plates, resorption of interalveolar partitions by 2 \ 3 or more of their heights, the expressed phenomena of osteoporosis. The destructive process was generalized, but areas of destruction had a different depth in different parts of the alveolar process. It should be noted that not always clinically determined depth of periodontal pockets, severity of bone destruction and the degree of mobility of the teeth corresponded to the severe inflammatory and destructive process in the periodontal bone tissue, revealed radiologically.In 7 (23.3%) patients with AP with the absence of complaints, a satisfactory hygienic condition of the oral cavity and a moderately pronounced severity of clinical manifestations of the inflammatory-destructive process in the periodontal tissues, a significant active destruction of the alveolar bone observed radiologically.
4. Conclusions
The inconsistency of clinical examination data and X-ray picture in patients with AP leads to late diagnosis diseases that dictates the need to use paraclinical diagnostic methods (molecular biological, immunological), which are extremely useful and highly informative for early diagnosis of AP, clarification of the nature, degree of activity and depth damage of periodontal tissues. Patients with AP aged over the 35 with a long course of the disease (10 and more years), have severe destructive changes in the soft tissues and periodontal bone structures, due to frequent exacerbations of the disease and treatment failure.
References
| [1] | Kaner, D., Bernimoulin, J.P., Hopfenmtiller, W. et al. Controlled delivery chlorhexidine chip versus amoxicillin/metronidazole as adjunctive antimicrobial therapy for generalized aggressive periodontitis: a randomized controlled clinical trial., J. Clin. Periodontol. (36)4, №10. 880-91, 2017. |
| [2] | Buchmann, R., Nunn, M.E., Dyke, Т.Е. et al. Aggressive periodontitis: 5-year follow-up of treatment, J. Periodontol. (73)6. 675-83, 2002. |
| [3] | Closs, L.Q., Gomes, S.C., Oppermann, R.V. et al. Combined periodontal and orthodontic treatment in a patient with aggressive periodontitis: 9-year follow-up report. World J. Orthodont. (11)3, 291-97, 2010. |
| [4] | Bulkina, N.V., Morgunova, V.M. Modern aspects of etiology and pathogenesis of inflammatory periodontal diseases. Features of the clinical manifestations of refractory periodontitis. Fundamental research. 2(part 2), 415-20, 2012. |
| [5] | Agafonova, E.V., Frolova, L.B. Optimization of complex medical activities in patients with rapidly progressive periodontitis. Medical Almanac. 2, 176-79. 2011. |
| [6] | Barer, G.M., Grigoryan, S.S., Surazhev, B.Y. et al. Research nature of pathogenic microflora of periodontal pockets at the stage local anti-inflammatory therapy. Materials of the All-Russian scientific and practical conference dedicated to the 105th anniversary of the birth of prof. E.E. Platonov. MSMDU. Moscow, 2017. |
| [7] | Bezrukova, I.V., Grudyanov, A.I. Aggressive forms of periodontitis. Guide for doctors. - Moscow: MIA, 2002. - 126 p. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML