-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(7): 249-254
doi:10.5923/j.ajmms.20190907.05

Bone Resection Features in Leg Amputation in Patients with Gangrene of Lower Extremities on the Background of Diabetes Mellitus
К. J. Matmurotov, S. S. Atakov, I. S. Sattarov, J. H. Otajonov, T. Sh. Atajanov
Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: К. J. Matmurotov, Department of General Surgery, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The results of the examination and treatment of 54 patients for 2015 - 2019 were analyzed with diabetic gangrene of the lower extremities, who received inpatient treatment with limb amputation at the level of the upper third of the leg. Analysis of the results of treatment of patients with diabetic gangrene of the limb showed that with the correct determination of the level of amputation of the lower extremities in 85.2% of cases it is possible to ensure a smooth postoperative course, with primary wound healing. The resection of the tibia without damaging the feeding artery made it possible to preserve the functional state of the knee joint even with the development of purulent complications in the wound area in 7 cases out of 8.
Keywords: Diabetes mellitus, Critical ischemia, Gangrene, Purulent-necrotic process
Cite this paper: К. J. Matmurotov, S. S. Atakov, I. S. Sattarov, J. H. Otajonov, T. Sh. Atajanov, Bone Resection Features in Leg Amputation in Patients with Gangrene of Lower Extremities on the Background of Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 9 No. 7, 2019, pp. 249-254. doi: 10.5923/j.ajmms.20190907.05.
1. Introduction
- One of the most severe complications of diabetes mellitus (DM) as a result of surgical manipulation is diabetic foot syndrome (DFS). DFS manifests itself in the form of the development of common purulent-necrotic lesions in the lower extremities, which develop in 35-60% of patients with diabetes [1,3]. In foreign and domestic epidemiological studies, the number of DFS ranges from 30% to 80% of the total number of patients with type 2 diabetes [2]. Such fluctuation of occurrence is associated with late negotiability, which is caused by asymptomatic diabetes mellitus. During treatment, patients often already have widespread purulent-necrotic lesions, even gangrene. [4,5].The prevalence of critical ischemia on the background of diabetes mellitus increases with age: among patients at the age of 40, it is about 3%, among patients at the age of 60 years - 9%. Of interest is the fact that from 10 to 50% of patients with diabetic foot syndrome never go to the doctor about the symptoms. Late treatment of purulent-necrotic lesions leads to loss of the limb [2,7].During the first year after verification of the diagnosis of critical lower limb ischemia (CLLI), 15–20% of patients with diabetes mellitus have a high limb amputation [8,10]. The immediate and long-term results of amputation largely depend on the level of truncation of the limb. Transtibial amputation is accompanied by half the mortality and has significantly higher prospects for subsequent rehabilitation [13]. The implied goal of amputation is to achieve primary wound healing of the lower limb at the most distal level possible. Energy consumption during movement increases with increasing amputation from the shin to the thigh. Preserving the knee joint and a significant segment of the tibia allows the use of lightweight prostheses, minimizes energy consumption during movement and allows older or weaker patients to walk independently [6,12].Historically, the level of the intended amputation was determined by a clinical examination of the lower limb by the surgeon immediately before the operation. The chosen site is usually evaluated further in the operating surgeon, who notes the appearance of the subcutaneous tissue and muscle and the presence or absence of bleeding from dissected tissues. The appearance of ischemic or necrotic tissue or the absence of bleeding at the edges of the incision often serve as a basis for attempting to perform amputation at a higher level [2,11,14].Convincing evidence that describe the role of subjective opinion in assessing the likelihood of wound healing after trans-femoral amputation was presented in a large study by J. Dormandy et al. [9]. Data were obtained for 713 patients who required amputation below the knee in 51 hospitals in 6 European countries. The results of the study showed that after 3 months, 59% of the stumps healed, 19% required an amputation at a higher level, and 11% remained unhealed. The surgeon's assessment of the likelihood of healing was incorrect in 21% of cases, when the operating surgeon believed that the postoperative wound would heal. It was also incorrect in 52% of cases when it was thought that wound healing would not take place.It is widely believed that an increase in the ratio of amputation below the knee and amputation above the knee should inevitably lead to a higher failure rate. However, this opinion is not confirmed by a comparative analysis of the results [13]. According to published studies on the frequency of late healing and revision after amputation below the knee, the frequency of primary healing ranged from 30 to 92% (70–75% on average), and the reamputation frequency ranged from 4 to 30% (average 15%). In approximately 15% more cases, later or secondary healing took place, which in some cases required rehabilitation and further operations, such as a wedge-shaped excision in order to preserve the length of the lower limb. Of the 30% of patients with amputation below the knee, in whom the wounds do not heal initially, approximately half require reamputation at a higher level. To heal a postoperative wound, more blood flow is needed than maintaining skin vitality without surgery. After wound healing with a high amputation below the knee, only 4% of patients later require a higher amputation [10].At the present time cannot be considered as an ideal criterion for the choice of the level of amputation. In general, the more often an attempt is made to save the knee, the more often it succeeds. Thus, the use of an aggressive brigade approach to amputations led to an increase in the ratio of amputation below the knee and amputation above the knee from an unusually low figure of 0.14 to 2.1.In connection with this problem, the purpose of this study was to improve the results of leg amputations taking into account the state of the angioarchitecture of the leg in patients with diabetic lower limb gangrene (DLLG).
2. Material and Methods
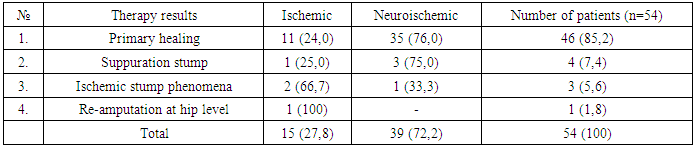
- The results of the examination and treatment of 54 patients for 2015 - 2019 were analyzed with diabetic gangrene of the lower extremities, who received inpatient treatment with limb amputation at the level of the upper third of the leg in the Republican center of purulent surgery and surgical complications of diabetes at the 2nd clinic of the Tashkent Medical Academy.The average duration of diabetes in patients was 13.7±4.5 years. The age of patients ranged from 26 to 81 years (on average, 53.1±5.2 years). Among the patients, there were 43 (79.6%) men and 11 (20.4%) women. The neuroischemic form of diabetic foot syndrome was diagnosed in 39 (72.2%) patients, ischemic - in 15 (27.8%). The duration of inpatient treatment of patients averaged 4-7 days.19 (35.2%) patients had signs of coronary heart disease (CHD), 8 (14.8%) patients had a history of myocardial infarction. In 11 (20.3%) patients, transient cerebral circulatory disorders occurred, 7 (13%) patients in the past suffered an acute cerebrovascular accident. In 21 (38.9%) patients, there was arterial hypertension.The instrumental method of assessing the state of the peripheral arterial bed was multispiral computed tomography (MSCT) of the lower limb arteries. After receiving information about the state of the peripheral arterial bed and the impossibility of restoring peripheral arterial blood flow, all patients underwent amputation of the tibia at the level of the upper third.Statistical data processing was carried out by using computer programs for statistical processing of the DBASE database and STAT4. For calculations, statistical methods for estimating differences in averages using Student’s t-test were utilized.All patients underwent amputation of the lower leg according to the method developed by us (patent RUz #IAP 2018 0251 of 06.06.2018) [1]. The technique of this method begins with the formation of the anterior and posterior skin and fascial flaps, which include the skin, subcutaneous tissue and its own fascia. After muscle incision and resection of the bones of the tibia, characterized in that the resection of the bones of the tibia is performed 12-15 cm below the knee gap with preservation of the nutritive artery (a. nutricium) of the tibia, leaving a short anterior (4-5 cm) and posterior, long flap (15-17 cm).The anterior and posterior skin-fascial flaps are formed, while the posterior flap is almost three times larger than the anterior flap and includes the gastrocnemius muscle to prevent stump tension. The determination of the level of amputation was made according to the clinical picture of ischemia and the state of the peripheral arterial bed of the limb.When analyzing the results of treatment of patients with favorable immediate outcome of amputation, primary healing of a postoperative wound was considered. Suppuration of the postoperative wound with secondary healing and gangrene of the stump of the lower leg, which later leads to re-amputation at the level of the thigh, and we also attributed death to adverse results of amputation.
3. Results and Discussion
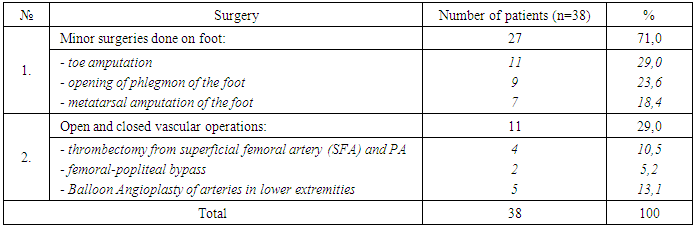
- As a result of the analysis, it was revealed that 38 (70.3%) patients out of 54 before entering our department underwent various surgical interventions.On admission to a history of 27 patients (50%), minor surgical interventions were performed on the foot and in 11 (20.3%) patients various vascular operations were performed on the limb arteries due to occlusive stenotic lesions. The revascularization of the lower limb arteries was performed in 5 (9.2%) cases (including one patient performed in our clinic).
|
 | Figure 1. The local status of the patient and the level of amputation of the leg |
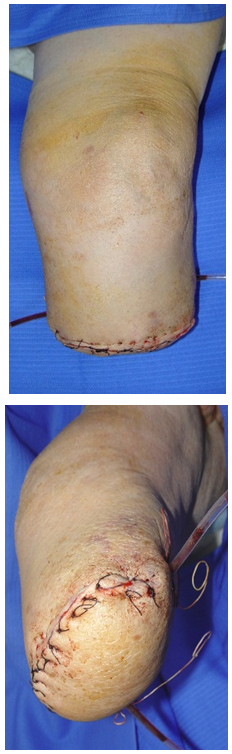 | Figure 2. Postoperative lower leg stump |
 | Figure 3. The appearance of the stump (after 18 days) |
|
4. Discussion
- Analysis of the results of treatment of patients with diabetic gangrene of the limb showed that with the correct determination of the level of amputation of the lower extremities in 85.2% of cases it is possible to ensure a smooth postoperative course, with primary wound healing. These results were achieved due to the correct selection of the level of amputation of the lower leg according to the original method developed by us. The resection of the tibia without damaging the feeding artery made it possible to preserve the functional state of the knee joint even with the development of purulent complications in the wound area in 7 cases out of 8. Amputation of the lower leg according to this technique, we were able to save the knee joint in 98.2% of cases.Adequately select the level of amputation, in our opinion, is possible only by conducting a comprehensive examination of the patient, taking into account a number of objective data. In determining the level of amputation, one should take into account the general condition of the patient, the degree of endogenous intoxication, and the data of the examination of the limb.The question of the need for limb amputation in patients with diabetic gangrene should be resolved only after assessing the possibility of a reconstructive vascular operation, the successful implementation of which reduces the level of amputation. In preparation for the amputation of the lower leg, it is important to pay special attention to the correction of the rheological and coagulation properties of the blood, the normalization of the functional state of the heart, as well as specialized psychotherapeutic training for timely and adequate psychological adaptation of the patient.
Findings
- 1. Performing amputation of the lower leg in patients with DLLG using the original method proposed by us (RUz patent #IAP 20180251 of 06/06/2018), allows preserving the knee joint in 98.2% of cases. 85.2% of patients had a smooth postoperative course.2. Anatomically substantiated resection of the bones of the tibia with the preservation of the supplying artery to allow the rapid emergence of primary callus in the stump and reduce the time of inpatient treatment of patients with lower extremity gangrene on the background of diabetes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML