Zufarov Mirjamol Mirumarovich, Mahkamov Najmiddin Kozimovich
Republican Specialized Scientific and Practical Medical Center of Surgery named after academician V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article discusses the possibilities of endovascular intervention in treatment of multifocal atherosclerotic lesions. The experience of intervention treatment of 75 patients with multifocal lesions of the coronary and carotid arteries has been presented. The technical aspects of carotid stenting have been considered. The issues of staged implementation of interventional and surgical interventions for multifocal atherosclerosis were also discussed. It has been noted that various combinations of myocardial revascularization techniques (coronary artery bypass grafting, endovascular interventions) and carotid artery stenting allow to develop a personal approach to each patient.
Keywords:
Multifocal lesion, Atherosclerosis, Myocardial revascularization
Cite this paper: Zufarov Mirjamol Mirumarovich, Mahkamov Najmiddin Kozimovich, Endovascular Intervention in Patients with Multifocal Atherosclerotic Carotid and Coronary Artery Disease, American Journal of Medicine and Medical Sciences, Vol. 9 No. 7, 2019, pp. 229-235. doi: 10.5923/j.ajmms.20190907.02.
1. Introduction
The World Health Organization (WHO) has identified cardiovascular diseases as the main cause of premature mortality in our planet. In 2016 17.9 million people died from cardiovascular diseases and it amounted 31% of all deaths in the world. 85% of these deaths occurred as a result of a ischemic heart disease and stroke [3-5, 16].In recent decades, in spite of advances in the prevention and treatment of cardiovascular diseases (CVD), they largely determine the high level of disability and remain the leading cause of death [3, 8, 12, 38]. The main cause of cardiovascular disease (CVD) in the modern world is vascular atherosclerosis and one of its main characteristics is a multifocal lesion. Multifocal atherosclerosis (MFA) being a systemic disease can affect any part of the vascular basin. The most frequent localization of atherosclerotic plaque at MFA is observed in the vessels of the coronary, extra-and intracranial basin, lower limb arteries and renal arteries. In ischemic heart disease (IHD), the frequency of combined lesions of various arterial basins can reach 70-80%. Most of all, there is a combination of lesions of the coronary and extracranial vessels - the carotid arteries [11, 23]. The clinical course of patients with vascular lesions of the coronary and carotid basins have their own characteristics and sometimes make it difficult to determine the optimal tactics and treatment method. [32, 36].The clinical course of the disease in this category of patients is manifested in the form of IHD and chronic cerebrovascular insufficiency. However, it primarily depends on the degree of narrowing and localization of the affected area of blood vessels. [32, 35]. Accordingly, the definition of a particular type of intervention stages in the diagnostics and choice of treatment method is coming to the fore.In recent years, thanks to the widespread introduction of modern diagnostic methods into clinical practice (echocardiography, CT of the coronary arteries, extra- and intracranial basin vessels) it has become possible to improve the tactics and treatment methods of patients with coronary heart disease (CHD) in combination with cranial vessels lesions [41]. Currently, the reports about the role of optical coherent tomography (OCT) in the choice of intervention for coronary artery lesions and evaluation the results of intervention have appeared in the literature [28, 29, 45].The progress of endovascular intervention field in recent years makes it possible to widely apply this method in such type of patients and leads to an improvement of immediate and long-term results. However, there are a number of unresolved issues in the diagnostics and treatment of patients with coronary artery disease in combination with the carotid arteries lesions. All mentioned above dictates further research to optimize treatment tactics and improve its results in such patients.
2. Material and Methods
The study was conducted in 75 patients with combined coronary and carotid artery disease in the department of endovascular surgery and cardiac arrhythmias’ of the Republican Specialized Scientific and Practical Medical Center of Surgery from 2012 to 2017. The age of patients ranged from 56 to 80 years (mean age 58.2 ± 1.2 years). All patients underwent a comprehensive examination approved for diagnostics of patients with combined disease of coronary and carotid arteries (ECG, Echo, US Doppler of carotid arteries) including consultations of a vascular surgeon, a cardiac surgeon, a neurologist and an endocrinologist if necessary. Depending on the treatment, the patients were divided into the following groups:Group I (35 patients) - patients who underwent percutaneous coronary intervention (PCI) and carotid artery stenting (CAS), from them 2 patients underwent in one-stage intervention - PCI and CAS. In the remaining 33 patients the first stage was PCI and after 2 days - CAS.Group II (24 patients) –for all patients in first stage CAS was done and then for second stage coronary artery bypass surgery (CABG) were recommended. This tactic was chosen because of high intraoperative risk of stroke development in CABG.Group III (16 patients) –for the first stage CAS was done and for coronary disease the optimal medical therapy (OMT) were recommended, because of this group included patients with not significant coronary artery stenosis.
3. Results
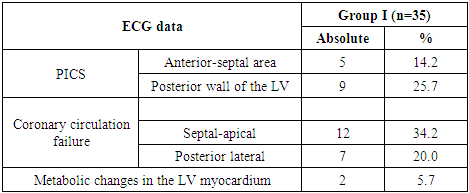
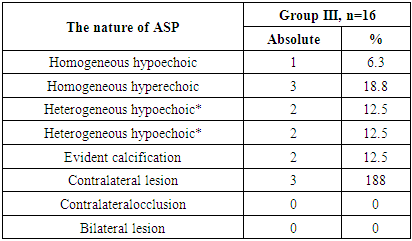
The analysis of the examination results and performed endovascular intervention in 75 patients was carried out.In group I (n = 35) the symptoms of CHD of various degrees prevailed in the clinical course of the disease. Unstable angina was detected in 7 (20.0%) patients, 9 (25.7%) cases belonged to Grade IV, by Canadian Cardiovascular Society (CCS), and 19 (54.2%) –to Grade III. All patients in this group were found to have significant stenosis of the internal carotid artery (ICA) of varying degrees. At the same time, in 16 (45.7%) they were of symptomatic and in 19 (54.2%) – of asymptomatic course.Also during the history taking we determined the risk factors for cardiovascular diseases (CVD) and concomitant diseases development. Thus, dyslipidemia was noted in 14 (40.0%) patients, hypertension in 24 (68.5%), in 7 (20.0%) - diabetes mellitus (DM) of type II, 17 (48.5%) patients had a hereditary history, in 16 (45.7) - a chronic disorder of cerebral circulation (CDCC), and 4 (11.4%) had a bad habit (smoking). Patients were also distributed according to old diseases: 17 (48.5%) patients had a history of post-infarction cardiosclerosis (PICS), 1 (2.8%) had a condition after CABG surgery, 1 (2.8%) – transient ischemic attack (TIA) and in 1 (2.8%) – acute stroke (AS) At the same time, in group I (n = 35) according to ECG data, in 5 (14.2%) patients PICS was detected in the anterior-septal area of the left ventricle (LV), and in the posterior wall of the LV - in 9 (25.7%) patients. The coronary circulation failure with the signs of ischemia in the septal-apical in 12 (34.2%) and in the posterior lateral LV area in 7 (20.0%) patients were revealed. The presence of metabolic changes in the LV myocardium was observed in 2 (5.7%) patients (Table 1).Table 1. Characteristics of ECG data in Group I (n = 35)
 |
| |
|
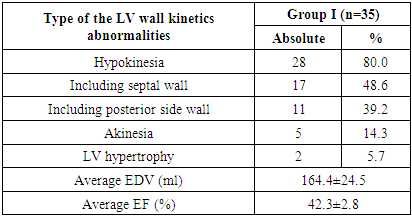
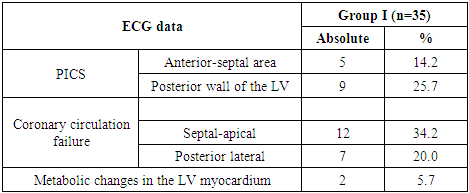
According to Echo data in this group, the LV hypokinesia zone was observed in 28 (80.0%) patients, in 17 (48.6%) among them in the area of the septal wall, in 11 (39.2%) cases - in the posterior side wall. Akinesia was detected in 5 (14.3%) patients and in 2 (5.7%) cases - LV hypertrophy. Comparative data of the end-diastolic volume (EDV) of the LV revealed their significant increase (164.4 ± 24.5 ml on average), while the indicators of the ejection fraction (EF) were lower (42.3 ± 2.8%) (Table 2).Table 2. Characteristics of echocardiographic data in Group I (n = 35)
 |
| |
|
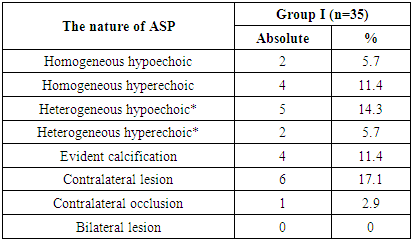
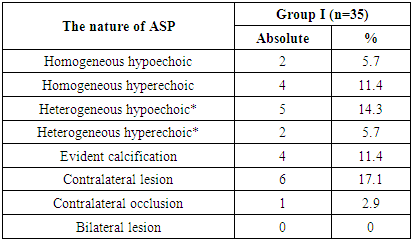
Ultrasound dopplerography investigations of the brachiocephalic arteries with duplexs canning in the first group patients revealed atherosclerotic plaques (ASP) of various nature with the presence of calcification: homogeneous hypoechoic ASP - in 2 patients, homogeneous hyperechoic - in 4, and in 5 – heterogeneous hypoechoic. Heterogeneous type was revealed in 7 patients, in 5 of them - hypoechoic type and in 2 - hyperechoic type. An evident calcification was observed in 4 patients. In 6 patients of this group a contralateral lesion disease of the carotid artery (CA) was noted, while a contralateral occlusion was noted in 1 patient.Based on the above data, 33 (44.0%) patients were underwent phased endovascular intervention in both basins of the arterial bed, in 24 (72.7%) of them PCI was performed by the first stage and the CAS - by the second stage. In 9 (27.2%) patients the first stage was САS, the second stage was PCI. This management tactics was chosen because of pronounced angina clinic. The angina clinic prevailed in this group: PCI as the first stage was performed at unstable angina and Grade IV and III by CCS. CAS as the first stages was performed in cases of CDCC evident symptoms prevailing over the manifestations of angina clinic. In 2 (2.6%) patients intervention was performed on the coronary and carotid arteries in one-stage: one patient (1.3%) intervention of carotid and carotid artery was done through radial approach and the second one (1.3%) - through femoral approach. The basis for a one-stage intervention was a local isolated coronary artery stenosis with a concomitant significant carotid stenosis.Table 3. Ultrasound characteristics of the carotid arteries and ASP in Group I (n = 35)
 |
| |
|
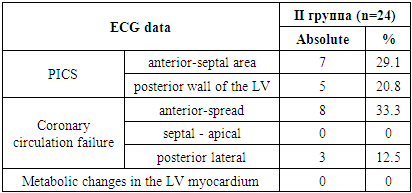
In group II (n = 24), the symptoms of CDCC prevailed in the clinical course of the disease. 20 (83.3%) of them had a symptomatic course and 4 (16.6%) – asymptomatic one. The patients in this group were also divided according to the clinical course of CHD: 5 (28.8%) patients belonged to Grade IV and 19 (79.1%) – to Grade IIIby CCS.Also during the history taking we determined the risk factors for cardiovascular diseases (CVD) and concomitant diseases development. Thus, dyslipidemia was noted in 8 (33.3%) patients, hypertension in 19 (79.1%), 10 (41.6%) had diabetes mellitus of type II, 12 (50.0%) patients had a hereditary history and 8 (33.3%) had a bad habit (smoking). Patients were also distributed according to old diseases: 9 (37.5%) patients had a history of post-infarction cardiosclerosis (PICS), in 2 (8.3%) cases – condition after carotid endarterectomy (CEA), and in 1 (4.1%) – TIA.Comprehensive investigations of the second group (n = 24) revealed: according to ECG data PICS was detected in 7 (29,1%) cases in anterior-septal area of the left ventricle (LV), and in 5 с (20,8%) patients -in the posterior wall of the LV. Signs of myocardial ischemia were observed in 8 patients (33.3%) - anterior-widespread and in 3 patients (12.5%) in the posterior lateral area of LV (Table 4).Table 4. Characteristics of ECG data in Group II (n=24)
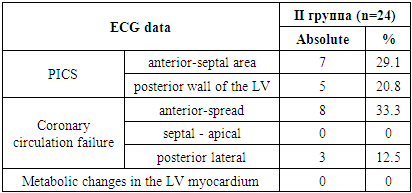 |
| |
|
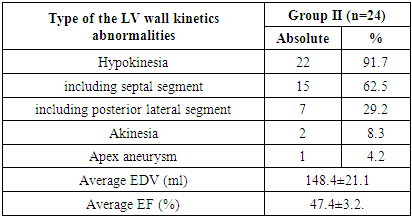
According to Echo data in this group, the LV hypokinesia zone was observed in 22 (91.7%) patients, in 15 (62.5%) of them – in the septal area and in 7 (29.2%) – in posterior lateral area. Akinesia was detected in 2 (8.3%) patients, in 1 (4.2%) among them the presence of LV apex aneurysm was found. The EDV data of the LV revealed an increase of 154.3 ± 22.4 ml on average, while the EF indicators were lower and made up 47.4 ± 3.2% (Table 5).Table 5. Characteristics of echocardiographic data in Group II (n=24)
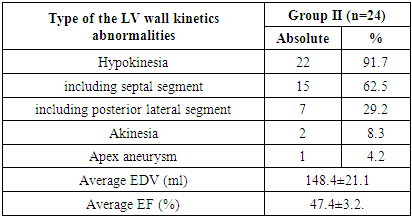 |
| |
|
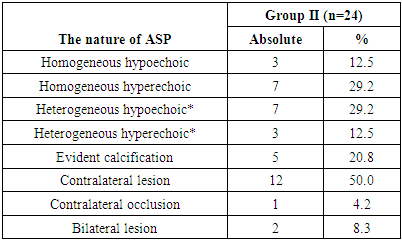
Ultrasound dopplerography investigations of carotid arteries revealed atherosclerotic plaques (ASP) of various nature with the presence of calcification: homogeneous hypoechoic ASP in 3 patients, homogeneous hyperechoic in 7 patients. In 10 patients a heterogeneous type was revealed: in 7 of them - the hypoechoic type and in 3 - hyperechoic type. An evident calcification was observed in 5 patients. In 12 patients of this group there was a lesion on the opposite side, while a contralateral occlusion was observed in 1 patient (Table 6).Table 6. Ultrasound characteristics of the carotid arteries and ASP in Group II (n=24)
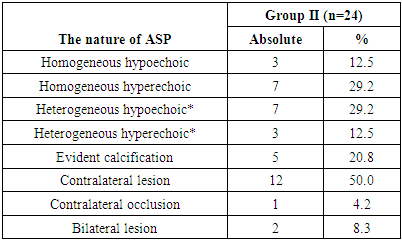 |
| |
|
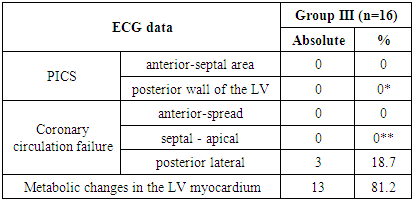
Thus, all patients in this group were performed endovascular intervention as the first stage, CAS with following CABG. This tactic was considered with a high intraoperative risk of stroke development due to the presence of carotid artery severe stenosis and the presence of a multivessel coronary disease that required CABG.In group III (n=16) the symptoms of CDCC prevailed in the clinical course of the disease. All patients had a symptomatic course of the disease. Also during the history taking, we determined the risk factors for cardiovascular diseases (CVD) and concomitant diseases development. Thus, dyslipidemia was noted in 5 (31,2%) patients, hypertension– in 13 (81,2%), 5 (31,2%) patients had a hereditary history and 2(12,5%) patients had a bad habit (smoking). Patients were also distributed according to old diseases: in 2 (12,5%) patients TIA was in the anamnesis, in 3 (18,7%) cases – condition after carotid endarterectomy (CEA).The investigation of ECG data in the third group (n = 16) showed less significant changes: in 3 cases (18.7%) myocardial coronary circulation was insufficient in the LV posterior lateral area, and in 13 (81.2%) cases - metabolic changes in the myocardium (Table 7).Table 7. Characteristics of echocardiographic data in Group III (n=16)
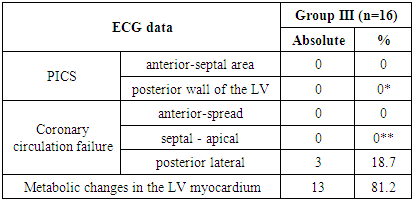 |
| |
|
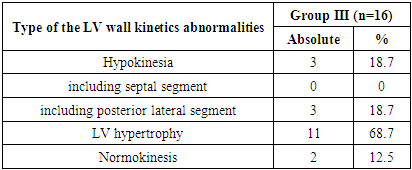
Echo study showed signs of hypokinesia in 14 patients: in the posterior-lateral wall of the left ventricle – in 3 (18.7%) patients; in 2 (12.5%) patients normokinesis was detected; LV hypertrophy was detected in 11 (68.7%) patients (Table 8).Table 8. Characteristics of echocardiographic data in Group (n=16)
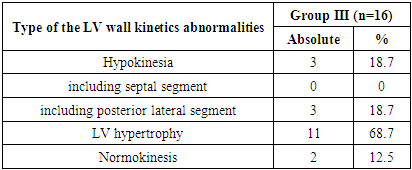 |
| |
|
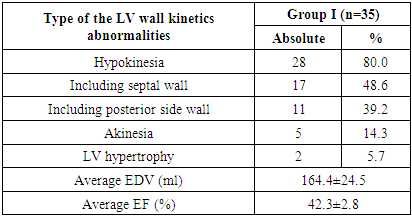
Ultrasounddopplerographyinvestigationsofcarotidarteriesrevealedatheroscleroticplaques (ASP) of variousnature: homogeneous was revealed in 4 cases – with hypoechoic type in 1 patient and hyperechoic – in 3 patients. Heterogeneous type was revealed in 4 patients: 2 patients had hypoechoic and 2 – hyperechoic types. An evident calcification was observed in 2 patients. There was a lesion on the opposite side in 3 patients of this group, occlusion and bilateral lesion were not detected (Table 9).Table 9. Ultrasound characteristics of the carotid arteries and ASP in Group III (n=16)
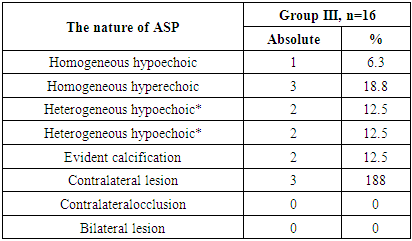 |
| |
|
We also checked the CT- angiography of the coronary arteries in 27 patients. In 16 (59.2%) patients from examined by CT-angiography no significant coronary artery lesions were detected. They were recommended further observation and treatment by a cardiologist.There was a uniform type of coronary blood supply in 11 (40.7%) patients with CT-angiography, less frequent - right and left types. In 17 (63.2%) patients the structure of the coronary bed was normal, in 10 (36.7%) patients such variants of its structure as trifurcation of the left coronary artery trunk, short trunk of the left coronary artery, hypoplasia of the right coronary and circumflex arteries were revealed.At CT-angiography atherosclerotic plaques that do not cause hemodynamically significant narrowing were detected in 16 (32.6%) patients in 28 arteries, in 17 segments. They were located more often in the proximal (50%) and medial (28.9%), less often in the distal (6.3%) segments and in the lateral branches (10.5%). Hemodynamically significant stenosis were found in 11 (40.7%) patients in 32 arteries, 48 segments: 46.8%, of themweremedial, proximal - 29.8%, distal - 6.4%, lateral branches - 10.6 %. In group III (n = 16) only intervention on the carotid artery was performed with following medical treatment for CHD: it was connected with a hemodynamically insignificant coronary artery lesion confirmed by CT-coronarography. The preoperative preparation of patients included the administration of medicines. Moreover, when endovascular intervetion on the carotid arteries was planned, dual antiplatelet therapy (DAPT) (clopidogrel 75mg / day; aspirin 75-150mg / day) started 4 days before the intervention. But to date there is no clear indication for the use of the clopidogrel preoperative dose at CAS in the recommendations. It should be also noted that for all patients who underwent percutaneous intervention (PCI), the pre-operative dose of clopidogrel was 600 mg, aspirin - 300 mg, according to the recommendations of ESC and AHA / ACC. In addition, all patients received basic medical therapy for CHD and concomitant diseases.In group I (n = 35), according to coronary angiography, in 2 (5.7%) patients single-vessel, in 21 (60.0%) - two-vessel and in 12 (34.2%) cases - three-vessel lesions of coronary artery were revealed. Coronary angiography data were also distributed according to the nature of the lesion: bifurcation, chronic occlusion, stenosis of the left coronary artery (LCA) and isolated. Coronary angiography data was assessed using the Syntax score to determine the optimal recommendation for the patient in choosing the method of operation (PCI or CABG). According to this scale, in 7 patients the SYNTAX Score was low risk - 18, in 23 patients - the average risk (SYNTAX Score = 28) and in 5 patients - the high risk (SYNTAX Score> 32 points). In 33 (44.0%) of all patients, step-by-step endovascular intervention was performed: in 24 (72.7%) of them the first stage was PCI and in 9 (27.2%) patients the first stage was СAS. In 2 (2.6%) patients one-stage intervention was performed on the coronary and carotid arteries. In 1 (1.3%) of those patient PCI + CAS was performed through radial approach. The choice of this approach to perform Intervention was the abnormal discharge of the left common carotid artery from the innominate artery. In the first group 36 CAS were performed in 35 patients, in one of them - on both sides. In all cases self-expanding stents were used: ProtégéTMRX (EV3); Acculink (Abbot); Xact (Abbot); Mer (Balton) - flask-shaped, tapered and straight. In 19 (54.2%) patients CAS was performed in the left internal carotid artery (ICA) and in 16 (45.7%) CAS was performed on the right. All patients with CCA were used distal protective devices (neuroprotective system) of various types. In 31 (86.1%) patients the neuroprotective system “Robin” was used and in 5 (13.8%) patients - “NAV6”. In 2 (5.7%) cases, due to the critical narrowing before embedding the device of protection against embolism, pre-dilatation of the bifurcation of the carotid artery by the coronary balloon NC Trek - 2.0 mm “Abbot” was performed. Before the installation of the defense system all patients were introduced atropine intravenously — 0.1% -1.0 mg, heparin 1000 U / kg. And also activated blood clotting time (ACT) was determined reaching a target level of more than 250-300 seconds. In 3 (8.5%) of all 35 patients stents of “straight” form were used, in 6 (17.1%) - cone-shaped ones and in26 (74.2%) flask-shaped stents were used. In 32 (91.4%) cases after implantation of the stent post-dilatation was performed with a coronary balloon 4.0-5.0mm. The indication for post-dilatation was the presence of residual stenosis> 30%.In group II (n = 24), CAS was performed in 24 patients. In all cases self-expanding stents were used: ProtégéTMRX (EV3); Acculink (Abbot); Xact (Abbot); Mer (Balton) - flask-shaped, tapered and straight. In 7 (29.1%) of them CCA was performed in the left internal carotid artery (ICA) and in 17 (70.8%) cases - on the right.All patients with CAS were used distal protective devices (neuroprotective system) of various types. In 21 (87.5%) patients the neuroprotective system “Robin” (Balton) was used, in 2 (8.3%) patients - “NAV6” (Abbot), and in 1 (4.1%) - “Filter Wire EZ (Boston Scientific). Before the installation of the defense system all patients were administered intravenous atropine — 0.1% -1.0 mg, heparin 1000 U / kg. And also ACT was determined reaching a target level of more than 250-300 seconds. All 24 patients were used flask-shaped stents. In 19 (79.1%) cases after stent implantation a post-dilatation was performed with a coronary balloon 4.0-5.0mm. The indication for post-dilatation was the presence of residual stenosis > 30%. In 8 (33.3%) patients in the postoperative period hypotension was observed, which was corrected by the intravenous administration of minimal doses of dopamine (3-5 mg / kg) with a duration of up to 6 hours. A good angiographic result was obtained in all patients with CAS. Such tactics in this group was associated with a high intra-operative risk of stroke development due to the presence of evident stenosis of carotid artery and the presence of a multivessle disease of coronary artery.In group III (n = 16), the CAS was also successfully performed in all patients. The clinical manifestation of angina pectoris in this group was assessed as Grade I-II by CCS, which was confirmed by CT-angiography of the coronary arteries, and OMT for CHD and observation by a cardiologist at the place of residence was recommended for all patients in this group.
4. Discussion
There are currently several studies comparing the results of stenting and endarterectomy from the internal carotid arteries. The most important is the study “Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy SAPPHIRE” comparing the results of these interventions in patients with high surgical risk [17]. As it has been shown in this work, 30 days after surgery the combined frequency of death, stroke and myocardial infarction was 5.8% at stenting and 12.6% at endarterectomy. After 1 year the same indicator was 11.9% at stenting and 19.9% at endarterectomy; in 2 years - 20.1% and 26.7%, respectively. When analyzing a group of patients with diabetes, the frequency of stroke within 30 days after the intervention was 2.4% for stenting and 6.8% for endarterectomy. A year later the incidence of stroke in this group was 4.8% and 25%, respectively. The main factors that increase the risk of carotid endarterectomy include: occlusion of the contralateral carotid artery, previously performed homolateral carotid endarterectomy, as well as combined lesion of the carotid and coronary arteries [15]. Considering the severe clinical condition of patients with multifocal atherosclerosis, as well as a large percentage of complications arising at the early hospital stage after performing open surgery, mini-invasive low-impact endovascular interventions are now increasingly used to treat these type of patients [1, 13]. Nevertheless, there are still many unresolved questions regarding the criteria for selecting patients for a particular treatment method, the volume of operations and their effectiveness. All this requires joint decisions of cardiologists, neurologists, vascular and X-ray endovascular surgeons. This paper presents our relatively small experience of endovascular intervention in patients with a combined lesion of the coronary and carotid basin. All carotid stentings in our hospital were performed using brain protection devices. It should be noted that the use of protective filters is not an absolute guarantee for the prevention of possible neurological complications. However, the effectiveness of these devices has been proved, and their application is obligatory. According to the literary data when stenting with the use of protective devices, the frequency of neurological complications is reduced by 60% [9] and the frequency of echo signals from microemboli that have come off during the procedure decreases from 28.5% to 8.2% [7]. In some cases, a filter held in the distal parts of ICA can provoke an evident spasm of artery. Stenting of the carotid arteries has recently become a real alternative to carotid endarterectomy, especially in patients with severe carotid stenosis in combination with concomitant diseases, i.e. in patients with high surgical risk [16]. A very significant case is the case of stenting of ICA and coronary artery in a patient with occlusion of the contralateral ICA. In such patients the endovascular method is the safest, and in some cases the only possible method to save the patient from the illness or to prepare him for surgical treatment. Various combinations of myocardial revasculization techniques (coronary artery bypass grafting, endovascular interventions) and carotid artery stenting make it possible to develop a personal approach to each patient. However, large randomized studies are needed in order to determine finally the role of carotid stenting in the treatment of patients with combined lesions of the coronary and carotid arteries.
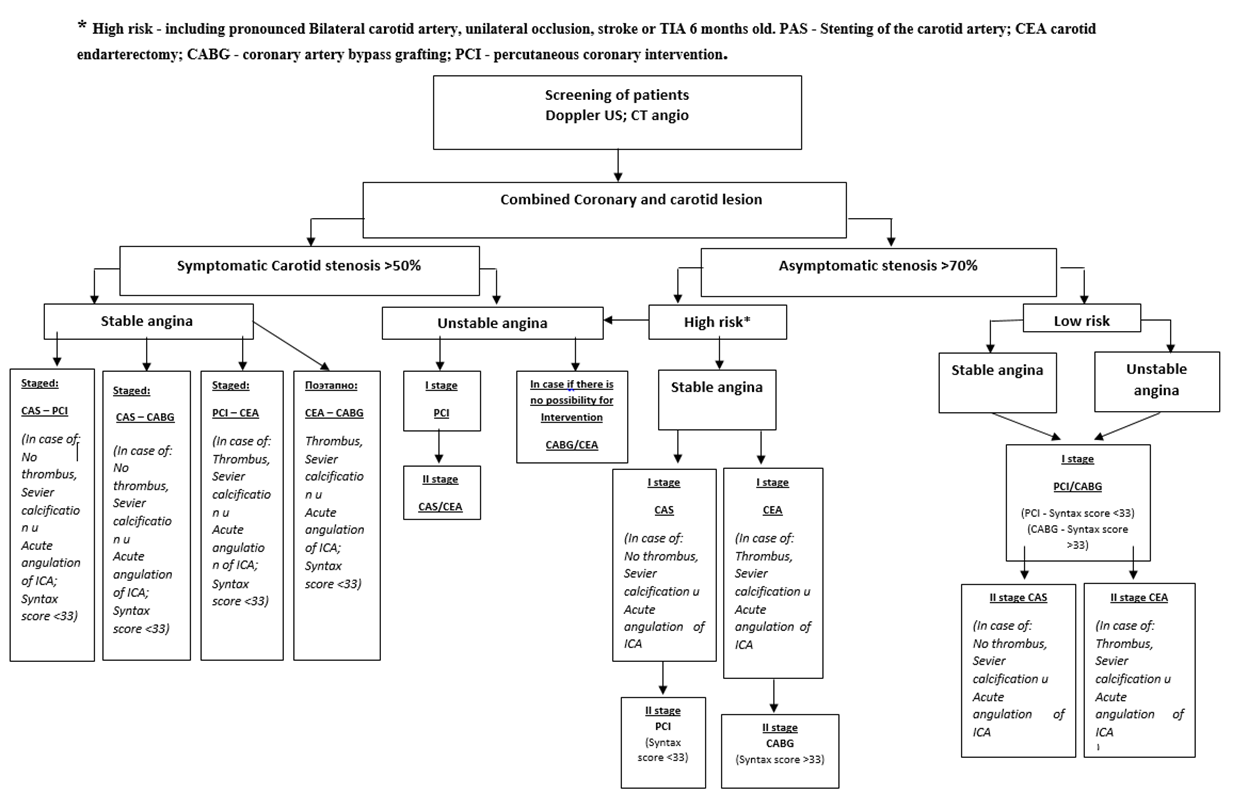
5. Conclusions
We developed the algorithm for choosing the correct and optimal tactics for patients with combined diseases of coronary and carotid arteries based on our study. Nowadays the results of CAS are comparable with the results of CEA, because it can be the alternative treatment method in patients with high surgical risk. The use of endovascular intervention allows to reduce the volume of surgical intervention and has a great importance for such severe group of patients.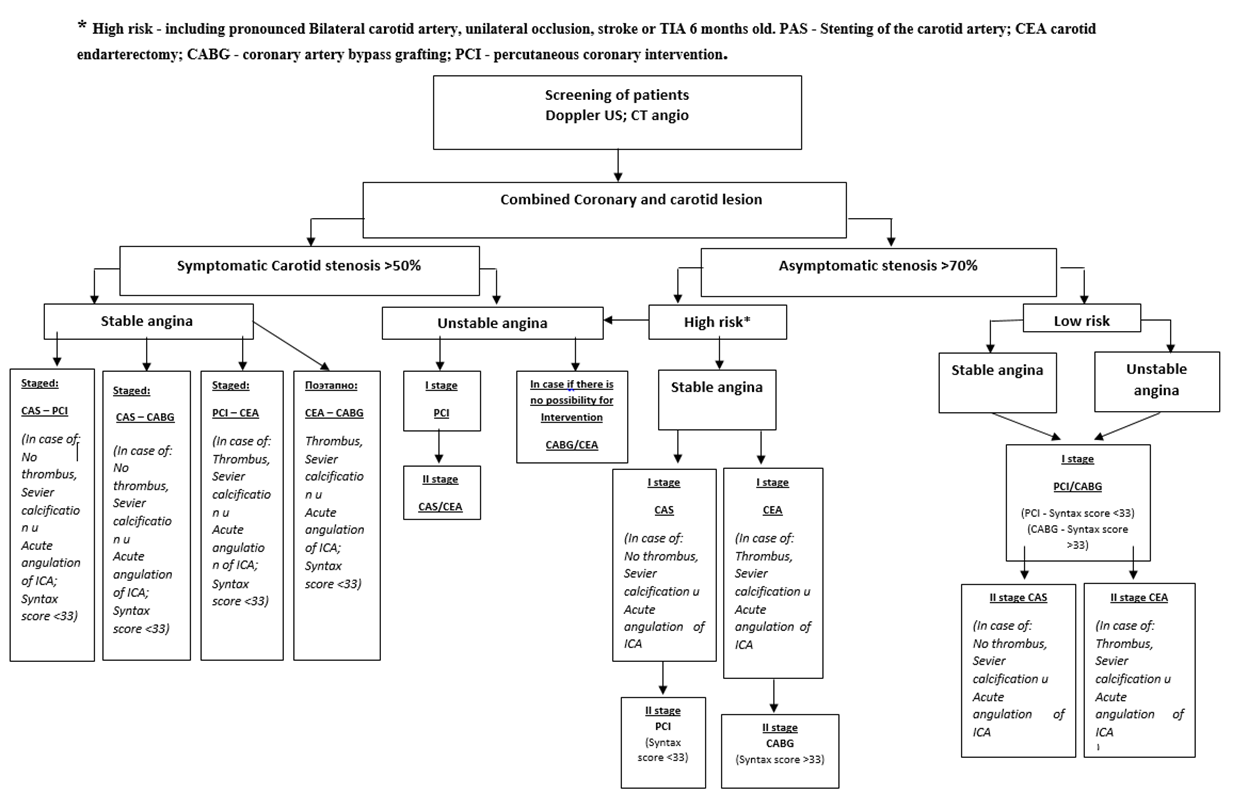 | Figure |
References
| [1] | Bockeria L.A, Alekyan B.G., Mironov N.P. Endovascular surgery in the treatment of patients with ischemic heart disease in combination with multifocal atherosclerosis: a guide to endovascular surgery of the heart and blood vessels. - M.: RSCVSnamed after A.N. Bakulev, 2008. - Volume 1. - Chapter 10. - P.132-148. |
| [2] | Bockeria LA, Gudkova R.G. Diseases and congenital anomalies of the circulatory system // Cardiovascular Surgery - 2007. - №1. - P. 25-29. |
| [3] | Bockeria L.A, Alekyan B.G., Ter-Akopyan A.B. Possibilities of endovascular treatment of patients with CHD in combination with the pathology of the internal carotid artery // Thoracic and cardiovascular surgery. - 2006. - № 6. - P.51 - 56. |
| [4] | Pokrovsky A.V. Prevention of ischemic stroke: surgery of the main arteries of the head // The works of the I National Congress “Cardioneurology”. - 2008. - P. 27-30. |
| [5] | Safiullina L.R., Akberov R.F., Sharafeev A.Z. Ultrasonic technologies in the diagnosis of multifocal atherosclerosis: a training manual. - Kazan: Printing house, 2008. –P.30. |
| [6] | Todurov B.M., A.V. Khokhlov, A.A. Maksakov, Khorram Sohrab, M.V. Shimanko. Absorbable stents: a new era in interventional cardiology. Heart surgery and interventional cardiology. 2013. №1, P.23-26. |
| [7] | Alcock R.F. Incidence and determinants of myocardial infarction following percutaneous coronary interventions according to the revised Joint Task Force definition of troponin T elevation / R.F. Alcock, P. Roy, K. Adorini et al. // Int J Cardiol. - № 2010. - № 140. - P.66-72. |
| [8] | Chieffo A. 5-Year outcomes following percutaneous coronary intervention with drug-eluting stent implantation versus coronary artery bypass graft for unprotected left main coronary artery lesions: the Milan experience / A. Chieffo, V. Magni, A. Latib et al.// JACC Cardiovasc Interv. – 2010. - №3. - P.595-601. |
| [9] | Damgaard S. One-year results of total arterial revascularization vs. conventional coronary surgery: CARRPO trial / S. Damgaard, J. Wetterslev, J.T. Lund et al. // Eur. Heart. J. - 2009. - V.30, №8. - P. 1005-1011. |
| [10] | Freitag G., Freitag J., Koch R. Percutaneous angioplasty of carotid artery stenoses // Neuroradiology.-1986.-Vol. 28, №2.-P. 126-127. |
| [11] | Lopes D.K., Mericle R.A., Lanzino G. Stent placement for the treatment of occlusive atherosclerotic carotid artery disease in patients with concomitant coronary artery disease. // J Neurosurg. – 2002. – vol.96. – P.490-496. |
| [12] | Mathias K., Jaeger M. How much Cerebral Embolization Occurs during C.A.S.? // International Symposium on Endovascular Therapy meeting. –Miami, 2001. – P 348. |
| [13] | Norris J., Bornstein N. Vascular risk of assimptomatic carotid stenosis // Stroke, 1991. – vol. 22. – P.1485-1490. |
| [14] | Ogilvy C.S. Restenosis rates following vertebral artery origin stenting: does stent type make a difference? / C.S Ogilvy, X. Yang, S.K. Natarajan et al //J Invasive Cardiol. - 2010. - V.22, №3. - P. 119-1124. |
| [15] | Onuma Y. Long-term clinical results following stenting of the left main stem: insights from RESEARCH (Rapamycin-Eluting Stent Evaluated at Rotter- dam Cardiology Hospital) and T-SEARCH (Taxus-Stent Evaluated at Rotterdam Cardiology Hospital) registries / Y. Onuma, C. Girasis, N. Piazza et al. // JACC Cardiovasc Interv. - 2010, - №. - P.5 84-594. |
| [16] | Schofer J. New Focal Ischemia of Brain After Carotid Artery Stenting Despite Distal Protection. – JACC, 2002. – vol.39 (suppl A). - P. 67A. |
| [17] | Yadav J. S., Wholey M. H., Kuntz R. E.Protected Carotid-Artery Stenting versus Endarterectomy in High-Risk Patients. // N Engl J Med. – 2004. – vol.351:1493-1501. |
| [18] | Yadav J.S., Wholey M. H., Kuntz R. E., et al. Protected Carotid-Artery Stenting versus Endarterectomy in High-Risk Patients. // N Engl J Med. - 2004; 351:1493-1501. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML