-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(6): 210-212
doi:10.5923/j.ajmms.20190906.07

The Role of Reproductive Surgery in Diagnostics and Treatment of Combined Pathologies in Women with Infertility Caused by Benign Structural Changes of Ovaries
Shukurov Farkhad Ishkulovich1, Ayupova Farida Mirzaevna2
1Tashkent Medical Academy, Tashkent, Uzbekistan
2Department of Obstetrics and Gynecology No.1
Correspondence to: Shukurov Farkhad Ishkulovich, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim of the study: to assess the role and effectiveness of reproductive surgery in the diagnosis and treatment of combined pathologies in women with infertility caused by benign ovarian structural changes. Methods: All patients underwent a comprehensive examination, which included clinical, laboratory, hormonal, transvaginal ultrasound scanning, hysterosalpingography, laparoscopy, hysteroscopy, and a prospective study. Results: During laparoscopy in patients with infertility, various combined pathologies of the fallopian tubes were revealed: in 24 (10%) adhesions in the area of fimbria, in 6 (2.5%) obstruction of the fallopian tube in the ampullary section was determined. In 3 patients (1.25%) the adhesive process of grade II – III was determined. During hysteroscopic examination, 26 (10.8%) women had an intrauterine pathology: endometrial polyp – in 11 (4.6%), synechia in the uterus – in 5 (2.1%), endometrial hyperplastic processes – in 4 (1.6%), ligatures in the uterus after a cesarean section – in 6 (2.5%). Correction of concomitant gynecological pathology was carried out: restoration of the anatomical ratios of the pelvic organs (adhesiolysis, salpingovario - and fimbriolysis, salpingostomy) and if patients had concomitant intrauterine pathology, hysteroscopic correction was performed. Uterine pregnancy occurred in 210 women (87.5%) and the menstrual function was restored in 79.6% of patients. Conclusion: The use of reproductive surgery in women with infertility caused by benign structural changes in the ovaries, allows you to identify and eliminate all existing comorbidities, including the causes of uterine infertility, and increase the frequency of pregnancy in 87.5% of women.
Keywords: Infertility, Combined pathology, Laparoscopy, Hysteroscopy
Cite this paper: Shukurov Farkhad Ishkulovich, Ayupova Farida Mirzaevna, The Role of Reproductive Surgery in Diagnostics and Treatment of Combined Pathologies in Women with Infertility Caused by Benign Structural Changes of Ovaries, American Journal of Medicine and Medical Sciences, Vol. 9 No. 6, 2019, pp. 210-212. doi: 10.5923/j.ajmms.20190906.07.
1. Introduction
- One of the areas of infertility treatment is the use of minimally invasive surgery, the frequency of pregnancy after which ranges from 21% to 30% [1-3]. The diagnostic value of reproductive surgery in identifying the causes of reproductive disorders in women is extremely high and reaches 97.6% [4-6]. The effectiveness of surgical treatment of women of reproductive age with various gynecological pathologies significantly increased after the introduction of new technologies in clinical practice using reproductive surgery [7, 8]. However, there remain debatable questions about the use of certain technical methods of surgery, various surgical approaches, new technical means, in the diagnosis and treatment of combined pathologies in women with infertility caused by benign ovarian structural changes [9, 10]. In connection with the discussion that has arisen, the clarification of the role of reproductive surgery in the diagnosis and treatment of combined pathologies in women with infertility has become very relevant, due to benign structural changes in the ovaries in modern conditions.Aim of the study was to assess the role and effectiveness of reproductive surgery in the diagnosis and treatment of combined pathologies of women with infertility caused by benign ovarian structural changes.
2. Material and Methods
- A total of 270 patients with infertility due to benign ovarian structural changes were examined. The main group consisted of: 120 women with polycystic ovary syndrome and 120 women with follicular ovarian cysts, the comparison group – 30 healthy women. The age of patients ranged from 24 to 34 years. The average age of patients was 28.2±0.5 years. Primary infertility suffered 156 (57.7%), the secondary – 114 (42.3%) patients. The duration of infertility was from 1 to 6 years. In order to clarify the cause of infertility, all patients underwent a comprehensive examination, which included clinical, laboratory, hormonal, microbiological studies, transvaginal ultrasound scanning, hysterosalpinography, laparoscopy, hysteroscopy and a prospective study. Diagnosis and treatment of patients with infertility was carried out by two methods of reproductive surgery: laparoscopic and hysteroscopic. Laparoscopic and hysteroscopic operations were performed using «Karl Storz» equipment. Depending on the operative method used, the patients were divided into 2 groups: all 240 patients underwent surgery on the ovaries in a laparoscopic manner; of these, 30 patients underwent hysteroscopy about the diagnosis and treatment of intrauterine pathology. To assess the role and effectiveness of various methods of reproductive surgery, the following indicators were used: the frequency of recovery of menstrual function and the frequency of uterine pregnancy according to the survey. Ethical Aspects. The study procedure doesn't interfere with any ethical basics and oral agreement was taken to all patients.The obtained data was processed using the statistical package of software "Statistics 6.0".
3. Results and Discussion
- As a result of the survey, infertility was detected in 120 women (44.4%), caused by follicular ovarian cysts (FOC) and 120 (44.4%) – infertility associated with impaired ovulation - polycystic ovary syndrome (PCOS). It should be noted that in 80 (30.0%) women there was a combination of 2 to 3 factors impairing reproductive function. The volume of laparoscopic operations for follicular cysts consisted of exfoliating the capsule of the cyst – cystoectomy, and for PCOS, 2 variants of laparoscopic surgery were mainly used: electrocautery (30 patients) and partial ovarian resection (90 patients). Laparoscopic electrocautery of polycystic ovaries was performed using a monopolar needle electrode. Electrocautery of the ovaries were produced with all possible small cystic inclusions. During laparoscopy, patients with infertility caused by benign ovarian structural changes revealed various combined pathologies of the fallopian tubes: 24 (10%) had adhesions in the area of fimbria, 6 (2.5%) obstruction of the fallopian tube in the ampullary section was determined. In 3 patients (1.25%) the adhesive process was determined by II–III degrees of severity (Fig.1).
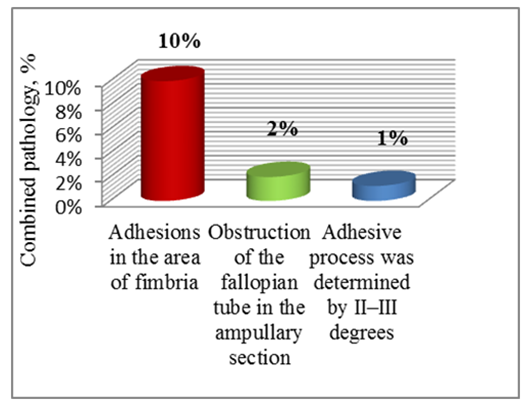 | Figure 1. Revealed combined pathology during laparoscopy in patients with benign ovarian structural changes |
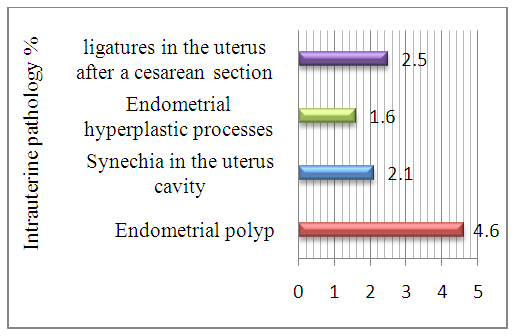 | Figure 2. The Identified types of intrauterine pathology during hysteroscopy in patients with benign ovarian structural changes |
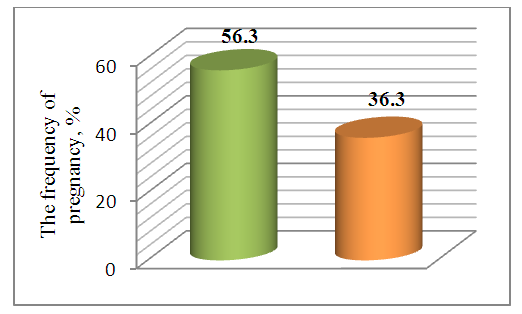 | Figure 3. The frequency of pregnancy in patients with PCOS, depending on the type of surgery on the ovaries |
4. Conclusions
- The use of reproductive surgery in women with infertility, caused by benign structural changes in the ovaries, makes it possible to identify and eliminate all the of combined pathologies existing, including the uterine causes of infertility and increases the pregnancy rate in 87.5% of women.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML