Khikmat Anvarov, Farkhod Khadjibaev
Republican Research Centre of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article provides the treatment analysis of patients with urgent surgical complications of liver parasite invasions. An analysis of the causes of the disease complications occurrence has been conducted. The use of a specialized algorithm with the wide use of minimally invasive technologies has made it possible not only to diagnose the cause of the obstruction in a timely manner, but also to provide complete and qualified assistance to patients.
Keywords:
Hepatic echinococcosis, Liver fluke, Fascioliasis, Obturation, Obstructive jaundice, Complications
Cite this paper: Khikmat Anvarov, Farkhod Khadjibaev, Surgical Management of Urgent Complications of Liver Parasite Invasions, American Journal of Medicine and Medical Sciences, Vol. 9 No. 6, 2019, pp. 197-202. doi: 10.5923/j.ajmms.20190906.05.
1. Introduction
Parasitic liver disease (PLD) is a common phenomenon caused by various types of round, flat and tape worms. In Uzbekistan, the most widespread parasitic lesion is by the larval stage of the E. granulosus chain [3-4] in which the liver most often affects (about 80%) and the right lobe is more often affected than the left one [4-5].Suppuration of hydatid cysts of the liver is the most severe and dangerous among the complications of liver echinococcosis (LE) (17-26%) and, as a rule, is followed by severe dysfunction of the liver and other vital organs [6-8]. Many important aspects of this complication occurrence mechanism are still controversial and not fully studied. The diversity of the disease clinical picture, the increase in the number of patients among urban population have led to diagnostic errors in early stages of the disease [11-12]. This, in turn, leads to an increase of the number of patients with complicated forms of LE and generally affects the treatment outcome.Another formidable complication of LE requiring urgent surgical intervention is the cyst breakthrough into the bile ducts with the development of bile ducts obturation and obstructive jaundice [2, 8], when the only treatment method for this case is surgery.Fascioliasis is a common parasitic disease caused by trematodes Fasciola hepatica L. and Fasciola gigantica genus with a primary lesion of the biliary system. Obturation of the biliary tract by adult individuals is a rare complication of this zoonosis occurring on average in 0.008-0.01% of surgical patients [11, 14]. At the same time, about 17 million people suffer from liver trematodes and about 350 million people are at risk of infection [12, 15].However, the lack of unified algorithm for diagnosis and treatment, as well as a late visit to a surgical hospital can lead to fatal consequences.
2. Material and Methods
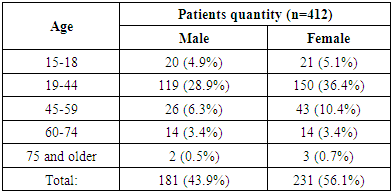
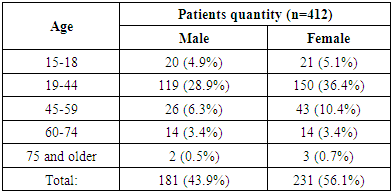
412 patients with various complications of parasitic liver diseases were observed the Republican Research Center of Emergency Medicine for the period from 2006 to March 2018. Obstruction of the biliary tract by adult forms of F. Hepatica was observed in 9 cases, complications of liver echinococcosis - in 403 cases.The age of patients ranged from 15 to 78 years (mean age was 34.4 ± 12.3 years. There were 181 men (43.9%) and 231 women (56.1%), in the ratio of 0.78: 1 (Table 1).Table 1. The distribution of patients by sex and age, n= 412
 |
| |
|
Patients were admitted to the hospital in terms from several hours to several days from the onset of LE complications. Thus, 11.6% of patients were admitted to the clinic within 24 hours after the onset of complications episode, 14.2% - before 48 hours, 22.8% - before 72 hours. 51.4% of patients were admitted at a later date. For the control, the patients were divided into two groups (Table 2).Table 2. The timing of patients admission since the development of parasitic liver disease complications, n= 412
 |
| |
|
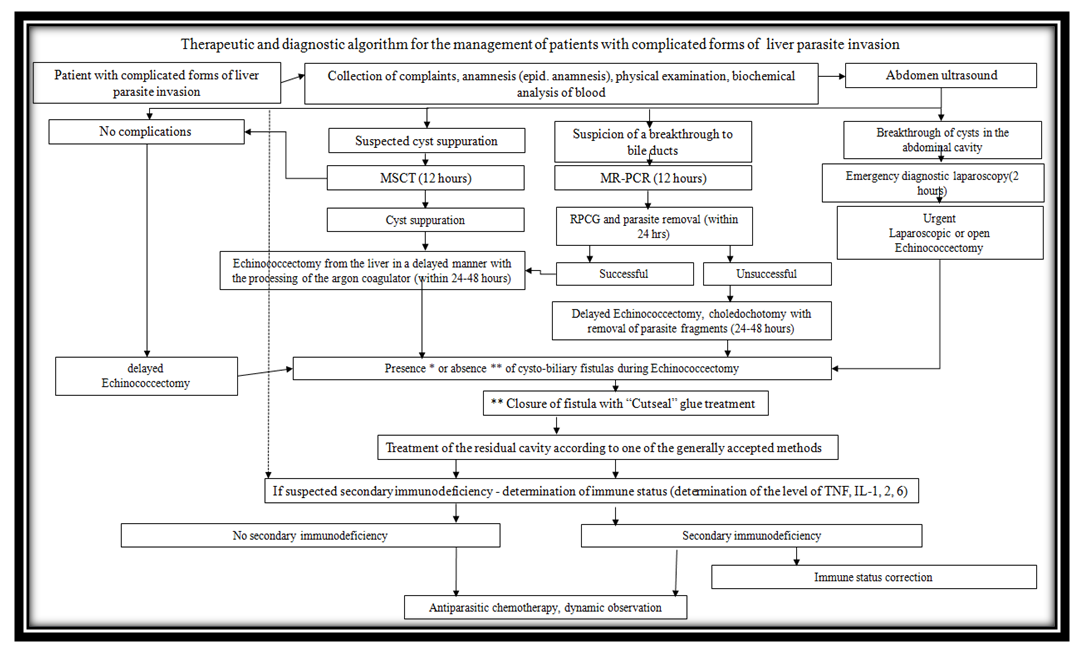
The reason for late diagnostics in some cases obviously was the complexity of diagnostics and the need for differentiation with a group of various emergency conditions, and to a greater extent - lack of public awareness about parasitic diseases and possible complications.All patients were admitted to the admission department with nonspecific symptoms more specific for the manifestations of cholelithiasis complications. In general, complaints of those patients at admission were similar to the classical picture of obstructive suppurative cholangitis (pain and a feeling of heaviness in the right or left hypochondrium, yellowing of the skin and sclera, fever to 39°C with chills, loss of appetite, dark urine color, clarification of the stool). However, a similar pattern was observed in 44% of cases, in 2 cases the detection of the parasitic obstruction of the common bile duct was a diagnostic finding.Clarity in the definition of the clinical diagnosis was made by the algorithm (Fig 1) of examination and treatment of patients with obstructive jaundice of parasitic etiology introduced in daily practice (the authors' testimony of Clinic No. 001038 of 11.15.2018), laboratory and instrumental methods of investigation. It should be noted that all the described patients at admission were in compensated and sub-compensated stages of liver failure.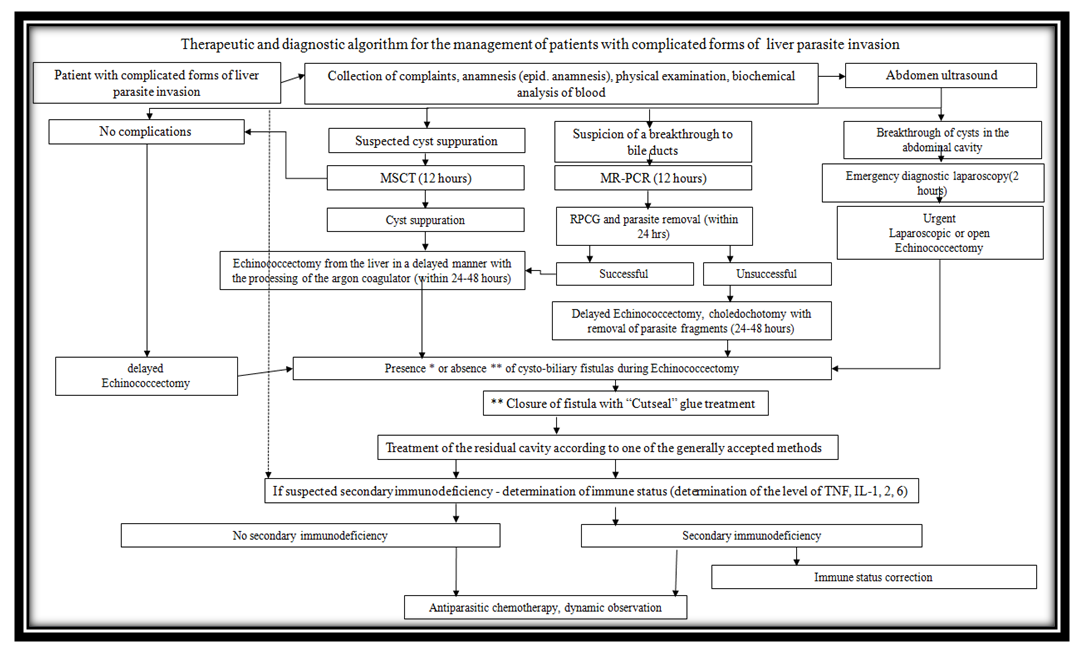 | Figure 1. Algorithm of examination and treatment of patients with obstructive jaundice of parasitic etiology |
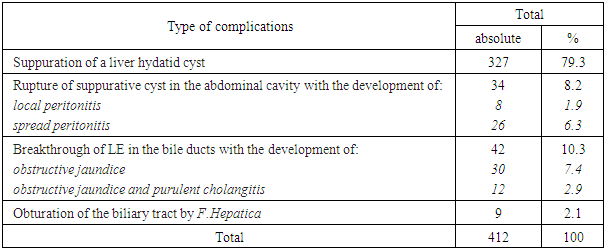
According to the algorithm, all patients underwent instrumental methods of research - ultrasound, CT, supplemented by enzyme immunoassay (ELISA) using human IgG and having specificity up to 95%. At the same time, only one patient (3.6%) had the ELISA result falsely negative (in the early period due to the technique of staging), in the rest of cases the ELISA result confirmed the clinical and instrumental presentation. All patients were performed a retrograde pancreatocholangiography (RPCG) which not only confirmed the diagnosis, but also was a therapeutic method on the first day of observation in the hospital (depending on the severity of the condition). Types of complications are presented in Table. 3Table 3. Types of surgical complications, n=412
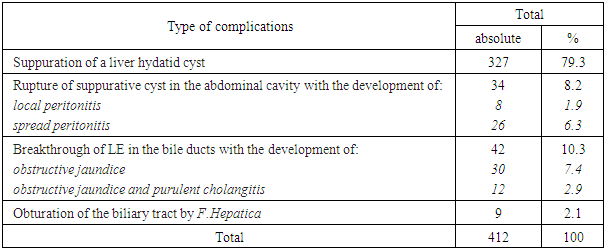 |
| |
|
3. Results
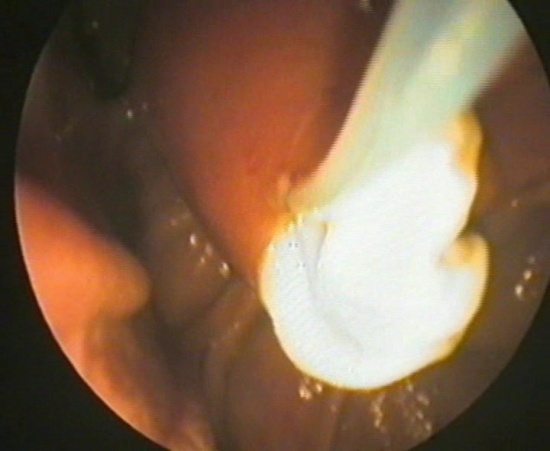
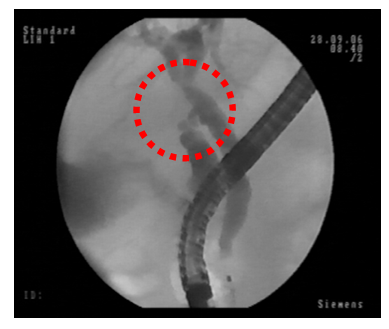
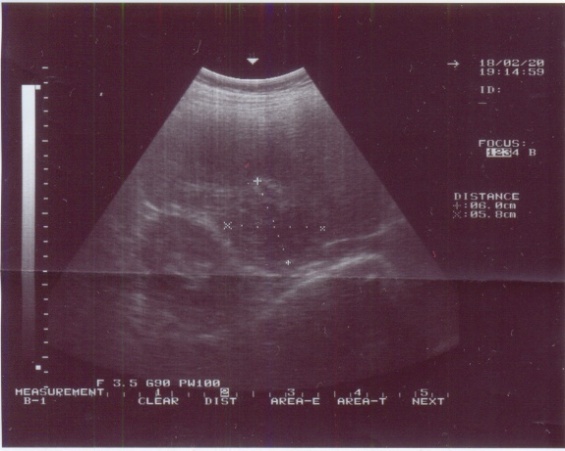
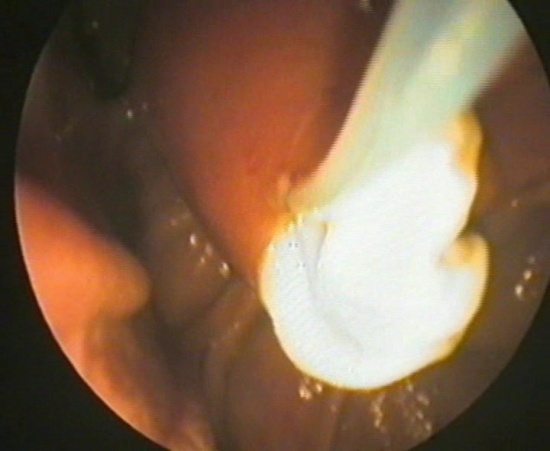
The main pathological processes are chronic proliferative cholangitis and pancreatic canaliculitis accompanied by various degrees of these organs fibrosis.Hyperplasic and inflammatory-sclerotic processes in the wall of the ampoule of the major duodenal papilla and in the mouth of the main pancreatic duct are important in the pathogenesis of diffuse cholangiectasia and pancreatic retention canaliculoectasis. The development of the thermal section of the common bile duct and cystic duct strictures is also characteristic. In some cases the course of the disease may be severe with obstruction of the bile ducts, development of jaundice, recurrent cholangitis, abscesses of the liver, acute pancreatitis and biliary peritonitis [4, 13-14].It is easy to understand that by persisting for years in the human body and not causing acute negative sensations, F.hepatica is rarely detected purposefully and only the occurrence of any serious complications (such as mechanical obstruction of the biliary tract) makes the patient visit a doctor. However, the absence of the so-called “parasitic caution” in the doctor leads to the fact that often the diagnosis is determined only intraoperatively.As an example, here is an extract from the case history No. 8124/624 of patient K.Patient K., 58 years old, was hospitalized at the Department of Emergency Surgery No. 1 of the RRCEM from March 3 to March 9, 2009 with pains and a feeling of heaviness in the epigastria and right hypochondrium, general weakness, yellowing of the skin, nausea, vomiting, loss of appetite, acholic stools, darkening of the urine.Ill for 6 days, noted pain in the right hypochondrium and epigastric pain. 2 days before admission, the onset of pain increased in waves, the clinic was supplemented by a sudden yellowing of the skin and visible sclera, an acholic stool appeared, he noted darkening of the urine.Objectively: the general condition upon admission is moderate. Consciousness is clear. Skin and sclera are yellow (+++). Palpable abdomen is soft, painful in the right hypochondrium and epigastric. The Shchetkin-Blumberg symptom is negative; the muscles of the anterior abdominal wall are not strained. The liver, gallbladder, spleen are not palpable. The stool is independent, acholic. Urine is dark colored.Surveyed: blood test: HB-118 g / l, RBC. -3.9 * 1012 / l, WBC.-9.8 * 109 / l, s / i-80%, Eosyn. 7%, Basophyles. 2%, Lymph. 10%, mon.1%. Total bilirubin -147.4 u / l, straight-54.5u / l, AcAT-68.5 u / l, AlAT-52.1. Ultrasound: in the right lobe of the liver in the projection of the V and VIII segment there is an education with irregular contours, 5.0 x 4.0 cm in size. The gallbladder 11.0 x 4.0 cm in the cavity there are stones up to 5 mm in size, choledoch 1, 0 cm (Fig. 3). X-ray of the lungs and abdomen without features.On 03.03.09 the patient underwent retrograde cholangiopancreatography (RPCG) which revealed an extension of the choledoch up to 12 mm (Fig. 2), produced by endoscopic papilla-sphyncterotomy (EPST) for 1.0 cm, resulting in obstruction of the bile duct of parasitic etiology / cholangitis. From the first attempt 2 worms up to 3 cm long were removed from the choledoch (Fig.3, 4).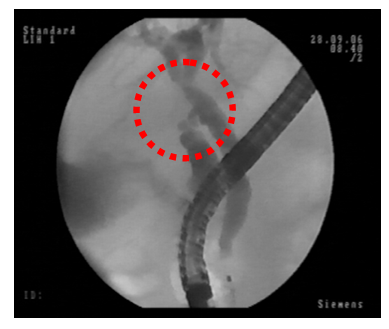 | Figure 2. Expansion of choledoch up to 11-12 mm |
 | Figure 3. View at RPCG: Liver fluke in duodenum |
 | Figure 4. Extracted F. hepatica worm |
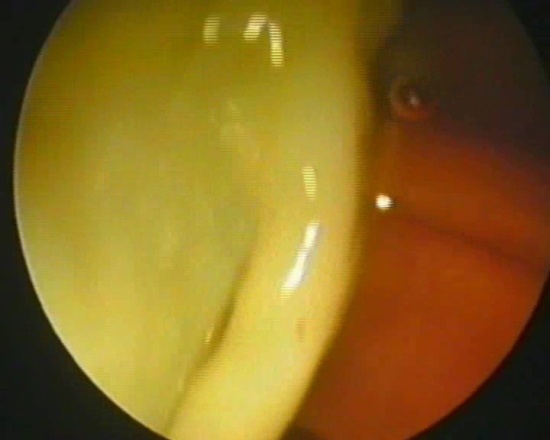
On the background of antibiotic therapy (metronidazole and cefaxime), the patient's condition with a noticeable improvement, control ultrasound of the biliary ducts of March 8, 2009 - choledoch 8 mm, volume formation in the projections of the V and VIII segments of the liver with a decrease in size 3.0 x 2.0 cm. Blood biochemistry in dynamics: total bilirubin 46.7 u / l; straight-21 u / l; Aspartat-aminotransferaze- 31.0 u / l; Alanine-aminotransferaze - 44.0. The patient in satisfactory condition was discharged for outpatient treatment with the recommendations of anti-parasitic medicine taking.Metabolism products of F.Hepatica helminthes cause toxic and allergic reactions which are most clearly manifested in the early period of the disease. Toxic-allergic reactions cause irritation of the nerve endings of the bile ducts which leads to the appearance of viscera-visceral reflexes that affect the functional state of the gastrointestinal tract and pancreas. In the later period of the disease, an enlargement of the duct lumen, thickening of the walls and adenomatous growth of the bile ducts epithelium occur, purulent cholangitis is developed [2-3, 6].All patients with suspected breakthrough of a hydatid cyst in the biliary tract on the first day (depending on the severity of the condition) were performed retrograde pancreatocholangiography (RPCG) for confirming the diagnosis. At the same time, an increase of the choledoch of more than 20 mm was observed in 3 patients (10.7%), 20-15 mm – in 14 patients (50%), 9-15 mm – in 11 patients (39.3%). It was not difficult to define the diagnosis after EPST (Fig. 5, 6).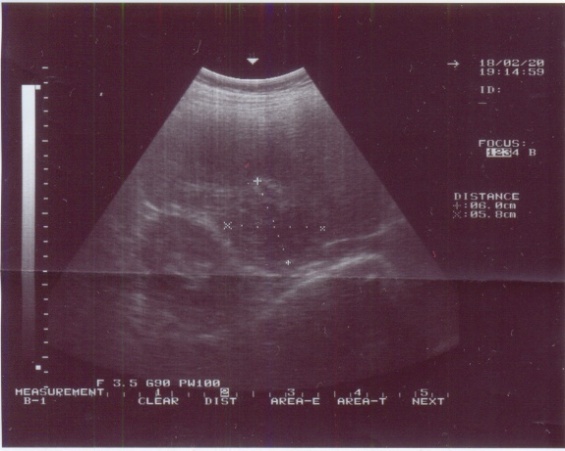 | Figure 5. Ultrasound signs of Hydatid cyst in V-VI liver segments |
 | Figure 6. EPST. Bulging of longitudinal fold |
In 20 cases (72%) after EPST the chitin membranes were removed with Dormia basket. The mechanical block was eliminated by washing the biliary tract with 0.06% sodium hypochlorite solution (Fig. 7, 8). Further these patients were performed open surgery in a delayed manner. In 8 cases (28%) the attempts to remove chitin shells were unsuccessful and mechanical jaundice could not be solved. Those patients were also performed surgery, but in urgent manner.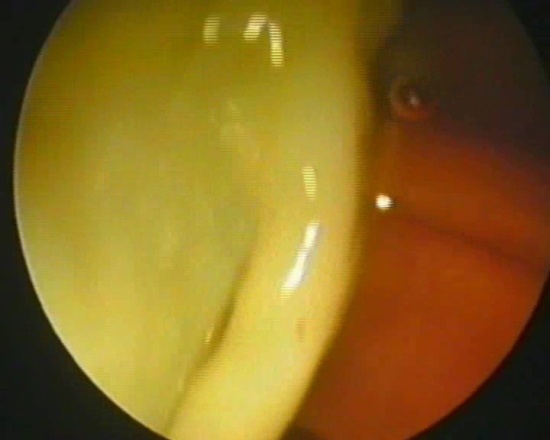 | Figure 7. EPST. Prolapse of chitin shell |
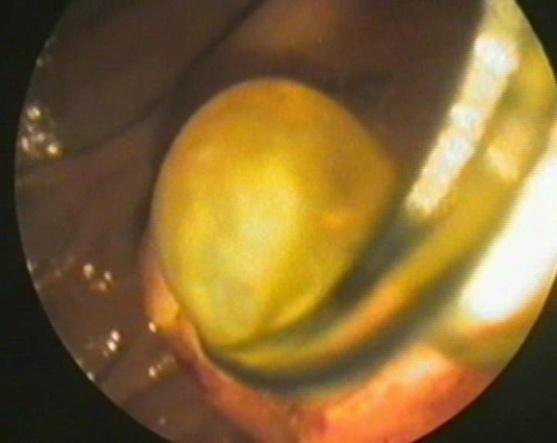 | Figure 8. Extraction of a daughter cyst |
Patients with a breakthrough of a hydatid cyst in the biliary tract and the occurrence of obstructive jaundice after RPCG were performed echinococcectomy according to the methods adopted in the clinic and described in the literature which in 16 cases were supplemented by pericystectomy with suturing of the residual cavity on the drainage tube.The choice of surgical tactics during operations aimed at eliminating of residual cavities and correcting of the bile ducts lesions depended on the location, size and number of hydatid cysts and their connection with the bile ducts. Calcification of the fibrous capsule was considered to be an absolute indication for pericystectomy, the remaining of which, as shown by our research and data from other surgeons was the cause of suppuration of the residual cavities and persistent of external gall-purulent fistula. A pericystectomy was performed precisely using an argon plasma scalpel, avoiding damage of the liver tubular structures, but without harm to the surgery adequacy. In all cases, the calcified areas of the fibrous capsule were removed and the unusually starred parts which were intimately welded to the vessels or bile ducts were partially dissected, leaving only small areas of the capsule safely. One of the important elements of echinococcectomy from the liver is the observance of the principle of anti-parasiticity (reliable isolation of the wound and disinfection of the germ elements of the parasite during the surgery). The most secure, simple and effective method using 80% sterile glycerin with an exposure time of 10 minutes from the currently proposed methods of antiparasitic treatment of hydatid cysts was used in the RRCEM clinic. And in some cases the treatment of the residual cavity with defocused argon plasma coagulator rays was used.
4. Conclusions
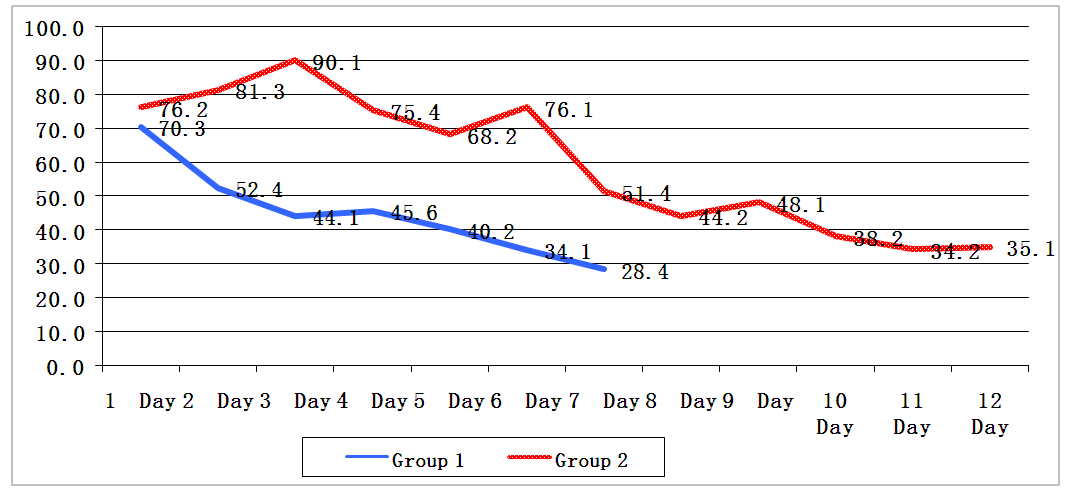
The analysis of the medical records, as well as the rest of the patients in this group, showed the following patterns. All the representatives of the described patients group were residents of rural areas. It once again underlines the need to strengthen sanitary and educational work and to increase e the hygienic literacy of the population.Also, all the described patients had gallstone disease. It, of course, confirms literary sources of the presence of causal relationships between the parasite and the host at the organism and cellular levels. According to recent data, the main pathological process is chronic proliferative cholangitis and pancreatic canaliculitis accompanied by various degrees of these organs fibrosis. Hyperplasic and inflammatory-sclerotic processes in the wall of the ampoule of the major duodenal papilla and in the mouth of the main pancreatic duct are important in the pathogenesis of diffuse cholangiectasia and pancreatic retention canaliculoectasis.In patients who were successfully performed retrograde resolution of obstructive jaundice before the open surgery (group 1) there was a significant decrease of liver failure as early as the second or third day after RPCG.At the same time, in patients operated on at the peak of obstructive jaundice due to an unsuccessful attempt of choledoch unblocking (group 2), a longer period of bilirubin level recovery was observed (Diagram 1).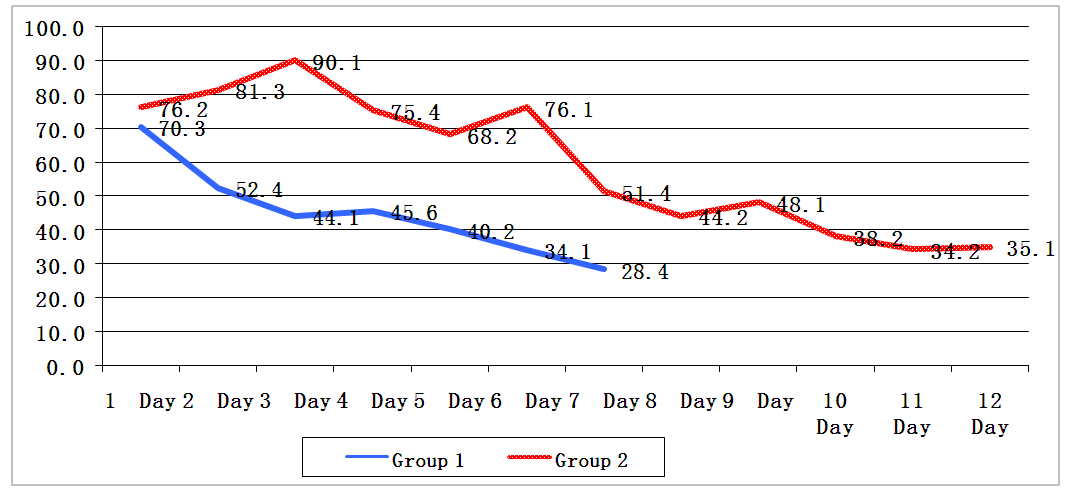 | Diagram 1. Comparative indicators of bilirubin level in 2 groups of patients (mean values, µmol/L; p<0.01) |
As it can be seen from the above diagram, a decrease in bilirubin up to almost normal values was observed in patients with successful retrograde unblocking by 6–7 days, while in the second group of patients this period mad up 11–12 days. When treating patients of group 1, it was managed to confine by minimally invasive intervention without the use of traumatic surgical methods which significantly reduced the patient's stay (average bed-day 4.9 ± 1.3) and also the cost of treatment.Carrying out of preoperative RPCG allowed not only to reduce the possible postoperative mortality by timely solution of biliary hypertension, but also allowed to determine the relationship of cysts with the main bile ducts and vessels and thereby to reduce the frequency of their accidental injury.The development of strictures of the thermal section of the common bile duct and cystic duct is also characteristic – we observed it in our patients. In some cases, the course of the disease can be severe with obstruction of the bile ducts, development of jaundice, recurrent cholangitis, abscesses of the liver, acute pancreatitis and biliary peritonitis. At the same time, we could not study what is the root cause in this case - parasitic invasion or cholelithiasis.Thus, purposeful retrograde examination of the biliary tract is not only a highly specific diagnostic method, but also a therapeutic method that can eliminate the cause of obstructive jaundice, adequately sanitize the biliary tree and reduce the risk of postoperative complications. The introduction of minimally invasive interventions into daily practice has led to a high professional level of specialists.The choice of tactics for complex diagnostics and treatment for this type of patients makes it possible to provide adequate and timely emergency assistance to patients and reduce the costs of their postoperative rehabilitation.
References
| [1] | Abdulloev A.G., Movchun A.A., Agayev R.M. Surgical tactics at echinococcosis of the liver with bile ducts lesion // Surgery. 2005. No. 2. P. 38–42. (In Russ) |
| [2] | Agaev R.M. The use of laser radiation in the surgical treatment of patients with liver echinococcosis / R.M. Agaev, R.E. Jafarli // Annals of surgical hepatology. - 2006. - Vol. 11, No. 3. - P.37-38. (In Russ) |
| [3] | Vetshev, P.S. Obstructive jaundice: causes and diagnostic approaches (lecture) / P.S. Vetshev / / Annals of Surgical Hepatology. - 2011.-Vol. 16, No. 3.-P. 50-57. (In Russ) |
| [4] | Vetshev, P.S, Musaev, G.Kh. Echinococcosis: state of the problem // Annals of surgical hepatology. 2005. No. 4. P. 7–12. (In Russ) |
| [5] | Diagnosis and surgical tactics in obstructive jaundice syndrome / Yu.L. Shevchenko, P.S. Vetshev, Yu.M. Stoyko et al. // Annals of surgical hepatology. - 2008. - Vol. 13, №4. - P. 96-105. (In Russ) |
| [6] | Kubyshkin V.A., Vishnevsky V.A., Kakharov M.A. Evolution of methods of surgical treatment of liver echinococcosis. Annals of surg. hepatol. 2002; 7: l: 18-22. (In Russ) |
| [7] | Machulin E.G. Obstructive jaundice of non-tumor genesis. Minsk: Harvest 2000. |
| [8] | Nazirov, F.G., Ilkhamov, FA. Surgical treatment of complicated liver echinococcosis // Annals of surgical hepatology.- 1999.- Vol. 4. - №1.-P.96-97. (In Russ) |
| [9] | Shevchenko Yu. L., Nazirov F.G. Echinococcosis surgery (monograph). Moscow, Dynasty, 2016, 288; P.72-86. (In Russ) |
| [10] | Becker K., Frieling Т., Saleh A., Haussinger D. Resolution of hydatid liver cyst by spontaneous rupture into the biliary tract. J Hepatol 1997; 26: 6: 1408-1412. |
| [11] | Chitsulo, Montresor, and Savioli. New opportunities for the control of fascioliasis.// Bulletin of the World Health Organization. 16 May 2001. |
| [12] | Cook GC. Parasitic infections of the gastrointestinal tract: a worldwide clinical problem. Curr Opin Gastroenterol 1989; 5: 126-139. |
| [13] | Hong ST et al. Infection Status of Hydatid Cysts in Humans and Sheep in Uzbekistan // Korean J Parasitol. 2013 Jun; 51(3): 383–385. |
| [14] | Kiladze M. et al. Obstruction of common bile duct caused by liver fluke--Fasciola hepatica. PubMed ID 11220154. |
| [15] | PAIR: Puncture, Aspiration, Injection, and Re-Aspiration. An option for the treatment of Cystic Echinococcosis. WHO/CDS/CSR/APH/2001.6 // World Health Organization, Department of Communicable Disease, Surveillance and Response. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML