-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(6): 194-196
doi:10.5923/j.ajmms.20190906.04

Screening Diagnostics of Oral Precancerous Diseases
Khaydar Kamilov1, Aliya Kadirbaeva1, Karima Musaeva2
1Hospital Therapeutic Dentistry Department, Tashkent State Dental Institute, Tashkent, Uzbekistan
2Hospital Prosthodontics Department, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Aliya Kadirbaeva, Hospital Therapeutic Dentistry Department, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chronic diseases of oral mucosa are characterized by growing number of patients every year and unsatisfactory results of treatment. A persistent clinical course is typical some diseases of oral mucosa, and it tends to malignancy in 20-30% of cases. Research was dedicated to determination of dispersed luminous particles’ (DLP) role in diagnostics of oral precancerous diseases. 130 patients with various forms of leukoplakia, oral lichen planus, traumatic ulcers, dysplasia of oral mucosa were examined at the Department of Therapeutic Dentistry, Tashkent State Dental Institute clinics. DLP was detected both inside the cells and in the intercellular space in cases with maligning processes. Determination of DLP can be considered as screening method of oral precancers diagnostics.
Keywords: Oral precancerous diseases, Oral mucosa, Leukoplakia, Lichen planus, Dysplasia of oral mucosa
Cite this paper: Khaydar Kamilov, Aliya Kadirbaeva, Karima Musaeva, Screening Diagnostics of Oral Precancerous Diseases, American Journal of Medicine and Medical Sciences, Vol. 9 No. 6, 2019, pp. 194-196. doi: 10.5923/j.ajmms.20190906.04.
Article Outline
1. Introduction
- Chronic diseases of the oral mucosa and red lips, accompanied by keratinization of the epithelium, are rather extensive group of pathological processes that attract the attention of dentists, oncologists, dermatologists and pathologists due to long clinical course with varying degrees of maligning likelihood and considered by most experts as precancerous lesions [1].The urgency of the problem is due to the increase in the number of patients with this pathology in recent years. At present, according to a summary of various authors, precancerous processes in the oral cavity are found in 4.5% of cases [2, 3, 15]. The frequency of chronic inflammatory processes of the mucous membrane of the cavity of the mouth and the red border of the lips, which may precede precancerous lesions, corresponds to 19.9% [5, 8, 9, 10]. The lack of statistically reliable data in this area does not allow us to estimate the true frequency of these changes in the general statistics of the pathology of the oral mucosa [6, 7, 11, 13].According to literary sources, precancerous lesions make up 15.2-84.9% of all diseases of the oral mucosa [4]. Therefore, early diagnosis using screening methods for the active detection of precancerous diseases of the oral mucosa and the early stages of asymptomatic cancer is of particular relevance [12, 14, 16].
2. Object of Research
- Taking into account the urgency of the problem, the object of our research was to study the content of disperse luminescent particles (DLP) in precancerous processes in the oral mucosa, to improve early detection of precancerous processes, and to apply cytological examination of smears from the oral mucosa to determine the DLP in clinical practice.
3. Material and Methods of Research
- The analysis of the results of minimally invasive modern methods for oral precancerous processes diagnosing was carried out on a fairly large clinical material. 130 patients at the age of 25-70 years old were examined for the presence of DLP at the Department of Therapeutic Dentistry, Tashkent State Dental Institute. Early diagnosis is important in preventing the development of cancer of the oral mucosa. One of the methods that provide early diagnosis of precancerous diseases is the cytological method, which is convenient and simple for mass prophylactic examinations using the AK method (Abdullakhodzhayeva-Krakhmalev). The native smear was viewed in an Axiovert 40 inverted microscope. The cells and the extracellular space were examined for the presence of dispersed luminous particles (DLP) at a magnification of 16x50.AK method needs no special paints or other preparing of smears, only native smear from oral mucosa and microscope. It gives result in several minutes. Normally, the DLP are absent. In pathology (precancerous processes, cancer at an early stage, carcinoma in situ, cancer), there is the presence of the internal and extracellular DLP, also they can be found in red blood cells, monocytes. DLP have a rounded shape, glow in the reflected light colours of the spectrum of visible light.
4. The Results of the Study
- 80 patients were diagnosed with leukoplakia, 40 patients had erosive-ulcerative lichen planus (OLP), and 10 patients had signs of malignancy of the oral mucosa. Also in the study it was noted that erosive and ulcerative form of lichen planus took the leading position in the structure of oral precancerous lesions, by 44.12% cases (75 people). Verrucous leukoplakia was in 38.82% (66) patients. Traumatic ulcer of oral mucosa was detected in 1.53% (2) patients. It was found that lichen planus was significantly more common in women (6.46% vs. 2.15% in men, p <0.05). Also a statistically significant increase in the incidence of oral mucosa with increasing age was noted. Thus, the frequency of detection of oral cancer among patients of 56-60 years was significantly higher compared with age group of 40-45 years (1.08 ± 0.09% and 0.68 ± 0.08%, respectively, p <0.05). In addition, there was a significant prevalence of the frequency of traumatic ulcers of oral mucosa and verrucous leukoplakia in the older age group (56-60 years) compared with patients aged 40-45 years. The clinical examination revealed that among the signs of most common oral precancerous diseases were such as oral pain in 39.22% of patients, as well as a burning sensation in 21.56% of cases.
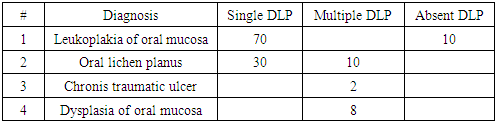
|
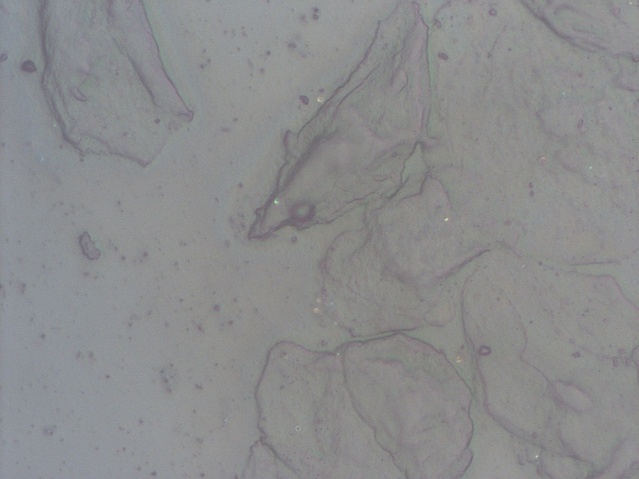 | Figure 1. Single DLP in the extracellular space of a patient with leukoplakia |
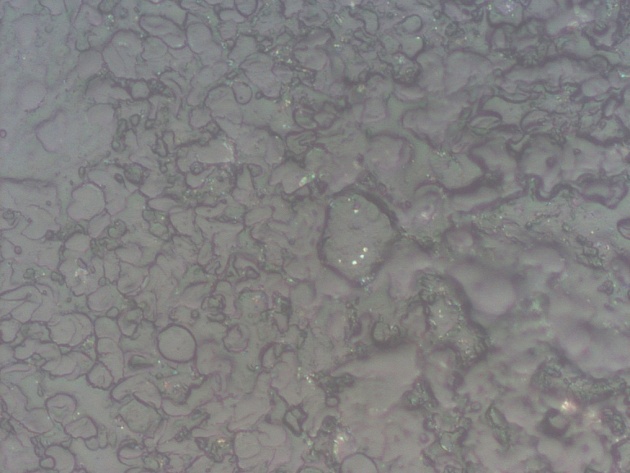 | Figure 2. Multiple DLP in the cytoplasm of cells and the intercellular space. A patient with dysplasia of the oral mucosa |
5. Conclusions
- Thus, the express method for determining the DLP allows the detection of precancerous pathology of the oral mucosa without the use of expensive chemical dyes, while being informative, with high sensitivity and specificity. Early detection of potential pre-cancerous processes allows avoiding interventional diagnostic methods, as well as reducing the risk of developing oral mucosa cancer. It should also be noted that for all merits, this system has low specificity and does not allow differential diagnosis of precancerous and malignant changes of oral mucosa. The problem of early diagnosis of precancerous diseases is becoming due to the wide spread of this pathology, its less symptomatic course and non-specific external manifestations. All this is the reason for the late admission of patients for medical care, which, in turn, leads to a high percentage of malignancy and cases of arrested cancer. Meanwhile, taking into account the tendency to rejuvenate the evil lesions of oral mucosa, their severe course and unresolved treatment tactics, it becomes obvious that the most effective way out of this situation is the introduction of new methods into widespread dental practice screening diagnosis of oral precancers.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML