-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(6): 184-189
doi:10.5923/j.ajmms.20190906.02

Effect of Serum Level Changes of Electrolytes during Hemodialysis Sessions on Cardiac Rhythm in Patients with Maintenance Hemodialysis
Osama Mohamad Ahmad1, Mohamed Sayed Bashandy2
1Internal Medicine Department, Al-Azhar University, Faculty of Medicine Damietta, Egypt
2Cardiology Department, Al-Azhar University, Faculty of Medicine Damietta, Egypt
Correspondence to: Osama Mohamad Ahmad, Internal Medicine Department, Al-Azhar University, Faculty of Medicine Damietta, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: End-stage renal disease is a global public health burden bearing high morbidity and mortality, and cardiovascular (CV) disease is a major cause of mortality in hemodialysis (HD) patients. Aim of the study: detection the effect of electrolyte disturbance on cardiac rhythm during hemodialysis session in chronic hemodialysis patients. Patients and methods: This prospective observational study included 42 chronic hemodialysis (HD) patients on regular HD came to the hemodialysis center of Al-Azhar University Hospital New Damietta. The study was carried out over a period from July 2017 to May 2018. All the patients received HD three times per week, and each HD session was performed for 3.5–4.5 hours with a blood flow rate of 250–300 mL/min and dialysate flow of 500 mL/min, Standard 12 lead ECGs (10 mm/mv and 25 mm/sec) were done for all patients before and after HD, and Two dimensional transthoracic echocardiography was performed for all patients after HD session. Results: This study included 42 patients with chronic renal failure on regular HD, their age ranged between 31 and 58 years (mean±SD = 46.7±8.7 years), males represented 85.7% of them, 28.6% were diabetics, 90.5% were hypertensive and 9.5% had hepatitis C virus. There was statistically significant decrease of electrolyte levels after dialysis when compared to values before dialysis. QT interval and QTc were significantly decreased after dialysis while QT dispersion and QTc dispersion were significantly increased. Conclusion: Cardiac arrhythmia is a frequent finding in HD patients affecting 85.7% of our study population. The prevalence of AF among those patients is more than double its prevalence among general population. This increase in the prevalence of cardiac arrhythmia especially AF seems to be due to electrolyte disturbance and autonomic disturbance as reflected by QT dispersion.
Keywords: Hemodialysis, Cardiovascular
Cite this paper: Osama Mohamad Ahmad, Mohamed Sayed Bashandy, Effect of Serum Level Changes of Electrolytes during Hemodialysis Sessions on Cardiac Rhythm in Patients with Maintenance Hemodialysis, American Journal of Medicine and Medical Sciences, Vol. 9 No. 6, 2019, pp. 184-189. doi: 10.5923/j.ajmms.20190906.02.
Article Outline
1. Introduction
- End-stage renal disease is a global public health burden bearing high morbidity and mortality, and cardiovascular (CV) disease is a major cause of mortality in hemodialysis (HD) patients [1].Sudden cardiac death is one of the major causes of mortality in end-stage renal disease patients under maintenance hemodialysis beside cardiac arrhythmias especially ventricular arrhythmias [2].Electrolytes have been also attributed to the genesis of arrhythmia, especially hyperkalemia and hypokalemia [2].Several electrocardiographic methods can be used to assess cardiac arrhythmia risk, including measurement of the (QT interval and dispersion, signal averaged ECG and heart rate variability) [3].
2. Aim of the Study
- Recognition the effect of electrolyte disturbance on cardiac rhythm during hemodialysis session in chronic hemodialysis patients.
3. Patients and Methods
3.1. Study Design
- This prospective observational study included 42 chronic hemodialysis (HD) patients on regular HD came to the hemodialysis center of Al-Azhar University Hospital New Damietta. The study was carried out over a period from July 2017 to May 2018. All the patients received HD three times per week, and each HD session was performed for 3.5–4.5 hours with a blood flow rate of 250–300 mL/min and dialysate flow of 500 mL/min.Those patients with inability to achieve the dry weight, immeasurable T waves, atrial fibrillation, bundle branch block, pacemaker, anti-arrhythmic drugs that lengthen the QT interval, and/or impaired ejection fraction (EF<40%) were excluded from the study.
3.2. Ethical Aspects
- The study procedure doesn't interfere with any ethical basics and oral agreement was taken to all patients.
3.3. Study Protocol
- All patients were subjected to history taking with emphasis on presence of heart-related symptoms, medical treatment, duration of HD, and presence of cardiovascular risk factors (diabetes mellitus, hypertension, dyslipidemia etc.), complete general and cardiac examination, and calculation of body weight before and after HD.Standard 12 lead ECGs (10 mm/mv and 25 mm/sec) were done for all patients before and after HD to calculate QT intervals for each lead (from the beginning of QRS to end of T wave), QTc [corrected QT interval, calculated using Bazett’s formula (QTc = QT interval/√RR interval)], QT dispersion (QT max – QT min) and QTc dispersion (QTc max – QTc min).Two dimensional transthoracic echocardiography was performed for all patients after HD session (to exclude those with EF<40%) at echocardiogrhy laboratory at Al-Azhar University Hospital New Damietta using Philips IE 33 (Philips Ultrasound, 22100 Bothell Everett Highway, Bothell, WA, 98021 USA). The probe used was S-5 phased array sector probe (frequency range 1.5-4.3 MHz).Patients underwent Holter ECG monitoring before (half an hour), during and after HD (4 hours), to detect occurrence of arrhythmia using Meditech Kft, Hungary, 3 channel holter, Model: cardioblue 24.Laboratory investigations were taken before and after HD session, including serum sodium, potassium, magnesium, calcium, CBC, blood urea, serum creatinine, and albumin.
3.4. Statistical Analysis
- The collected data were organized, tabulated and statistically analyzed, using Statistical Package for Social Science (SPSS) version 16 (SPSS Inc, Chicago, USA), running on IBM compatible computer. For qualitative data, frequency and percent distribution were calculated and for comparison between groups, Fisher exact test was used. For quantitative data, mean and standard deviation were calculated, and student (t) test was used for comparison. For interpretation of results p ≤ 0.05 was considered significant.
4. Results
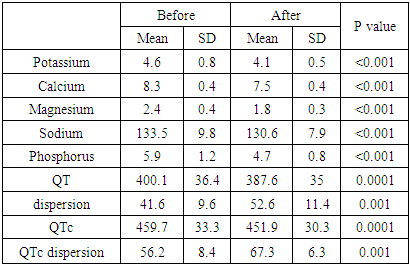
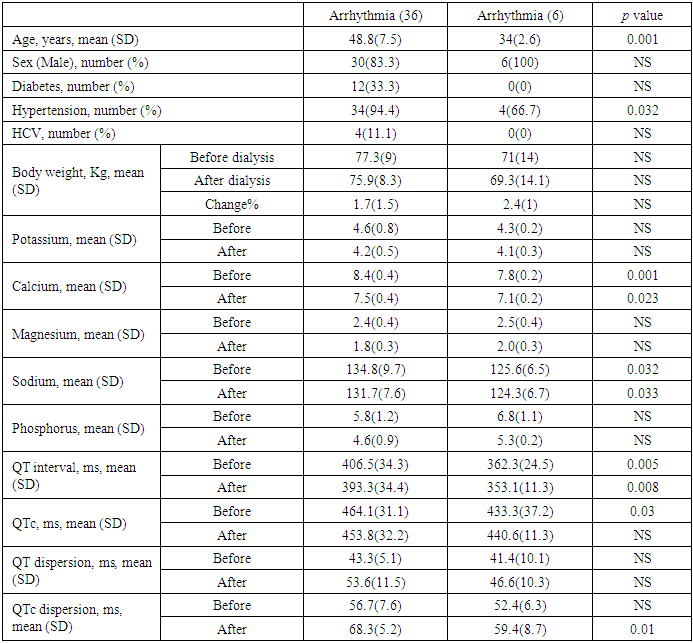
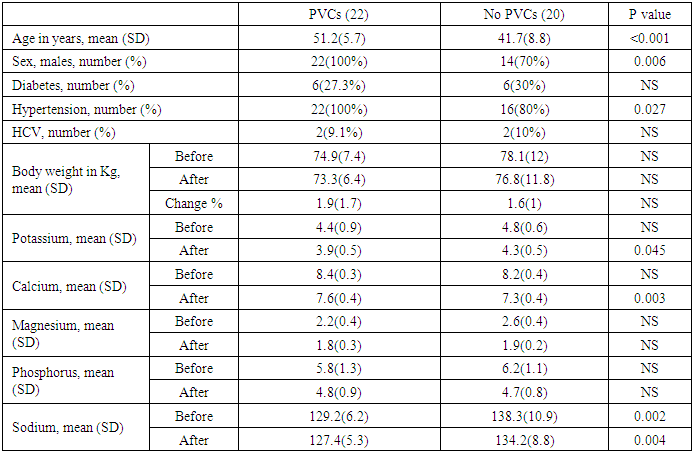
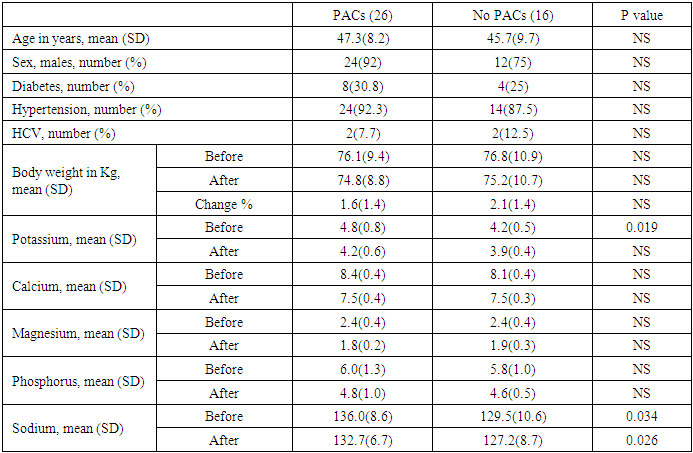
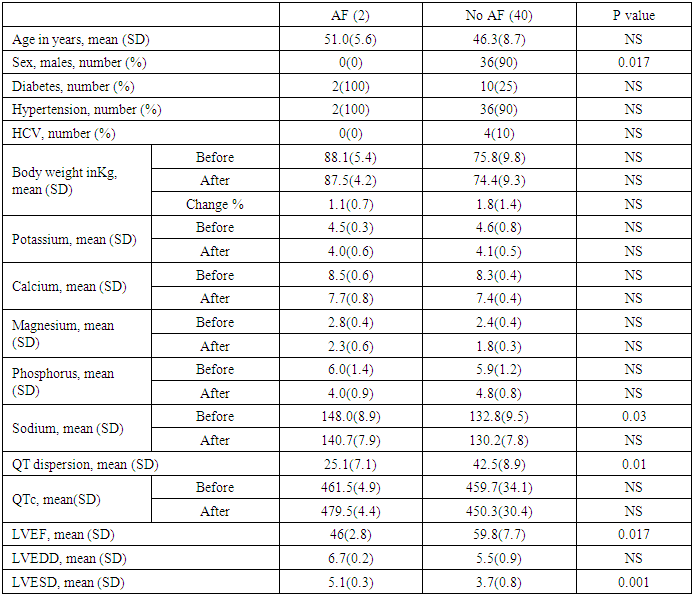
- This study included 42 patients with chronic renal failure on regular HD, their age ranged between 31 and 58 years (mean±SD = 46.7±8.7 years), males represented 85.7% of them, 28.6% were diabetics, 90.5% were hypertensive and 9.5% had hepatitis C virus. There was statistically significant decrease of electrolyte levels after dialysis when compared to values before dialysis. QT interval and QTc were significantly decreased after dialysis while QT dispersion and QTc dispersion were significantly increased.Arrhythmias developed in 85.7%, PVCs (premature ventricular contraction) in 52.4%, PACs in 61.9%, and AF in 4.8%. When comparing patients who developed arrhythmias to those who did not regarding patient demographics, associated medical disease and body weight, those developed arrhythmia were significantly older and had higher prevalence of hypertension (p=0.001 and 0.032 respectively) [table]. There were significantly higher levels of serum sodium and calcium before and after dialysis among patients who developed arrhythmia when compared to those did not. There were no significant differences between them regarding other electrolytes [table]. QT before and after dialysis, QTc before dialysis and QTc dispersion after dialysis were significantly higher in those developed arrhythmia. Patients who developed PVCs were significantly older, males, and had more hypertension prevalence. Patients who developed PVCs had significantly lower serum potassium after dialysis, higher serum calcium after dialysis, and lower serum sodium before and after dialysis when compared to those who did not develop PVCs. There was no significant difference between those had PACs and those did not regarding patient demographics, associated medical disease or body weight. Patients who developed PACs had significantly higher serum potassium before dialysis and also higher serum sodium before and after dialysis when compared to those who did not develop PACs. There was no significant difference between those had AF and those did not regarding patient demographics, associated medical disease and body weight except for female predominance in those developed AF. Regarding echocardiographic and Holter parameters, those who developed AF had significantly lower EF, larger LVESD and less QT dispersion when compared to those did not. Patients who developed AF had significantly higher serum sodium before dialysis when compared to those who did not.
|
|
|
|
|
5. Discussion
- In CKD patients, the increased susceptibility of ventricular arrhythmias seems to be related to metabolic disturbances and cardiac structural disorders caused directly by renal dysfunction. According to the United States Renal Data System (USRDS), the leading cause of death among HD patients is related to cardiac arrhythmias [4].In HD patients, CV autonomic neuropathy and the related risk of arrhythmia may partially explain the observed high rate of CV mortality besides the traditional risk factors, including hypertension, diabetes, and dyslipidemia [5].Increased dispersion of QT intervals is known to predispose to ventricular arrhythmias and sudden cardiac death. Among the noninvasive techniques which can be useful in predicting the patients at risk for sudden death is the measurement of QT interval changes [6].This prospective observational study was conducted at cardiology department of Al Azhar university hospital (New Damietta). The study was carried out over a period from July 2017 until May 2018. The study included 42 patients on regular HD three times weekly.Arrhythmias developed in 85.7%, the most common arrhythmia was PACs in 61.9%, then PVCs in 52.4%, while AF developed only in 4.8%. No patients developed supraventricular tachycardia, sustained/non-sustained ventricular tachycardia, or ventricular fibrillation.These results are somewhat similar to those of [7], who studied 70 patients with CRF on chronic HD, they reported that the most common arrhythmia found were PVC 64%, PAC 40%, and AF developed only in 2.7%. No patients in their study developed serious ventricular arrhythmia.Kaya et al., 2018 [8] Studied 59 CRF on HD and they reported that prevalence of arrhythmia was 78%, atrial arrhythmia in 74%, ventricular arrhythmia in 68%. AF was present in two patients (3.4%) in the form of paroxysmal AF.In our study AF developed in 4.8% of study population which is higher than the incidence of AF in general population which ranges between 1.5 and 2% in middle-east countries [9], this can be explained by change in serum levels of electrolytes and metabolites, acid-base imbalance, reduced circulating blood volume, and sympathetic overactivity during dialysis.Hiroshi and his colleagues (2009) [10] followed up patients with kidney dysfunction for 6 years and found increased risk of new onset of AF among them.Soliman and his colleagues (2010) [11] reported that the prevalence of AF in CKD patients was around 20%, also Ananthapanyasut and coworkers (2010) [12] reported that the prevalence of AF among CKD patients was 21.2% which is much higher than our study which can be explained by our exclusion of pre-existing AF patients. Bansal and his colleagues (2014) [13] followed up CKD patients without pre-existing AF for five years, and found that the prevalence of AF among them was 7.7%.Change in electrolyte concentration is a risk factor for cardiac arrhythmia. Potassium plays an important role in depolarization and repolarization of the cardiac cells [14].Hypokalemia or hyperkalemia may trigger arrhythmias by altering the trans-membrane potential [15]. Hypokalemia is a stronger risk factor than hyperkalemia [14]. In our study those developed PVCs had significantly lower serum potassium levels after dialysis when compared to those did not, while those developed PACs had significantly higher serum potassium levels before dialysis than those did not which raise the importance of change in level of serum potassium level in developing arrhythmia.
6. Conclusions
- Cardiac arrhythmia is a frequent finding in HD patients affecting 85.7% of our study population. The prevalence of AF among those patients is more than double its prevalence among general population. This increase in the prevalence of cardiac arrhythmia especially AF seems to be due to electrolyte disturbance and autonomic disturbance as reflected by QT dispersion.
Abbreviations
- HD
 HemodialysisCV
HemodialysisCV  cardiovascular
cardiovascular Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML