-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(5): 174-179
doi:10.5923/j.ajmms.20190905.04

Surgical Treatment Results of Patients with Mitral Valve Insufficiency
Nazirov Feruz Gafurovich, Aliyev Sherzod Makhmudovich, Pulatov Lazizzhon Abdukhamidovich, Ilkhomov Oybek Erkinovich
Republican Specialized Scientific and Practical Medical Center of Surgery named after Academician V.Vakhidov, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to compare the results of mitral valve reconstruction with application of various methods of valvuloplasty using a strip of synthetic fixed-length prosthesis and plasty with a rigid support ring. Material and methods: 65 surgeries in patients with mitral insufficiency of III-IV degree at the age of 18 and 65 years (mean age 46.7 ± 14.2 years) were performed in the Department of Combined Heart Disease Surgery between October 2012 and April 2017. According to echocardiography, mitral insufficiency of III degree was noted in 64.6% of cases, severe (IV degree) of insufficiency - in 35.4% of patients. Depending on the method of performing plastic surgery the patients were divided into 2 groups. Group I - 56 (84.4%) patients who underwent resection of the prolapse site or the creation of a neohord or translocation of chords with implantation of Carpentier’s support ring of various sizes depending on the diameter of the fibrous ring. Group II - 9 (13.8%) patients who underwent resection of the prolapse site using a strip of polytetrafluoroethylene (PTFE). Results: There were no lethal outcomes at the hospital stage. According to echocardiography, both groups maintained a positive trend. Patients survival after 12 months made up 98.5%, after 24 months - 90.5% and by the end of 38 months - 87.5%. Freedom from reoperation of patients after mitral valve plasty for 12 months made up 92.3%, for 24 months - 87.5%, for 38 months - 82.7%. After mitral valve plasty on the support ring reoperation (mitral valve replacement) was observed in 3 cases. There were no reoperations at mitral valve plasty with the use of a strip from PTFE. Conclusion: It is advisable to perform valvuloplasty techniques with the mandatory implantation of a rigid support ring for prolapses of the anterior cusp and both cusps of the mitral valve with dilatation of the left ventricular cavity. It is possible to perform resection techniques of valvuloplasty using a strip from synthetic prosthesis (PTFE) for the isolated prolapse of the posterior cusp central part (zone P2).
Keywords: Mitral valve insufficiency, Mitral valve surgery, Valvuloplasty
Cite this paper: Nazirov Feruz Gafurovich, Aliyev Sherzod Makhmudovich, Pulatov Lazizzhon Abdukhamidovich, Ilkhomov Oybek Erkinovich, Surgical Treatment Results of Patients with Mitral Valve Insufficiency, American Journal of Medicine and Medical Sciences, Vol. 9 No. 5, 2019, pp. 174-179. doi: 10.5923/j.ajmms.20190905.04.
1. Introduction
- Mitral insufficiency (MI) is the second most common heart disease that requires surgical treatment [1, 6, 10, 19]. Previously, chronic rheumatic heart disease was leading in the structure of the causes of isolated mitral valve insufficiency (MVI). Now, along with the insufficiency of ischemic genesis, the dominance of syndromes characterized by degenerative valve changes is observed. This condition is characterized by a number of morphofunctional disorders in the mitral valve (MV) and ultimately serves as the basis for the development of MVI and chronic heart failure (CHF) [1, 14, 17]. These disorders occur in a number of nosological forms and symptom complexes (Barlow, Marfan, Ehlers-Danlos syndrome, etc.).The main cause of MV ischemic insufficiency is dysfunction of the papillary muscles and myocardium due to coronary artery disease - it also disrupts the normal cooptation of the valves and aggravates MVI. Therefore, the main method of treating ischemic MV insufficiency is myocardial revascularization and restrictive annuloplasty [1-2, 6, 17].Fundamentally different pathophysiological mechanisms develop in the presence of valve dysplasia. These changes may be due to genetic factors or can develop against the background of acquired fibroelastic insufficiency of the connective tissue [5, 18, 21]. The development of insufficiency is often caused by an excess amount of the valves tissue, the formation of peculiar "hoods" on the free edges. There is often a prolapse of the anterior or both valves [5, 19]. Another cause of MVI is infectious endocarditis. The basis of the pathophysiological mechanisms is the formation of vegetations [3]. Vegetations are formed at the site of the pathogen adhesion — the areas of the damaged endocardium in the zones of turbulent or slow blood flow [4, 6]. The development of severe MVI with symptoms of circulatory failure, vegetations up to 1 cm or more, fibrous ring abscesses and the ineffectiveness of conservative therapy are indications for surgical treatment [7, 16]. According to the literary data, etiological cause of MI development in Europe and the United States are: connective tissue dysplasia (29-60%), coronary heart disease (CHD) (11-27%), idiopathic chord rupture (1-14%), infective endocarditis (2- 10%) [9, 12, 20]. Treatment experience of mitral insufficiency in the Republican Specialized Scientific and Practical Medical Center of Surgery named after academic V.Vakhidov revealed the following structure of etiological causes in Uzbekistan: infective endocarditis - 32.6%, myxomatous degeneration - 30.3%, rheumatism - 27%, IHD - 6.7%, injury - 3.4% [1, 5-6, 21, 23]. It is advisable to distinguish 2 main groups among the surgical methods of treatment: prosthetics of MV by mechanical or biological artificial prosthesis and reconstructive interventions. The use of mechanical prostheses has several disadvantages, first of all - thromboembolic complications. In many ways, the use of biological artificial heart valves helps to solve this problem, but today they have a limited lifespan (10-15 years). All these difficulties determined the continuous search of the ways for efficient reconstruction of MV in its insufficiency. The “revolution” in reconstructive surgery of MV was the work of the French cardiac surgeon A. Carpentier who is rightfully considered the “father” of MV reconstruction. He was the first to propose a technique for implantation of so-called support rings for annuloplasty of the fibrous ring. Among all degenerative forms of MVI, from the current point of view, it is customary to distinguish 2 large groups: Barlow syndrome and fibroelastic failure [6, 13]. The main techniques for reconstruction of the anterior cusp prolapse proposed by different authors in different years are chord shortening [8, 11, 20], transposition of chords and papillary muscles, the use of large support rings and, finally, chord prosthetics with artificial polytetrafluoroethylene (PTFE) threads. The use of a support ring is the main factor determining the quality of long-term results [14, 22]. Reports of non-implantation methods of MV reconstruction are still found in the literature [4, 17-18], but they are fragmented and controversial while most researchers focus on the crucial role of the ring proposed by Carpentier [10, 15, 19]. The necessity for surgical correction of MVI of III degree and above is not in doubt, but the justification for interventions on the mitral valve in case of insufficiency of II degree is still controversial [1, 4, 16]. Calafiore A.M. et al. demonstrated that the presence of even moderate mitral valve insufficiency reduces long-term survival rates of patients [11]. According to Zheleznev S.I. et al. [4], despite the excellent immediate surgical treatment results of severe MI of degenerative genesis, in the late postoperative period there is a return of significant (≥2nd degree) of mitral regurgitation and / or stenosis (peak gradient > 10 mmHg) of mitral valve. Thus, the 5-year freedom from stenosis according to Chung C.H et al. [13] was only 65.1 ± 10.7%.Thanks to new technologies and knowledge mitral valve reconstruction is feasible in the majority of patients. Thus, in the leading world centers, the developed original methods of surgeries allow to save the native valve in 90–100% of cases [11, 18, 20, 22]. So, today the number of patients with connective tissue dysplasia has significantly increased. The use of various mitral valve reconstruction techniques makes it possible to abandon the use of artificial heart valves which have many prosthetic-dependent complications.
2. Material and Methods
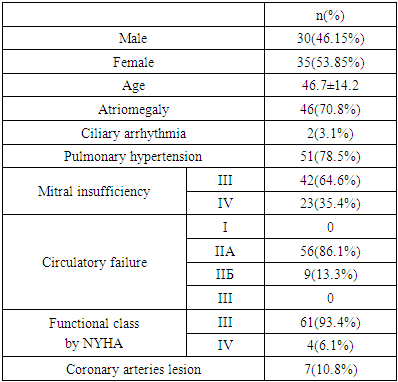
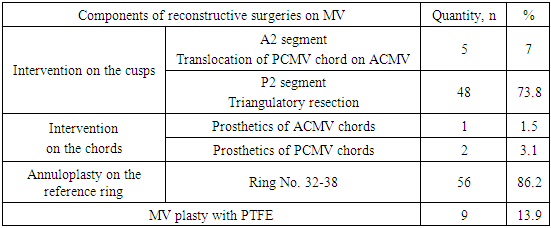
- 65 surgeries in patients with mitral insufficiency of III-IV degree at the age of 18 and 65 years (mean age 46.7 ± 14.2 years) were performed in the Department of Combined Heart Disease Surgery between October 2012 and April 2017. In total, 30 (46.15%) men and 35 (53.85%) women were operated on. The age of patients ranged from 18 to 65 years (mean age – 46.7 ± 14.2 years).The etiological causes of mitral insufficiency were as follows:• myxomatous degeneration - 45 (69.2%)• infective endocarditis - 9 (13.8%)• chord separation - 3 (4.6%)• ischemic dysfunction of the left ventricle - 7 (10.8%)• relative mitral valve insufficiency at aortic defect - 1 (1.5%).To assess the initial severity and severity of the defect the following indicators were evaluated - circulatory failure stage, NYHA functional class, mitral insufficiency according to echocardiography, presence of pulmonary hypertension, atriomegaly. The majority of patients - 61 (93.4%) were operated on in the third NYHA functional class, the remaining 4 (6.1%) were in the fourth functional class; circulatory failure of stage IIA was observed in 56 (86.1%) patients, circulatory failure of stage IIB was observed in 9 (13.8%) patients (Tab.1). Transthoracic echocardiography (EchoCG) was performed in all patients in the pre- and postoperative period. Transesophageal echocardiography was used during the surgery. Mitral insufficiency of III degree was noted in 64.6% of cases, severe (IV degree) in 35.4% of patients. Atriomegaly was observed in 46 (70.8%) patients. The average size of the left atrium was 6.7 ± 1.2 cm. Pulmonary hypertension was diagnosed in 51 (78.5%) cases. According to ECG data 63 (96.9%) patients had sinus rhythm, only 2 (3.1%) cases had ciliary arrhythmia. In 43 (66.2%) patients we revealed the signs of LV hypertrophy. In 7 (10.8%) patients there was insufficiency of the coronary circulation of the anterolateral and apical wall of the left ventricle. 59 (90.8%) patients had left atrial and left ventricular hypertrophy with overload. Coronary angiographic studies were performed in men after 40 years and in women after 45 years. In 7 (10.8%) patients lesions of the coronary arteries were detected. Two of them had a three-vessel and two had a two-vessel lesions. In one case occlusion of anterior interventricular branch (AIVB) was observed. The remaining 2 patients had critical stenoses (1 stenosis of the anterior interventricular branch (AIVB), 1 stenosis of the blunt edge branch).
|
|
3. Results and Discussions
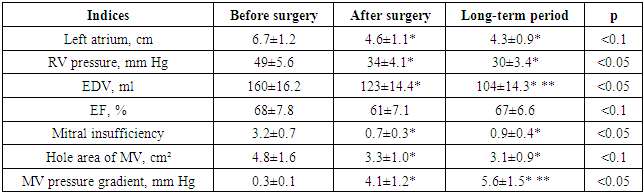
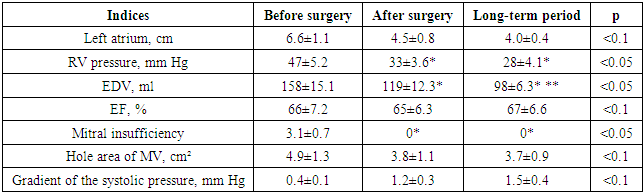
- To assess the immediate results, the patients were divided into 2 groups: Group I - 56 (84.4%) patients who underwent resection of the prolapse site or the creation of a neocord or chord translocation with implantation of a Carpentier support ring of different sizes depending on the diameter of the fibrous ring; Group II - 9 (13.8%) patients who underwent resection of the prolapse site with strengthening the size of the fibrous ring of the posterior cusp of the mitral valve by using a strip of synthetic prosthesis (PTFE). When evaluating the immediate results of operations, the following criteria were taken into account: the patient's objective condition, the need for inotropic hemodynamic support, analysis of ECG observations, EchoCG — the size of the heart chambers, the work of the left ventricle, the frequency and nature of complications in the immediate postoperative period, analysis of the frequency and structure of mortality. In group I where MV plasty was made by Carpentier using an artificial rigid support ring, the average duration of cardiopulmonary bypass was 65.2 ± 12.4 minutes, the aortic clamping time was 49.0 ± 8.3 min. In group II - 58.2 ± 10.9 min and 43.0 ± 7.4 min respectively. The time of cardiopulmonary bypass and aortic clamping when using a support ring or strips of PTFE did not significantly differ. In group I the average time of patients stay in the intensive care unit was 18.7 ± 1.5 hours. The resuscitation period in patients without catecholamine support did not exceed 1 day. Patients of group I had no lethal outcomes at the hospital stage. However, there were various complications in the early postoperative period. We divided these complications into cardiac (cardiovascular insufficiency, heart rhythm disturbances) and non-cardiac (pneumonia, sepsis, purulent mediastinitis, complications from the central nervous system (CNS) site). In 21 (37.5%) patients rhythm disturbances were observed in the form of paroxysms of ciliary arrhythmia which were treated with medication. In 2 (3.6%) patients with the initial form of ciliary arrhythmia after surgery we managed to restore the sinus rhythm. Ischemic genesis of mitral valve insufficiency was observed in 7 (12.5%) patients of group I who underwent simultaneous mitral valve repair with coronary artery bypass surgery. In the same category of patients in the early postoperative period, signs of myocardial weakness were observed which required prolonged artificial lungs ventilation and prolonged infusion of inotropic drugs (dopamine, adrenaline, dobutamine). The resuscitation period in these patients averaged 54 ± 1.6 hours. The cause of the heart failure development in the early postoperative period in this category of patients can be explained by the initial severity of the condition (low left ventricular ejection fraction - 38 ± 2.4%, EDV - 236 ± 23.8 ml, EF - stage III-IV). A positive echocardiographic result was observed 3-4 days after correction of MV deficiency (Tab.3). The end diastolic volume (EDV) significantly decreased (before / surgery (b\s) 160 ± 16.2 ml; after / surgery(a\s) 123 ± 14.4 ml), pressure in RV (b\s 49 ± 5.6 mm Hg; a\s 34 ± 4.1 mm Hg), the degree of mitral insufficiency (b\s 3.2 ± 0.7; a\s 0.7 ± 0.3). It should be noted that a decrease of pressure in the RV and EDV in the postoperative period was detected in all patients. The pressure gradient of the mitral valve significantly increased due to restrictive annuloplasty. In the early postoperative period after plasty of MV on the support ring, the average pressure gradient did not exceed 4.1 ± 1.5 mm Hg. Residual insufficiency of the mitral valve of I degree after plastic surgery on MV was noted in 5 (8.9%) cases. In 5 (8.9%) patients of group I non-cardiac complications were noted. An X-ray examination in 3 patients (5.4%) at the hospital stage revealed hydrothorax which was cured by evacuation of up to 500 ml of serous hemorrhagic fluid. Complications of the postoperative wound were observed in 2 patients in the form of the sternum diastasis. They were performed a second operation - sternoplasty. There were no complications of the central nervous system.In one patient of group I the plasty was found to be unsatisfactory during the hospital period due to the eruption of the seams and the dislocation of the rigid support ring in the early postoperative period. The patient was re-operated: the reference ring was removed, mitral valve replacement was performed. At the time of discharge the general condition of all patients improved significantly. 83.5% of patients were classified as NYHA functional class I, 16.5% - as class II. Thus, the immediate results of operations in group I showed quite good efficiency. 9 patients of II group underwent resection of the prolapse site using a PTFE strip. The mitral insufficiency of ischemic genesis was not noted in them. Lethal outcomes were not observed in the early postoperative period. However, the following complications occurred: 3 (33%) patients had heart rhythm disturbances, in all cases it was possible to restore sinus rhythm. No non-cardiac complications were noted among patients. In all patients of this group we noted a decrease in the size of the left atrium (b \ s 6.6 ± 1.1 cm, a \ s 4.5 ± 0.8 cm), EDV (b \ s 158 ± 15,1 ml, a \ s 119 ± 12.3 ml), pressure in the right ventricle (b \ s 47 ± 5.2 mm Hg, a \ s 33 ± 3.6 mm Hg), there was no regurgitation. The average pressure gradient on the MV after the surgery did not exceed 1.2 ± 0.3 mm Hg. Immediate postoperative changes in hemodynamics of the left ventricle in comparison with the preoperative data are presented in the Table 4.
|
|
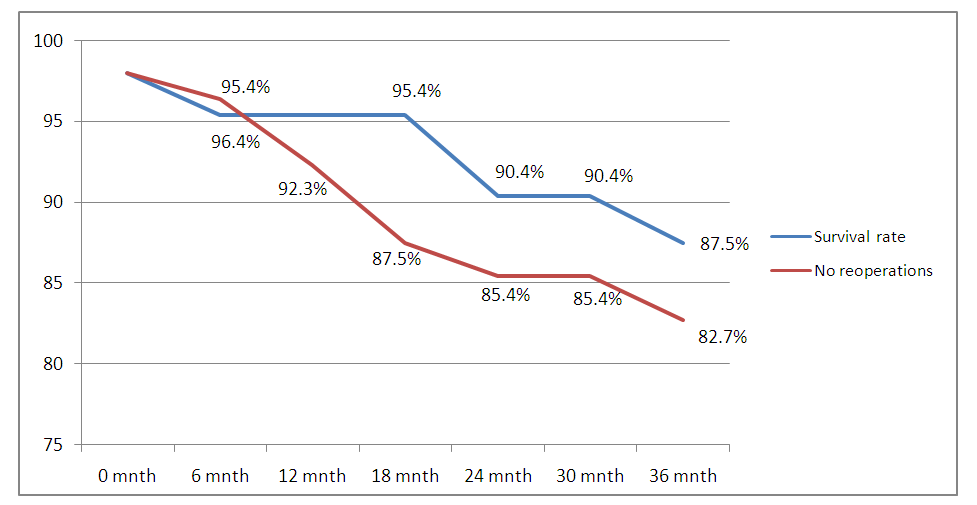 | Figure 1. Dynamics of survival and freedom from reoperations |
4. Conclusions
- Mitral valve plasty on the “PTFE” strips and “Carpentier” rings showed its high efficiency, while retaining the natural configuration, architecture and mobility of the fibrous ring of the mitral valve. The "PTFE" strip has a number of undeniable advantages: strength combined with optimal plasticity make it handle and safe. The "PTFE" strip does not require special material equipment, does not cause any pathological deviations in the patient's body. These patients are free from taking anticoagulants, free from complications associated with mechanical prosthetic heart valves. It is advisable to perform valvuloplasty techniques with the mandatory implantation of a rigid support ring for prolapses of the anterior cusp and both cusps of the mitral valve with dilatation of the left ventricular cavity. At an isolated prolapse of the central part of the posterior cusp (zone P2) it is possible to perform resection techniques of valvuloplasty using a strip of synthetic teflon prosthesis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML