-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(5): 170-173
doi:10.5923/j.ajmms.20190905.03

Clinical and Anamnestic and Laboratory Criteria for Diagnostic Pre-Thrombotic Conditions in Patients with Hemostasiopathy
Aziza Dzhumanovna Makhmudova1, Inna Viktorovna Berger2, Nigora Abduvalievna Tursunova3, Lola Valievna Ashurova1
1Administration, Scientific-Research Institute of Hematology and Blood Transfusion of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
2Research Department, Scientific-Research Institute of Hematology and Blood Transfusion of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
3Day Stay Department, Scientific-Research Institute of Hematology and Blood Transfusion of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
Correspondence to: Inna Viktorovna Berger, Research Department, Scientific-Research Institute of Hematology and Blood Transfusion of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The Hematology Research Institute examined patients with thrombophilia, determined the frequency and nature of violations in different parts of the hemostasis system. Clinical, anamnestic and laboratory criteria for the diagnosis of prethrombotic conditions in patients with chronic melastoplastic disease (CMD) have been established. Studies were conducted on the basis of a study of hemostasiogram data, as well as studies of Protein C, lupus anticoagulant and D-dimer. Studies have shown and confirm that violations in different parts of the hemostasis system for CMD are frequent and are characterized not only by vascular and platelet, but also deep plasma disorders.
Keywords: Thrombophilia, Thrombotic complications, Hemostasis, Hypercoagulation
Cite this paper: Aziza Dzhumanovna Makhmudova, Inna Viktorovna Berger, Nigora Abduvalievna Tursunova, Lola Valievna Ashurova, Clinical and Anamnestic and Laboratory Criteria for Diagnostic Pre-Thrombotic Conditions in Patients with Hemostasiopathy, American Journal of Medicine and Medical Sciences, Vol. 9 No. 5, 2019, pp. 170-173. doi: 10.5923/j.ajmms.20190905.03.
Article Outline
1. Introduction
- Pre-thrombotic state (thrombophilia, hypercoagulability) is a condition of increased blood clotting resulting from changes in one or several hemostatic components - platelets (thrombocytosis, increased platelet function), coagulation factors (increased content of prothrombin, fibrinogen), fibrinolysis factors (decrease in plasma levels). Its activators, an increase in the activity of inhibitors), vascular wall factors (decrease in the synthesis of prostacyclin, a decrease in the activity of the active plasminogen ator) [1]. Often, instead of the term “prethrombotic state”, the term “thrombophilia” is used [4, 5].According to some foreign studies, thrombophilia, in this variant in hematological patients is acquired and detected in more than 40% of patients. Most often, thrombogenic risk factors in patients with the above pathologies include genetic abnormalities as well as individual characteristics of the organism [2]. It has been established that if a patient’s age exceeds 45 years, the risk of a thrombotic state increases by another 25% and may lead to the development of thrombotic readiness [2]. Thrombophilic conditions are clinically manifested in the form of venous thrombosis, thromboembolism, ischemia, infarction of various organs, strokes, pulmonary thromboembolism, which inevitably can be fatal [3].The study of blood coagulation and thrombosis, the value of each phase of hemocoagulation and fibrosis during the formation of a prethrombotic state will significantly increase the number of indicators for its diagnosis, which can be grouped as follows: 1) the results obtained using instrumental methods (thromboelasto and electrocoagulography); 2) total blood coagulation activity (blood clotting time, heparin tolerance, recalcination time); 3) functional properties of platelets (adhesion and aggregation) and erythrocytes; 4) fibrinogen and products of its transformation and degradation; 5) stabilizing fibrin factor; 6) anticoagulant activity (antithrombins, especially antithrombin III, heparin, their inhibitors); 7) total fibrinolytic activity of blood and fibrinolysis inhibitors; 8) antithrombogenic properties of the vascular wall. [four].
2. Main Body
2.1. The Purpose of Our Research
- Establish clinical-anamnestic and laboratory criteria for the diagnosis of pre-thrombotic conditions in patients with CMP (chronic myeloproliferative diseases).
2.2. Material and Methods of Study
- In the research work used the blood and plasma of patients suffering from CMD. The control group consisted of 20 healthy donors. All persons in the control group conducted a study of the parameters of the blood coagulation system used in the work.When studying prethrombotic conditions in hematological patients who are hospitalized at Scientific Research Institute of Hematology and Blood Transfusion of the Ministry of Health of the Republic of Uzbekistan (SRI of H and BT) for 2016-2017, it was found that they occur in pathologies such as: chronic myeloid leukemia (250 patients), erythremia (68 patients), subleukemic myelosis (49 patients), multiple myeloma (413 patients), Waldenstrom's disease (30 patients), chronic megakaryocytic leukemia (23 patients), as well as vasculitis (69 patients). In total, 902 patients with these pathologies were registered for 2017, which is significantly more than in 2015 (850) and 2014 (835 patients).
2.3. Results of the Study
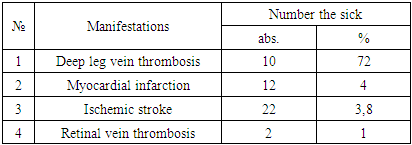
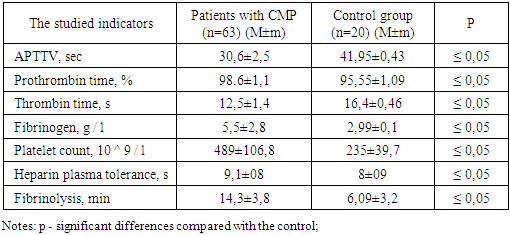
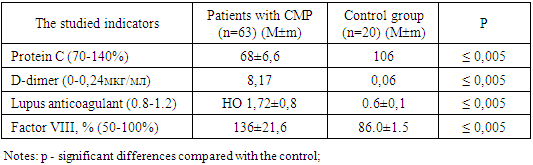
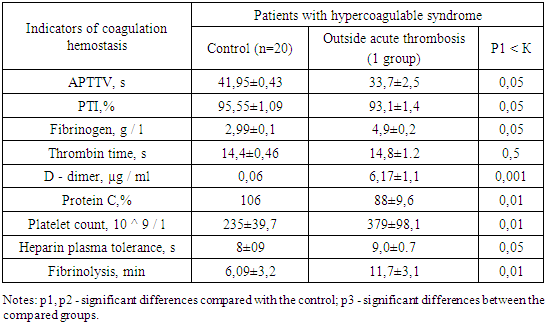
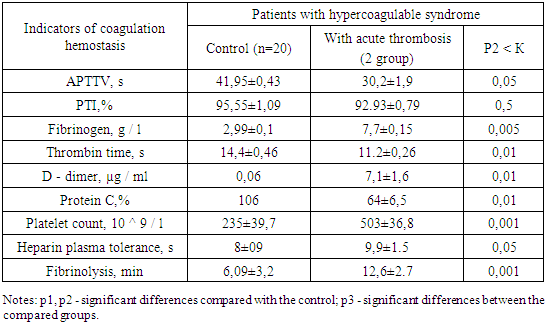
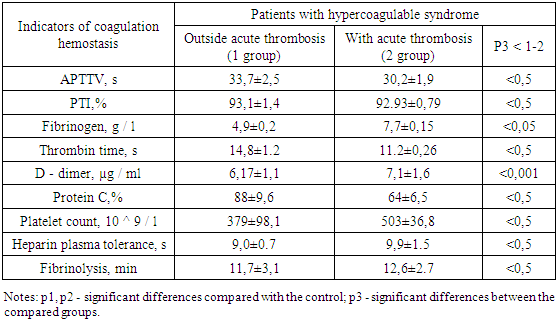
- During the period of 2018, a comprehensive clinical and laboratory examination of 63 patients suffering from CMP (48 men and 15 women) aged from 18 to 62 years was conducted. Of them: 42 patients with Multiple myeloma, 13 - with Erythremia, 8 - with chronic myeloid leukemia. Signs of thrombophilia confirmed by clinical and laboratory studies were found in 13 patients from the examined (21%) patients. The diagnosis of myeloproliferative diseases was established on the basis of clinical symptoms, laboratory tests, and cytological and immunohistochemical studies of the bone marrow.Signs of thrombophilia confirmed by clinical and laboratory studies were found in 13 patients from the examined (21%) patients. All examined patients with suspected thrombophilia are tested for D-dimer, Protein C and lupus anticoagulant, the level of factor VIII previously not included in the examination algorithm.The incidence of thrombosis in patients with nosological groups of myeloproliferative diseases (n = 54) was determined by collecting anamnestic data, and the incidence of the hypercoagulative syndrome and localization of thrombosis were determined with the calculation of the percentage of localization occurrence (Table 1), so in 72% of cases deep venous thrombosis was detected. tibia, 4% myocardial infarction, 3.8% ischemic stroke, retinal vein thrombosis was recorded in 1% of cases (confirmed by ophthalmoscopy).
|
|
|
|
|
|
3. Conclusions
- Based on clinical and laboratory studies, the frequency and nature of violations in different parts of the hemostasis system in a group of patients with CMD were determined. As part of the problem of high growth in the number of patients with thrombophilic complications, further study of this condition is necessary, which makes knowledge of clinical features and algorithms particularly important. Patients have a state of increased blood clotting due to changes in one or more components of hemostasis - platelets (thrombocytosis, increased functional activity of platelets), blood coagulation factors (increased prothrombin content, fibrinogen), fibrinolysis factors (reduced content of plasminogen and its activators, increased inhibitors), vascular wall factors (reduced synthesis of prostacyclin, reduced activity of plasminogen activators) in persons suffering from CMD.In contrast to the control group of comparison, which has the same age characteristics, there were no changes in the hemostasis system and no patients had any changes indicating the onset of thrombosis. Thus, our studies show and confirm that violations in different parts of the hemostasis system in CMD are frequent and are characterized not only by vascular and platelet, but also deep plasma disorders.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML