-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(5): 167-169
doi:10.5923/j.ajmms.20190905.02

Risk Factors for Protracted Community-Acquired Pneumonia in Children
Khaydarova Sarvinoz Khaydarjonovna
Basic PhD Doctorate 2 years at the Department of Pediatrics, Samarkand State Medical Institute, Uzbekistan
Correspondence to: Khaydarova Sarvinoz Khaydarjonovna, Basic PhD Doctorate 2 years at the Department of Pediatrics, Samarkand State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance of the research problem: Pneumonia is an acute infectious disease, predominantly of bacterial etiology, characterized by a focal lesion of the respiratory departments of the lungs, the presence of intra-alveolar exudation detected by physical and instrumental examination, and a febrile reaction and intoxication expressed in varying degrees. Objective: Identify factors that have prognostic value in the formation of a protracted course of community-acquired pneumonia in children. Materials and methods: The results of a retrospective analysis of 6790 histories of treated patients with bronchopulmonary pathology at the clinic in Samarkand for the period 2015-2017, as well as the results of a prospective study of 100 patients with CAP aged from 6 months to 15 years who were admitted to inpatient treatment at the Department of Pulmonology of the Republican Specialized Scientific and Practical Medical Center of Pediatrics and Samarkand State Medical Institute. Results of the study: In a retrospective analysis of 6790 case histories of children with bronchopulmonary diseases treated in Samarkand, 63.3% of children had community-acquired pneumonia. It should be noted that radiological confirmation of pneumonia was noted only in case histories of 64.6% of patients. It shows that 35.4% had overdiagnosis of community-acquired pneumonia. Conclusions: Based on a retrospective analysis, it was revealed that general practitioners have overdiagnosis of community-acquired pneumonia and incorrect management of antibiotic therapy, and this in turn leads to a prolonged course of the process in the lungs.
Keywords: Pneumonia, C-reactive protein, Procalcitonin, Overdiagnosis, Diseases of the bronchi and lungs
Cite this paper: Khaydarova Sarvinoz Khaydarjonovna, Risk Factors for Protracted Community-Acquired Pneumonia in Children, American Journal of Medicine and Medical Sciences, Vol. 9 No. 5, 2019, pp. 167-169. doi: 10.5923/j.ajmms.20190905.02.
Article Outline
1. Relevance of the Research Problem
- Pneumonia is an acute infectious disease, predominantly of bacterial etiology, characterized by a focal lesion of the respiratory departments of the lungs, the presence of intra-alveolar exudation detected by physical and instrumental examination, and a febrile reaction and intoxication expressed in varying degrees [2, 6]. Due to the success of recent years, achieved in the diagnosis and treatment of community-acquired pneumonia (CAP) in children, the course of the disease has changed, the number of severe forms of the disease has decreased, and the mortality rate has decreased [1, 8]. However, the urgency of the problem of pneumonia remains, the prevalence of the disease is still quite high, and despite the fact that the CAP is usually attributed to controlled diseases, mortality is recorded annually. In recent years, cases of prolonged pneumonia have increased, which is caused by atypical pathogens and the ineffectiveness of antibacterial therapy [2, 4, 7].With prolonged remission of pneumonia, the pneumonic infiltrate is absorbed slowly, over an extended period of time (from above 4-6 weeks). About 30% of acute pneumonia take a protracted nature of the flow. The reasons for this may be chronic intoxication or a weakened state of the body, irrational antibiotic therapy, a concomitant violation of the drainage function of the bronchi, prematurity and a complicated course of acute pneumonia. However, in the practice of the pediatrician, there are frequent cases of misinterpretation of clinical symptoms in terms of determining the variant of CAP (typical or caused by atypical flora) and the associated erroneous starting antibacterial therapy [3-5].The inflammatory biomarkers include procalcitonin and C-reactive protein, the study of which in the diagnosis of bronchopulmonary diseases in children is a promising direction. Studying the possibility of using these biomarkers of inflammation to predict the course of the disease will be a promising scientific direction.
2. Objective
- Identify factors that have prognostic value in the formation of a protracted course of community-acquired pneumonia in children.
3. Materials and Methods
- The results of a retrospective analysis of 6790 histories of treated patients with bronchopulmonary pathology at the clinic in Samarkand for the period 2015-2017 y, as well as the results of a prospective study of 100 patients with CAP aged from 6 months to 15 years who were admitted to inpatient treatment at the Department of Pulmonology of the Republican Specialized Scientific and Practical Medical Center of Pediatrics and Samarkand State Medical Institute.C-reactive protein (CRP) in the blood serum was determined in an automatic analyzer immunohemilyuminestsentnom Immulite 2000 (Siemens, Germany). Determination of the concentration of procalcitonin (PCT) in the serum was performed on an Advia Centaur automatic immuno-chemiluminescent analyzer (Siemens, Germany). The data were processed by the method of variation statistics Fisher - Student using personal computers and use of the application package.
4. Results of the Study
- In a retrospective analysis of 6790 case histories of children with bronchopulmonary diseases treated in Samarkand, 63.3% of children had community-acquired pneumonia. It should be noted that radiological confirmation of pneumonia was noted only in case histories of 64.6% of patients. It shows that 35.4% had overdiagnosis CAP. The subjective error in the appointment of the starting antibiotic is the wrong choice of the drug in 21.2% of cases. Advantageously administered antibiotics penicillin, and 45% of the starting preparation was ceftriaxone. At 12.0% conducted unreasonably repeated courses of treatment and further a second aminoglycoside antibiotic. Moreover, amikacin was prescribed more often in 40.0% of cases. Schemes with the appointment of a combination of cefazolin and amikacin in 9.5% of children are also defined as inadequate: excessive prescription of 1st generation cephalosporin.In the analysis of 7397 case histories of children treated in the Samarkand region for the period 2015 - 2017. at 35.9% it was found CAP. As a result of the analysis, overdiagnosis of CAP was found in 13.8% of children. Irrational use of antibacterial drugs in children treated in hospitals reaches 15.5% of cases. In all cases, there was an empirical choice of starting antibiotic therapy: therapy began without taking into account the sensitivity of pathogens to antibiotics. Inadequate use of cephalosporins 1st generation in the appointment, which is not necessary, have a narrow spectrum of activity and a low level of activity against bacteria and further the problem of growth of antibiotic resistance.In the analysis of 6426 case histories of children treated in the Samarkand region for the period 2015-2017. 45.5% had CAP. As a result of the analysis, overdiagnosis of CAP was revealed in 15% of children. The subjective error in the appointment of the starting antibiotic is the wrong choice of the drug in 15.3% of cases. The main causes of overdiagnosis of CAP are underestimation of the history and incorrect interpretation of radiological and laboratory data, as well as unreasonable use of antibiotics, leading to a prolonged course of the process in the lungs. The content of CRP increases in serum during inflammation (infectious diseases). Normal concentration of CRP in serum does not exceed 8 mg / l. In a prospective study, out of 35 examined CAP patients in the initial period of the disease, 28.6% (10) had an increased CRP level in blood serum, and 71.4% (25) children had it within the normal range (fig. 1).
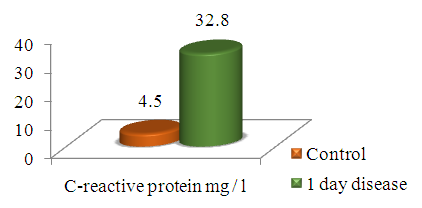 | Figure 1. Indicators of C-reactive protein in children with CAP, M±m |
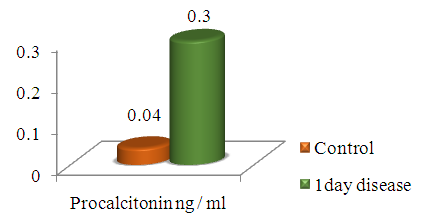 | Figure 2. Indicators of procalcitonin in children with CAP, M ± m |
5. Conclusions
- 1. Based on a retrospective analysis, it was revealed that general practitioners have overdiagnosis of community-acquired pneumonia and incorrect management of antibiotic therapy, and this in turn leads to a prolonged course of the process in the lungs. 2. Evaluation of biomarkers of inflammation C-reactive protein and procalcitonin is an informative indicator in the diagnosis of community-acquired pneumonia in children, their increase is confirmed by the bacterial nature of the pathological process, which can be used when choosing differentiated therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML