-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(4): 143-145
doi:10.5923/j.ajmms.20190904.02

The State of Blood Coagulation System in HIV Infection in Children
Daminov T. A., Tuychiev L. N., Khudaykulova G. K., Rakhmatullaeva Sh. B.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The problem of HIV infection in childhood is currently the most relevant because of the increase in the number of pregnant HIV-positive women. One of the manifestations of HIV infection in childhood are the changes in the system of hemostasis, manifested by a decrease in the aggregation capacity of platelets, detected at the initial stages of the disease with normal blood platelet levels and PTI.
Keywords: HIV infection, Coagulogram, Platelets
Cite this paper: Daminov T. A., Tuychiev L. N., Khudaykulova G. K., Rakhmatullaeva Sh. B., The State of Blood Coagulation System in HIV Infection in Children, American Journal of Medicine and Medical Sciences, Vol. 9 No. 4, 2019, pp. 143-145. doi: 10.5923/j.ajmms.20190904.02.
Article Outline
1. Introduction
- Currently, HIV infection in children is one of the most urgent problems in the world. One of the typical manifestations of the impact of HIV infection on the child's body are hemostatic disorders that lead to severe life-threatening complications [1, 4, 11].HIV directly affects megakaryocytes, platelets, and vascular endothelium at the stage of acute HIV infection and may play a role at the stage of pronounced clinical manifestations of the disease when the maximum concentration of HIV RNA is recorded in the blood of patients [6].At the stage of asymptomatic HIV infection, disorders in the hemocoagulation system are primarily associated with changes in the immune system.At the stage of accession of secondary diseases in the genesis of hemostasis disorders in patients with HIV infection, most authors identify several factors: the direct effect of HIV on blood cells and bone marrow, mediated through changes in the immune system, as well as the effect of secondary diseases and drugs [5, 6].It is noted that the severity of disorders in the hemocoagulation system increases in accordance with the progression of HIV infection [6, 11].A striking manifestation of vascular-platelet disorders is the development of chronic immunological thrombocytopenic purpura (ITP), which can be diagnosed both at the onset of the disease and at the AIDS stage (Schneider PA, Abrams DI, Rayner AA, Hohn DC Immunodefi ciency associated thrombocytopenic purpure (IDTP) ) // Arch. Surg. - 1997. - 122. - P. 1175-1178).According to most authors (Vasilyev SA, Berkovsky A.L., Antonova O.A., Mazurov A.V. Thrombocytopenia: pathogenesis, differential diagnosis and the basis of therapy. Thrombosis, hemostasis and rheology. - 2000. - №4 - C.6-15), mechanisms of thrombocytopenia can be associated with enhanced peripheral destruction of platelets and ineffective thrombopoiesis (due to impaired production and release of platelets) [2, 5].Obviously, the spectrum of the pathology of the hemostasis system in HIV infection is very wide and for detailed study it requires an in-depth approach to researching the production and life cycle of platelets, the CIC level, the content of blood coagulation factors and anticoagulants, as well as autoantibodies, depending on the clinical manifestations and the timing of the disease.Thus, the effect of the immunodeficiency virus on the child’s body contributes to the development of complex disorders in both the coagulation and anticoagulation mechanisms of the blood. When examining patients with HIV infection, it is necessary to evaluate both the platelet component and the enzymatic component; as well as integrative methods, allowing to judge about all components of the hemostasis system in their interaction.In this regard, it is important to study the changes in coagulogram in children with HIV infection.The aim of the work is to study coagulogram parameters in children with HIV infection in different clinical stages.
2. Materials and Methods
- For the period from 2015 to 2017, the study included 89 children aged 4 to 16 years. The children were under medical supervision in the AIDS Centre of the Tashkent city. The diagnosis was established on the basis of clinical and laboratory data in accordance with the order of the Ministry of Health No.81 dated 5.03.2015 (according to WHO proltokol). The average age of patients was 9.8±0.49 years. 61.8% were boys and 38.2% were girls of the children included in the study.The patients were divided into 3 groups depending on clinical stage of HIV infection: clinical stage II - in 17 patients (group 1); clinical stage III– in 62 patients (group 2); IV clinical stage – in 10 patients (group 3). Patients with clinical stage I were not included, because their number is not enough to obtain reliable data. A control group (norm) was also formed, which included 25 healthy volunteers of the same age.Coagulogram analysis included the determination of the following parameters: platelet count, platelet aggregation (adenosine diphosphate (ADP) 1 mmol), activated partial thromboplastin time (APTT), prothrombin index (PTI), thrombin time, plasma fibrinogen, CN-a dependent fibrinolysis, orthophenanthroline test. Prothrombin index was determined by Quique, plasma fibrinogen - by Klaus. Platelet aggregation according to the method of Born on the optical analyzer of platelet aggregation. APTT, thrombin time is a standardized screening methods.Statistical processing of the results of the study was carried out using the methods of parametric and nonparametric statistics using STATISTICA 5 computer program.Statistical processing of the material included the calculation of absolute and relative values, average values (M).In the description of quantitative indicators minimum and maximum value, the average value, taking into account the error of deviation (m) were used. Absolute and relative frequencies (in %) were calculated for qualitative indicators.The criterion of statistical reliability of the findings was considered to be the generally accepted value P≤0.05.
3. Results of the Study
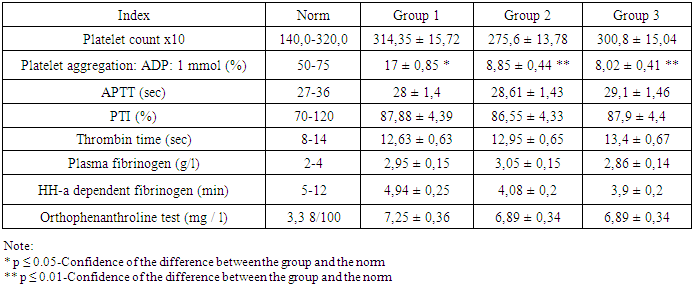
- Analysis of the results showed the following changes (table.1).
|
4. Discussion
- Platelet dysfunction, according to the results of the study, was to reduce the platelet aggregation ability detected from the first clinical stages of HIV infection [1, 4, 6].This may be due to the weakening of platelet adhesion-aggregation and retractile properties caused by virus replication in bone marrow cells or their presence in platelets [8].It is assumed that viruses can affect the antigenic structure of platelets, changing it, not only due to interaction with membrane proteins, but also as a result of nonspecific fixation on the surface of platelets.In turn, this leads, firstly, to the development of antibodies against altered platelet antigens, and secondly, to the interaction of antiviral antibodies with viral proteins, which are fixed on the platelet surface [1, 4, 11].
5. Conclusions
- Deviations in the coagulogram in children of different clinical stages of HIV infection are represented by a decrease in the aggregation ability of platelets, detected at the initial stages of the disease.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML