-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(3): 104-107
doi:10.5923/j.ajmms.20190903.07

Condition of the Immune System in Patients with Various Variants of Cephalgia in an Interictal Period
Durdona Abdullajonovna Alijanova, Yakutkhan Nabiyavna Madjidova
Neurological Diseases, Children's Nervous Diseases, Medical Genetics, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

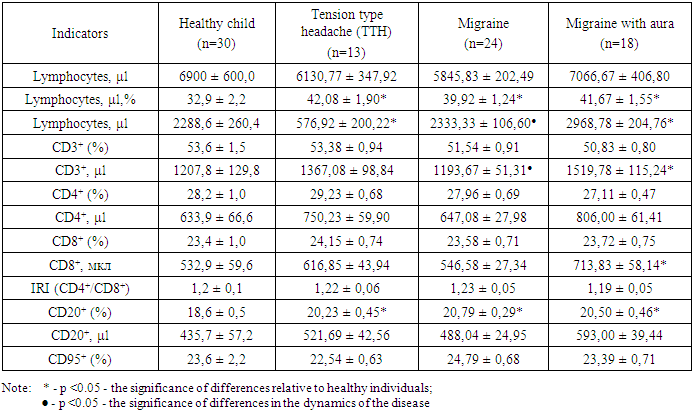
The aim of the present study was to analyze the neurological and immunological aspects of a headache in children. Were examined 24 children with simple migraine, 18 children with migraine with aura and 13 children with tension type headache, with determining the number of circulating T-lymphocytes (CD3+) and their main immune regulating subpopulations of T-helper and T-cytotoxic cells (CD4+, CD8+), B lymphocytes (CD20+), immune regulatory index (IRI), marker of apoptosis (CD95+) in the inter attack period, with remission of somatic diseases. As a result of a comparative analysis of the obtained indicators of the immune system in patients, there was no significant deviation in the cellular immunity parameters relative to control values, which indicates that they have immune homeostasis in the inter attack period.
Keywords: A headache, Migraine, Children, Immunology, Cellular immunity
Cite this paper: Durdona Abdullajonovna Alijanova, Yakutkhan Nabiyavna Madjidova, Condition of the Immune System in Patients with Various Variants of Cephalgia in an Interictal Period, American Journal of Medicine and Medical Sciences, Vol. 9 No. 3, 2019, pp. 104-107. doi: 10.5923/j.ajmms.20190903.07.
Article Outline
1. Introduction
- The problem of a headache in modern neurology remains one of the leading ones [1, 2]. Headache is also one of the most frequent complaints of child age, about which parents treat to the doctor. A wide range of diseases associated with headaches, the diversity of their clinical manifestations, the frequent persistence of the course reflects the urgency of the problem of headaches in pediatrics and neurology [3, 4]. The most frequent types of primary headaches are migraine and tension type headache (TTH) [5], and in 15% of patients, the first attacks occur before the age of 10 years [6].Despite the huge interest of domestic and foreign researchers in the changes of cellular and humoral immunity accompanying with various pathological conditions, immunological aspects of the pathogenesis of primary cephalgia (an autoimmune component, etc.) in literature practically not discussed, though the close interrelation of NMDA - receptors with immunological indicators is well known. In this regard studying of the immune status of patients with primary headaches is of considerable interest [7-11].The pathogenesis of cephalgia is complicated and not fully learned. Modern immunology is one of the most actively developing branches of science, continuously expanding its borders by introducing into various areas of clinical medicine [12]. It has been proved that the immune system is not limited to identifying and destroying foreign antigens, an increasingly strong position is taken by the idea of its ability to control non-immune functions of the body [13]. In this regard, a whole new direction has emerged, such as non-infectious immunology. However, the influence of the immune system on the development and progression of primary headaches is not fully understood what an important source of discussion.
2. Main Body
2.1. Purpose of the Study
- To study and determine the state of the immune system in patients with various types of cephalgia in the inter attack period.
2.2. Materials and Methods of Investigation
- Forty-two children with a diagnosis of a child migraine enrolled in a study. 24 children with simple migraine — girls 54.2% (13), boys 45.8% (11), respectively; 18 children with migraine with aura- girls 55.5% (10), boys 44.4% (8), respectively and 13 children diagnosed with tension type headache, 38.5% (5) were girls and 46.2% (6) boys. The average age of children was -12.44 ± 0.46.Based on anamnestic, clinical and neurological data, the third edition of the International Classification of Headache Disorders (ICHD-3) 2013 used for the diagnosis of a migraine. Additionally, the following paraclinical studies were carried out for the purpose of differential diagnosis: MRI, EEG, TCDG, and consultations with narrow specialists.The assessment of the immunological status was performed according to the recommendations of R.M. Khaitov [14] and 1-level tests for T-cell immunity in the following indicators: the number of circulating T-lymphocytes (CD3) and their main immune regulatory subpopulations of T-helper and T-cytotoxic cells (CD4, CD8), B-lymphocytes (CD20) using monoclonal antibodies, produced by the Research Institute of Immunology of the Ministry of Health of the Russian Federation (Moscow, “Sorbent” company) according to the method of Garib F.Yu. with co-authors [15]. Blood lymphocytes were analyzed in a group of 42 previously diagnosed childhood migraine patients and 13 children with a tension type headache. This is the cross-sectional analysis, which data collection performed in the morning, only in the inter attack period, with remission of somatic diseases.
2.3. Statistical Analysis
- Collected data were recorded into previously prepared forms, and the statistical analyses were performed with Statistical Package for the Social Sciences (SPSS) version 17.0 software package. Continuous values were presented as median and mean±standard deviation, where suitable. Fisher’s exact test were used to compare categorical variables among groups. The Mann–Whitney U test was used to compare nonparametric variables. The categorical values were presented as number and percentage. Statistical significance was set at p<0.05.
2.4. Results and Discussion
- According to anamnestic studies, 23% of children with a diagnosis of a migraine were diagnosed with a burdened perinatal history, with tension type headache (TTH) 6% of children, respectively. In 27% of children with a migraine, the hereditary nature of the disease was observed through the maternal line, whereas with a diagnosis of TTH, these figures were 4%. In 32% of children with a migraine, concomitant chronic somatic diseases of the ENT organs were detected, whereas in TTH this was 8% of children.During the clinical and neurological examination in the inter attack period, there were no gross focal symptoms, there was a diffuse micro symptomatology of a residual nature, in children with a migraine 26%, in TTH 11% of children; Symptoms of peripheral cervical insufficiency were observed in children with a migraine in 22% of cases, whereas in TTH in 4% of children. The most pronounced symptoms were vegetative disturbances in the form of hyperhidrosis of the palms and feet, meteolability, mood swings in the inter attack period in 28% of children with a migraine and in 9% of children with TTH.According to paraclinical studies on MRI of the brain, signs of angioencephalopathy were observed in 24% of the examined children with a diagnosis of a migraine, with TTH - in 8% of the children; 9% of children with a migraine had foci of demyelination, with TTH, the incidence was 2% of children and 57% of children did not show any pathological changes. EEG studies of the brain revealed dysfunction of the brainstem structures in 28% of children with a migraine, with TTH it was 9%, increased convulsive activity in 15% of patients with a migraine, with TTH 3%, respectively; diffuse changes in the brain were detected in 34% of children with a migraine, with TTH were 11%.Transcranial Doppler sonography of the head vessels revealed a lack of blood supply in the vertebrobasilar system in 48% of patients with a migraine, with TTH in 5% of children. The anomaly of vascular development was noted in 12% of children with a migraine, with TTH in 2% of children. In 16% of children with a migraine and in 17% of children with TTH, there were no pathological disorders in the blood supply.Based on the results of the study in a comparative aspect, conducted in a group of children with a diagnosis of migraine and tension headache, analysis of subjective and objective clinical and neurological parameters, along with the results of paraclinical studies (MRI, EEG, TCD), confirms the literature on the occurrence of headaches migraine pain with pathogenetic mechanisms of vascular genesis. Whereas in TTH, these studies cannot serve as reliable indicators of the connection of this nosology with a vascular genesis.The results of immunological studies: Baseline indicators of absolute values of leukocytes in the examined groups showed no significant changes. Thus, there is a slight decrease in patients with a tension headache and migraine (6130.77 ± 347.92 and 5845.83 ± 202.49 μl, respectively, with control values of 6900 ± 600.0 μl), together with this with a migraine a small leukocytosis is observed with aura (7066.67 ± 406.80 μl, P> 0.05).Absolute and relative values of lymphocytes show pronounced lymphocytosis in these conditions. Thus, the highest average values of relative indices are observed with tension headache (42.08 ± 1.90% and), slightly less with migraine with aura (41.67 ± 1.55%) and least of all with migraine (39.92 ± 1.21%), relative to the control (32.9 ± 2.2%), the absolute values of lymphocytes with tension headache (576.92 ± 200.22 μl) were significantly reduced as compared to the control (2288.6 ± 260.4 μl) and values in patients with migraine (2333.33 ± 106.60 μl) and migraine from auras (2968.78 ± 204.76 μl, P< 0.05).A comparative analysis of the relative and absolute indices of cellular immunity in patients showed the absence of pronounced disorders, with the exception of the absolute values of T-lymphocytes and T-cytotoxic cells in patients with migraine with aura.Thus, the mean values of the relative index of the total pool of CD3+ lymphocytes in patients with tension headache do not practically differ from the mean values of the control group (53.38 ± 0.94% and 53.6 ± 1.5%, respectively), also there is a slight but not significant increase in the absolute values of the index (1367.08 ± 98.84 and 1207.8 ± 129.8 μl, respectively).
|
3. Conclusions
- As a result of a comparative analysis of the obtained results of the immune system in patients with migraine, migraine with aura and tension type headache, there were no significant deviations of cellular immunity indicators relative to control values, except for a significant increase in B-lymphocytes, which indicates a postponed inflammatory process and indicates the integrity they have an immune homeostasis in the interictal period.
ACKNOWLEDGEMENTS
- The authors thank the patients who participated in this study and their parents/guardians and family members. The author thanks head of the Department of Neurological diseases, children's nervous diseases, medical genetics Professor Madjidova Yakuthon Nabievna for assistance in the preparation of the article to the publication.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML