-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(3): 71-75
doi:10.5923/j.ajmms.20190903.01

Determination of the Bile Ducts Injuries Risk in the Surgery of Cholelithiasis
M. M. Akbarov1, Z. B. Kurbaniyazov2, P. A. Askarov2
1Republican Specialized Scientific-Practical Medical Centre of Surgery named after academician V.Vakhidov, Tashkent, Uzbekistan
2Samarkand State Medical Institute, Samarkand, Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

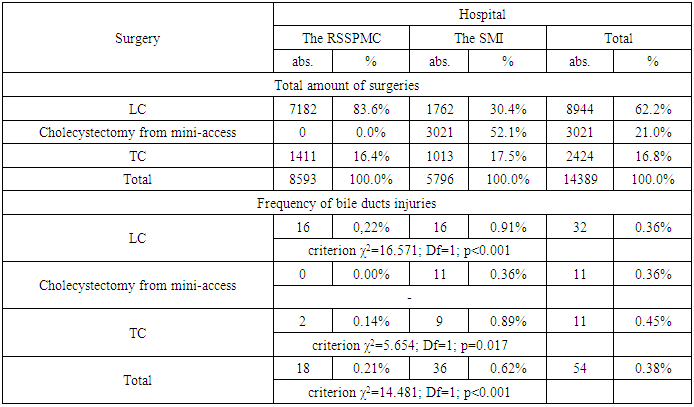
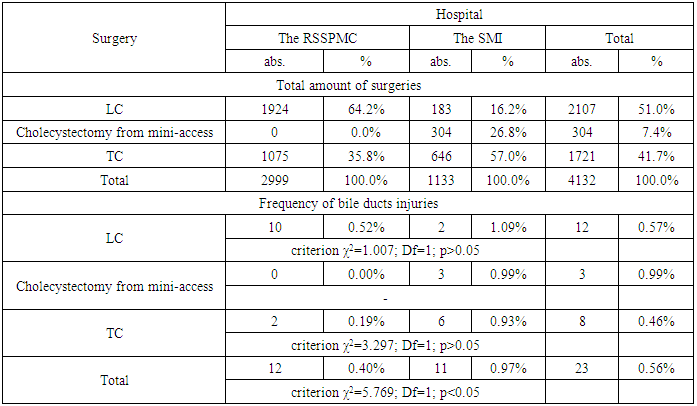
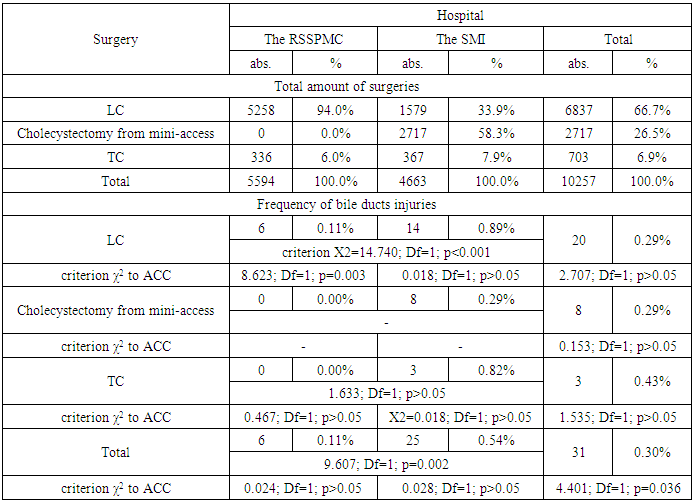
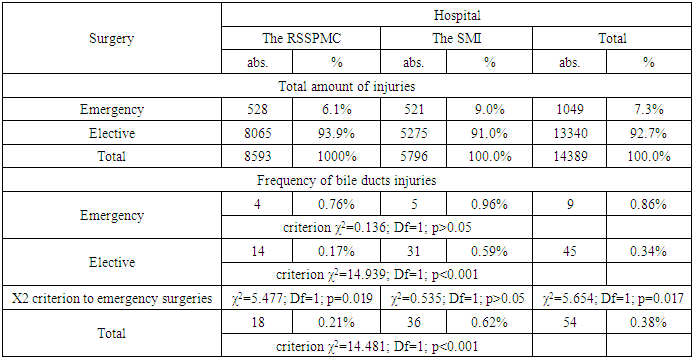
When performing operations on the abdominal organs, the frequency of intraoperative injury of the bile ducts is 0.09 - 3%. As a rule, iatrogenic trauma of the extrahepatic bile ducts occurs during surgery on the biliary tract, most often - cholecystectomy. The article is devoted to the stratification analysis of the risk of damage of the bile ducts in surgery for gallstone disease. The study revealed that the probability of damage of the bile ducts in gallstone disease surgery is 0.38% (in 54 from 14389 operated patients), and depending on the type of surgery, the frequency of this complication was 0.36% (in 32 from 8944) with laparoscopic cholecystectomy, 0.45% (11 from 2424) - with traditional cholecystectomy and 0.36% (11 from 3021) with cholecystectomy from a mini-access. A significant difference in the risk of damage was determined for acute calculous cholecystitis - 0.56% and chronic calculous cholecystitis - 0.30% (criterion X2 = 4.401; Df = 1; p = 0.036). In turn, the risk of damage to the bile ducts also differed significantly during emergency surgery - 0.86% from planned interventions - 0.34% (criterion X2 = 5.654; Df = 1; p = 0.017).
Keywords: Cholelithiasis, Bile ducts, Cholecystectomy, Injury, Surgery
Cite this paper: M. M. Akbarov, Z. B. Kurbaniyazov, P. A. Askarov, Determination of the Bile Ducts Injuries Risk in the Surgery of Cholelithiasis, American Journal of Medicine and Medical Sciences, Vol. 9 No. 3, 2019, pp. 71-75. doi: 10.5923/j.ajmms.20190903.01.
1. Introduction
- According to the World Health Organization, damage to the bile ducts, despite the constantly improving technique of surgical interventions, is one of the most terrible complications of biliary surgery and has no tendency to decrease [1]. When performing operations on the abdominal organs, the frequency of intraoperative damage to the bile ducts is 0.09 - 3%. As a rule, iatrogenic trauma of the extrahepatic bile ducts occurs during surgery on the biliary tract, most often cholecystectomy, less frequently in operations on the stomach, duodenum, pancreas [2].The “gold” standard in the treatment of cholelithiasis is laparoscopic cholecystectomy. A characteristic feature of the method is a new type of damage to the duct - thermal burn of the hepaticocholedochus.At the same time, the risk of mechanical injury of the main bile duct pathways during clipping of the cystic duct is not excluded. Another feature of laparoscopic cholecystectomy was an increase in the proportion of high injuries [3-4]. Injuries at the level of the common hepatic duct, bifurcation of the lobar ducts and the isolated right and left lobar ducts make up 69%, whereas with “traditional” cholecystectomy such injuries occur in 44.8% [5]. The consequences of iatrogenic damage to the bile ducts can cause catastrophic damage to the health of the patient and only in a timely and competently performed operation can prevent the development of such complications as biliary cirrhosis, portal hypertension, purulent cholangitis, hepatic failure [6]. In this regard, the prevention and surgical treatment of iatrogenic trauma of the bile ducts, the development of optimal treatment tactics and rational surgical techniques and the rehabilitation of patients are a pressing issue in hepatobiliary surgery.
2. Material and Methods
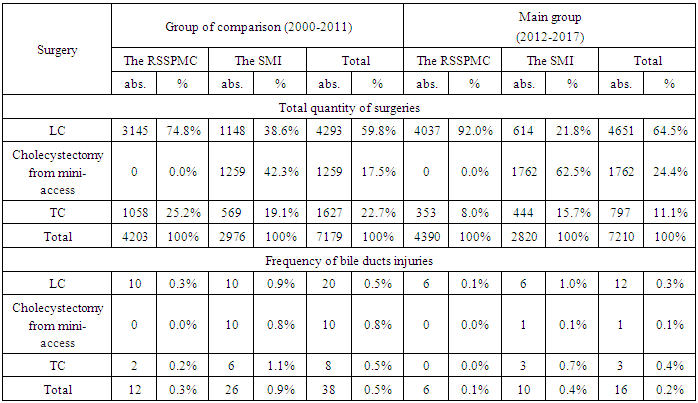
- The paper analyzes clinical material based on the results of a comprehensive examination and surgical treatment of 14389 patients with cholelithiasis operated at the Republican Specialized Scientific-Practical Medical Centre of Surgery (RSSPMC) named after academician V.Vakhidov and Samarkand Medical Institute (SMI) between 2000 and 2017. Patients were divided into 2 groups. The comparison group consisted of 7179 interventions, 4293 (59.8%) of which were performed laparoscopically, 1259 (17.5%) cholecystectomy from a mini-access and 1627 (22.7%) operations performed in the traditional way in the period of 2000-2010.The main group of the study consisted of 7210 cholecystectomies which in 4651 (64.5%) patients underwent by laparoscopic way, in 1762 (24.4%) patients cholecystectomy was made from a mini-access and in 797 (11.1%) cases the intervention was performed in the traditional way from (2011 to 2017).
3. Results
- In the group of comparison during that period at the RSSPMC there were performed 3145 (74.8%) laparoscopic cholecystectomies (LC) and 1058 (25.2%) traditional cholecystectomies (TC). In that group at Samarkand Medical Institute (SMI) there were performed 1148 (38.6%) LC, 1259 (42.3%) cholecystectomies from mini- access and in 1627 (22.7%) cases – TC. In the main group of investigation at RSSPMC there were performed 4037 (92%) LC and 353 (8.0%) TC; at the SMI – 614 (21.8%) LC, 1762 (62.5%) cholecystectomies from mini- access and 444 (15.7%) TC. The frequency of bile ducts injuries at both hospitals is given in the Tab. 1.
|
|
|
|
|
4. Discussion
- The introduction of new technologies in surgical practice brings new types of iatrogenic injury. Of great interest is the question of the causes of the extrahepatic biliary tract injuries. Many authors consider the cause of accidental injuries of the hepaticocholedochus anomalies of the biliary tract and vessels in the portal fissure, inflammatory infiltration and cicatricial adhesions in the neck of the gallbladder, bleeding that occurred during the operation, forced surgical intervention at night, Mirizzi’s syndrome (type II) [7]. Despite certain successes achieved in this complex field of surgery, unsatisfactory results are observed in even the most experienced surgeons on average in 10% of cases [8]. According to Spence L.H. with co-authors such patients need repeated, sometimes repeated reconstructive operations and are rightly called “biliary cripples” [9]. From the point of view of treatment outcomes, the timing of detection of bile ducts lesions is crucial. Accordingly, the long-term results of surgical treatment depend on the time of detection and the nature of the injury [10]. The main reasons for failures in the treatment of injuries of the main bile ducts are the untimely diagnosis and the performance of reconstructive surgeries that are inadequate in volume by surgeons who do not have adequate experience in biliary surgery [11]. There is no unity in the choice of the method of operation for “fresh” injuries of the bile ducts diagnosed intraoperatively or in the immediate postoperative period. There is still a desire for recovery operations, which give unsatisfactory results, due to the rapid development of cicatricial stricture or the failure of the anastomosis. A number of surgeons resort to duodenal anastomosis which leads to the development of duodenal fistula or reflux cholangitis, the development of anastomotic stricture [12]. The tactics of treatment of the bile duct injury are decisive factors that influence the choice of operation: the nature and location of injury, the condition of the crossed duct, the time of diagnosis of damage and the presence of a surgeon who has experience in reconstructive bile duct surgery. The analysis of the literature suggests that in the present period, the treatment and diagnostic tactics for iatrogenic injuries of the bile ducts is one of the most urgent and unresolved problems of modern hepatobiliary surgery.
5. Conclusions
- The probability of the bile ducts injuries in the surgery of cholelithiasis is 0.38% while depending on the type of operation, the frequency of this complication was 0.36% (in 32 of 8944) during laparoscopic cholecystectomy, 0.45% (11 of 2424) - during traditional cholecystectomy and 0.36% (11 of 3021) - during cholecystectomies from the mini-access.A significant difference in the risk of BD injuries in acute calculous cholecystitis (ACC) - 0.56% and in chronic calculous cholecystitis (CCC) - 0.30% was determined (criterion X2 = 4.401; Df = 1; p = 0.036). In turn, the risk of the bile ducts injuries also differed significantly during emergency surgery - 0.86% from planned interventions - 0.34% (criterion X2 = 5.654; Df = 1; p = 0.017).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML