-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(2): 63-70
doi:10.5923/j.ajmms.20190902.06

Extracorporal Immunopharmacotherapy in Complex Treatment of Cervical Cancer and Ovarian Cancer
S. V. Kamishov , M. N. Tillyashaykhov
Republican Specialized Scientific-Practical Medical Center of Oncology and Radiology of Ministry of Health of the Republic of Uzbekistan
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

When prescribing extracorporeal immunopharmacotherapy methods for patients with cervical and ovarian cancers, the results of clinical and diagnostic studies, anamnestic data, the presence of specific antitumor or alternative treatments before admission to the hospital, as well as the histological type of the tumor, the macroscopic form of growth and the degree of its prevalence were taken into account. Extracorporeal immunopharmacotherapy methods are recognized, first of all, to reduce toxic manifestations after chemotherapy and radiation therapy as well as to improve the general condition after extensive surgery in patients with oncologic diseases. In the course of the conducted surveys an algorithm for preparing patients with cervical and ovarian cancers to perform EIFT techniques was developed and it included: 1) the study of anamnestic data (the presence of concomitant diseases and earlier symptomatic or specific treatment); 2) the study of general clinical and biochemical analysis of blood; 3) the study of immunological parameters; 4) study of urinalysis; 5) study of the degree of toxicity of chemotherapy by the CTC-NCIC scale; 6) study of the subjective general condition of patients (Performancestatus) by the Karnovsky’s scale and ECOG (WHO); 7) assessment of the quality of patients life according to the SF-36 questionnaire; 8) the conclusion of the cardiologist; 9) if necessary, conservative fortifying, cardiotropic, hepatotropic and other types of therapy were given to patients.
Keywords: Ovarian cancer, Cervical cancer, Immunotherapy, Extracorporeal immunopharmacotherapy, Polychemotherapy
Cite this paper: S. V. Kamishov , M. N. Tillyashaykhov , Extracorporal Immunopharmacotherapy in Complex Treatment of Cervical Cancer and Ovarian Cancer, American Journal of Medicine and Medical Sciences, Vol. 9 No. 2, 2019, pp. 63-70. doi: 10.5923/j.ajmms.20190902.06.
Article Outline
1. Introduction
- An increased attention to the problem of increasing cancer incidence is one of the characteristic features of the modern health care system of all developed countries.This is due, above all, to a steady trend of increasing malignant neoplasms among the population which has reached rather high rates and will increase in the foreseeable future. Oncological diseases are initially detected every year in 12 million people worldwide, while the number of cancer cases in the world over the past ten years has increased by twenty percent.This is the second cause of death after cardiovascular diseases in developed countries and the common cause of 10% of all deaths in the world which is about 6 million deaths per year [4, 8, 12].The progress has been made in recent years in the study of immunology and cancer immunotherapy, including malignant tumors of the female reproductive system. Evidence has been obtained that the majority of malignant tumors develop on the basis of evident disorders of the immune system arising already in pre-tumor diseases, are determined by the prevalence of the tumor process and are aggravated by the used therapeutic effect. These data, as well as information about a more favorable course of the disease with preserved immunity encourage many researchers to further study of the state of the immune system and develop more effective treatment regimens for patients with malignant tumors with the inclusion of immunotherapy methods [1, 2, 5, 9]. Ovarian cancer (OC) currently continues to be the fourth leading cause of cancer mortality among women and is still the most fatal of gynecological tumors [3, 4, 12]. Cervical cancer (CC) is also one of the most common malignant tumors of the female genitalia. The incidence rate throughout the world varies from 10 to 40 per 100 thousand of the female population, while almost half of the patients die within the first year due to late diagnosis of the disease [3, 5, 6, 10].Common forms of the disease worsen the prognosis and require the use of combined and complex treatment methods. At the same time, it is necessary to take into account the high toxicity of many anticancer drugs, which also leads to the limitation of surgical intervention in elderly patients and in the presence of severe concomitant pathologies [5, 7].The percentage of recurrences in patients with OC is approximately 75% and this is equivalent to approximately 2500 patients per year. Relapse therapy is the most controversial section of gynecological oncology and is primarily palliative, and with this in mind, its main goal is to prolong life and improve its quality [8]. Five-year survival for cervical cancer according to different authors in the presence of stage III-IV of the disease is 17-22%.The main cause of mortality is also recurrence of cancer ranging from 37% to 50% of all treated patients [3, 9, 12]. In this regard, the improvement of drug therapy methods in order to extend and improve the quality of patients life is a very urgent problem of clinical oncology [6, 9].For many years cancer treatment has focused on surgery, chemotherapy, and radiation therapy, but as knowledge of the immune system's capabilities in the fight against cancer deepened, treatment methods using the immune system against malignant tumors began to develop.Although immunotherapy of malignant tumors is a relatively new scientific trend, the results obtained in the last decade allow us to count on the important role of immunotherapeutic approaches in the treatment of oncological diseases [8, 11]. Immunosuppression of mixed genesis is observed in patients with oncological diseases after conducting a comprehensive antitumor treatment.First, the fact of the development of the oncological process allows us to speak about the presence of an initial defect in the function of immune surveillance, which allows tumor cells to multiply unhindered. Secondly, the tumor cells themselves have a local and immunosuppressive effect due to the production of various substances. Thirdly, modern complex antitumor treatment (surgical treatment, radiotherapy and chemotherapy) turns out to be a powerful factor inducing generalized immunosuppression.In this regard, cancer patients make up a special group of patients who have been advised to undergo immunotherapy [6, 8]. Currently, the main objectives of immunotherapy in oncology have been formulated - these are basic immunotherapy of tumors with the aim of obtaining a direct antitumor effect, reducing the side effects of traditional antitumor therapy (treatment of myelosuppression and immunosuppression, correction of general toxic effect, antioxidant effect), prevention of tumor recurrence and the appearance of new other tumors, prevention and treatment of concomitant infectious complications (viral, bacterial and fungal infections) [1, 4]. Obtaining new unique immunomodulatory drugs has created a qualitatively new basis for the correction of immunity disorders, it became possible to act more selectively on individual components and links of this system. On the other hand, there are prospects for methods that have a positive effect on the immune system as a whole - the use of adaptogens, plasma exchange methods, perfusion of blood through sorbents, treatment with various activators [8, 10].One of the methods that have been successfully used for the relief of intoxication for a long time is therapeutic plasmapheresis which consists in removing blood plasma containing antibodies, circulating immune complexes, cytokines, products of cellular metabolism, etc.Modern methods of extracorporal immunopharmacotherapy (EIFT) are in essence an effective extension of therapeutic plasmapheresis. If during the plasmapheresis the cellular elements immediately after their separation from the plasma are returned to the patient, then with EIFT there is an additional release of the leukocyte fraction which is then subjected to treatment outside the body with a specific drug.Leukocytes activated in this way after returning to the bloodstream are able to synthesize the factors that activate the immune system and, consequently, activate other cells of the immune system.Thus, EIFT is a separate direction, born at the junction of immunology and extracorporal hemocorrection [5].At the same time, it should be noted that clinical trials of various immunological approaches in oncology are still episodic, and their implementation is still difficult due to technical problems, the toxicity of the used complexes, the lack of criteria for evaluating the feasibility of administering immunocorrective treatment and its effectiveness.The development, study and introduction into clinical practice of various methods of immunotherapy is an actual issue of modern oncology, since the application of these techniques can expand the therapeutic possibilities of standard treatment methods and reduce their side effects which will improve the quality of patients life with malignant tumors.
2. Aim of the Research
- To conduct extracorporal immunopharmacotherapy in patients with ovarian cancer and cervical cancer.
3. Material and Methods
- The examination included 268 patients with cervical cancer T2-3N0-1M0 stages (stage II-III), as well as 261 patients with ovarian cancer T2-3N0-1M0 stages (stage II-III) who were examined and treated in the gynecological oncology and chemotherapy departments of the Republican Specialized Scientific-Practical Medical Center of Oncology and Radiology (RSSPMCOR) from 2004 to 2014.In accordance with the objectives of the study the following groups of patients were created according to the methods of immunotherapy as part of complex treatment:Group 1 - 83 (31.0%) patients with cervical cancer (CC) who received extracorporeal immunopharmacotherapy (EIFT) without plasma exchange (PF);Group 2 - 67 (25.0%) of cervical cancer (CC) patients who received EIFT with preliminary PF;Group 3 (control) - 118 (44.0%) patients with cervical cancer (CC) without immunocorrective therapy;Group 4 - 78 (29.9%) patients with ovarian cancer (OC) who received EIFT without PF;Group 5 - 73 (28.0%) patients with ovarian cancer (OC) treated with EIFT with PF;6 control group - 110 (42.1%) patients with ovarian cancer (OC) without immunocorrective therapy.Morphologically, non-squamous epidermoid cancer was determined in 147 (54.9%) patients and keratinous squamous epidermoid cancer in 121 (45.1%).According to the degree of tumor differentiation, 138 (51.5%) patients were diagnosed with low-grade cancer, in 46 (17.2%) cases – moderately differentiated, and 84 (31.3%) patients had highly differentiated cervical cancer.The analysis of histological preparations in patients with OC showed that in the majority - 222 (85.1%) of the examined patients were diagnosed with cystadenocarcinoma, 39 (14.9%) patients had other forms of OC.All patients with cervical cancer received complex treatment, including neoadjuvant polychemotherapy (NAPCT), surgery and / or chemoradiotherapy (CRT) or two-stage combined radiation therapy, including remote telegrammatherapy (RTGT) and intracavitary brachytherapy.At the first stage all patients with cervical cancer have systemic or intraarterial polychemotherapy according to the following scheme: cisplatin 50 mg / m2 + 5-fluorouracil 1000 mg / m2 for 4 days, 4-6 courses 1 time in 3 weeks. Radiation therapy and chemotherapy were carried out both in the adjuvant and in the neoadjuvant mode. Surgical treatment was performed as a radical operation.
4. Results and Discussion
- When prescribing methods of extracorporeal immunotherapy for patients with cervical cancer and ovarian cancer, they tried to take into account the results of clinical diagnostic studies to the greatest extent. Analysis of anamnestic data of cervical cancer patients showed that the majority - 196 (73.1%) patients from the first visit to the gynecologist with complaints before the diagnosis of cervical cancer were treated with conservative anti-inflammatory therapy.33 (12.3%) patients were treated independently with unconventional methods, and 16 (4.9%) were performed electrocoagulation without histological examination.Specific anticancer treatment before admission to the hospital most of the patients did not receive. A small part of patients with cervical cancer was given specific antitumor treatment.Thus, 15 (5.6%) patients had previously undergone RTGT (summary local radiotherapy dose 40-50 Gy) without special effect and 8 (3.0%) patients - combined radiotherapy (RTGT + brachytherapy).In 3 of them we managed to achieve a partial regression of the tumor, and in 5 patients - stabilization of the tumor process with some subsequent improvement in symptoms. The analysis of the anamnestic data of patients with OC has made it possible to establish that in the period from the first visit to the gynecologist with complaints to the diagnosis of OC most of the 215 (82.4%) patients underwent conservative anti-inflammatory therapy.Patients with OC did not receive specific antitumor treatment before admission to the hospital.33 (12.6%) patients were treated independently using unconventional methods and 13 (5.0%) women were given hormone therapy for nodular goiter and ovarian cysts. Morphological analysis of the surgical material and biopsy results in patients with cervical cancer showed that in the majority – in 255 (95.1%) of the examined patients we had histologically revealed squamous cervical cancer, 13 (4.9%) patients had clear cell adenocarcinoma.In 147 (56.3%) patients serous cystadenocarcinoma was detected, in 50 (19.2%) - endometrioid cystadenocarcinoma, in 28 (10.7%) - mucinous cystadenocarcinoma, in 20 (7.7%) - clear cell cystadenocarcinoma and in 16 (6.1%) patients – mixed-type cystadenocarcinoma.According to the degree of tumor differentiation, 72 (27.6%) patients were diagnosed with poorly differentiated cancer, 129 (49.4%) - moderately differentiated, and 60 (23.0%) patients - highly differentiated cancer. Using clinical and instrumental methods of research in all patients with cervical cancer, the macroscopic form of tumor growth and the extent of the tumor process were determined.As it was mentioned earlier, in the majority of patients – 119 (44.4%) - we diagnosed stage IIIB of the disease. In most cases, in 140 (52.2%) of the examined patients it was revealed tumor volume in the range from 10 to 15 cm3.It was not possible to determine the initial tumor using clinical and instrumental methods in the majority of patients - in 164 (61.2%) cases. In 118 (44.0%) patients the tumor spread to the upper third of the vagina. In the case of OC, the majority — 107 (41.0%) of the examined patients were diagnosed with stage IIIC of the disease.According to the ultrasound examination, a tumor of more than 10 cm was detected in 143 (54.8%) patients and up to 10 cm in 118 (45.2%) patients. At the same time, one-sided lesion was observed in 113 (43.3%) of them and bilateral - in 148 (56.7%) patients. Dissemination of the peritoneum was absent in 107 (41.0%) patients, had insignificant dimensions - in 91 (34.9) and up to 2 cm - in 63 (24.1%) patients.The presence of ascitic fluid in the abdominal cavity was absent in 145 (55.6%) patients, was determined in the amount of up to 2 liters - in 65 (24.9%) and more than 2 liters - in 51 (19.5%) patients. Tumor cells in ascites or abdominal flushing were detected in 73 (62.9%) patients and were absent in 43 (37.1%) of 116 patients with ascites.All patients with cervical cancer have received a comprehensive treatment: two-stage combined radiation therapy, including remote telegrammatherapy (RTGT) by a split course with a single local dose of 2 Gy up to summary local radiotherapy dose 50 Gy 5 times a week and intracavitary brachytherapy with a single local dose of 5 Gy up to summary local radiotherapy dose of 45-55 Gy every other day.Also all patients with cervical cancer have received systemic or intraarterial polychemotherapy according to the following scheme: cisplatin 50 mg/m2 + 5-fluorouracil 1000 mg/m2 for 4 days, 4-6 courses 1 time in 3 weeks. Radiation therapy and chemotherapy were carried out both in the adjuvant and in the neoadjuvant mode.Surgical treatment was carried out in the form of a radical operation of Wertheim-Megeiss.All patients with OC were carried out a combined therapy in adjuvant or neoadjuvant regimen, polychemotherapy according to the scheme: cisplatin 75 mg/m2 + cyclophosphamide 1000 mg/m2 for 1 day for 4-6 courses 1 time per 3 weeks and surgical treatment in the amount of radical or cytoreductive surgery.The frequency and severity of reactions depended on the initial state of these organs and comorbidities. Among the early forms of urinary bladder reactions, radioepitheliitis should be distinguished which most often appears in the middle or at the end of the course of combined irradiation. Clinically, these complications were manifested by pollacyuria and cystalgia.In some cases late radiation damages of these organs occurred. Most patients had reversible cystalgia, pollakiuria, hematuria, rectitis, epithelium, ulceration, stenosis, necrosis. Rektita appeared later than cystitis, and were accompanied by tenesmus, itching and diarrhea. Late rectitis was more common than late cystitis. Also encountered radiation dermatitis accompanied by swelling and pain occured.Methods of extracorporeal immunopharmacotherapy (EIFT) were designed, first of all, to reduce toxic manifestations after chemotherapy and radiation therapy, as well as to improve the general condition after extensive surgery in patients with oncologic diseases.For the implementation of EIFT techniques it was necessary to develop indications and contraindications for their implementation in this category of patients. In the process of the conducted examinations we developed an algorithm for preparing patients with cervical cancer and ovarian cancer to perform EIFT techniques.We also developed clinical and laboratory criteria for the inclusion of patients with cervical cancer and ovarian cancer in the study on conducting EIFT methods. Accordingly, criteria were developed for excluding patients with CC and OC from the EIFT study.Since EIFT techniques involve taking from 200 to 1000 ml of blood from the bloodstream of patients with its special treatment and subsequent return to the bloodstream, conservative medical measures in some patients were carried out as prevention of exacerbation of concomitant diseases.Immunotherapy in patients with CC and OC was performed in the pre- and postoperative period. In the 1st group 83 (31.0%) patients with cervical cancer and in the 4th group - 78 (29.9%) patients with OC were performed EIFT by exfusion of 200-250 ml autologous blood into “Gemakon” or “Terumo” sterile containers, with incubation of immunomodulators: neovir in a total dose of 750 mg (for 3 treatments), cycloferon in a total dose of 750 mg (for 3 treatments) or polyoxidonium in a total dose of 36 mg (for 3 treatments) at 37°C for 60-100 minutes followed by reinfusion of the resulting conjugate.67 (25.0%) patients in the 2nd group with cervical cancer and 73 (28.0%) patients with OC in the 5th group were performed EIFT which was an extension of plasmapheresis. If during normal plasmapheresis, the cellular elements immediately after their separation from plasma are returned to the patient, then during EIFT, in order to achieve an additional immunocorrective effect, they are further processed outside the body with a specific drug.500-1000 ml of autologous blood were placed in “Gemakon” or “Terumo” sterile containers, then it was centrifuged at 3000 rpm for 30 minutes.50-80 ml of the blood plasma supernatant containing antibodies, circulating immune complexes, cytokines, and products of cell metabolism were removed. Then, the obtained leukotrombomass and erythrocyte mass were incubated with the above immunomodulators, in a total dose of 30 mg (for 3 procedures) at 37°C for 60-100 minutes followed by the return of the conjugate to the patients circulatory system.118 (44.0%) patients with CC in the 3rd control group and 110 (42.1%) patients with OC in the 6th control group did not receive immunotherapy. Thus, when prescribing EIFT methods to patients with CC and OC we tried to take into account the results of clinical diagnostic studies to the greatest extent. Anamnestic data, the presence of specific antitumor or non-traditional types of treatment before admission to the hospital, as well as the histological type of the tumor, the macroscopic form of growth and the degree of its prevalence were taken into account.
5. Evaluation of EIFT Techniques Effect on Remote Treatment Results
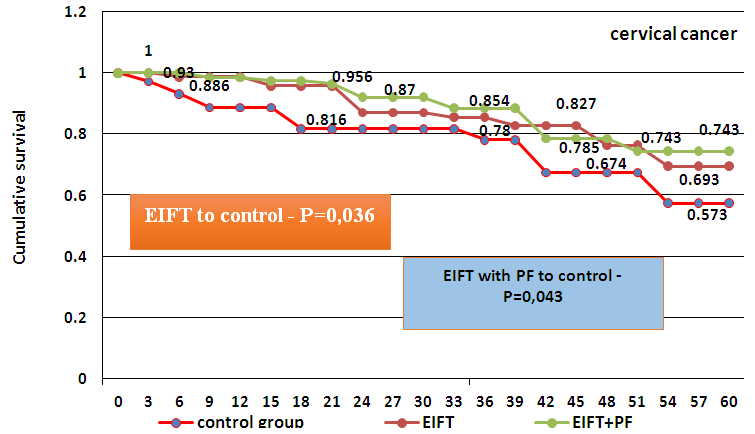
- Evaluation of EIFT techniques effect on long-term results of treatment was carried out by studying the indices of general and disease-free survival of patients with cervical cancer and ovarian cancer after treatment. In the first year, patients were monitored every 3 months, then every 6 months. The observation period ranged from 3 to 10 years.According to the latest published data in the literature of the CIS countries and abroad, 5-year survival in patients with cervical cancer is 65% and varies from 15 to 80%, depending on the spread of the tumor process. At the same time, the five-year survival rate at stage IIB is 48-63%, IIIA - 35-44%, IIIB - 12-31.5%. On average, at stage II, 5-year survival is 40-67%, at stage III - 35-45. In our studies in patients with cervical cancer, stage II of the disease was diagnosed in 90 (66.2%) and stage III – in 46 (33.8%) patients. In patients with cervical cancer, stage II disease was diagnosed in 90 (66.2%) and stage III – in 46 (33.8%) patients.In our studies, the overall 5-year survival rate of patients with oncological diseases after complex therapy in combination with immunotherapy was as follows: in the 1st group of cervical cancer (CC) patients receiving EIFT without PF - 69.3 ± 6.2% (P = 0.037); in the 2nd group of patients with CC, receiving EIFT with preliminary PF - 74.3 ± 7.1% (P = 0.041); in the 3rd control group of patients with CC without immunotherapy - 58.7 ± 5.8%; in the 4th group of patients with ovarian cancer (OC) receiving EIFT without PF - 71.5 ± 6.7% (P = 0.036); in the 5th group of patients with OC, receiving EIFT with PF - 76.5 ± 6.3% (P = 0.043) and in the 6th control group of patients with OC without immunotherapy - 62.5 ± 6.1% (Fig. 1, 2).
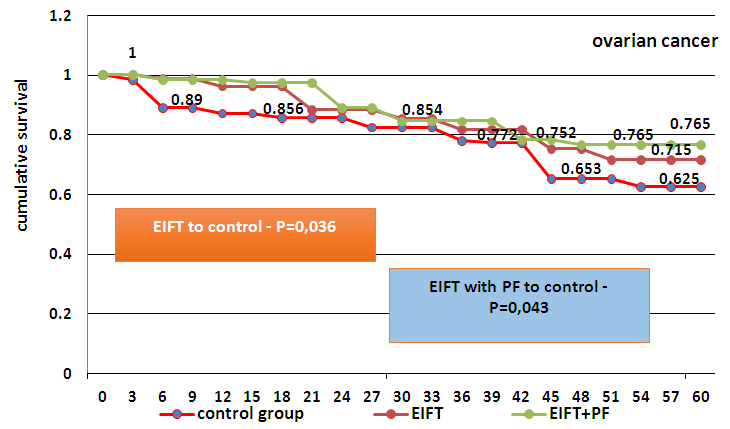 | Figure 2. Comparative assessment of the total cumulative five-year survival according to KaplanE.L. et Meier R. in patients with OC depending on the type of immunotherapy in complex treatment |
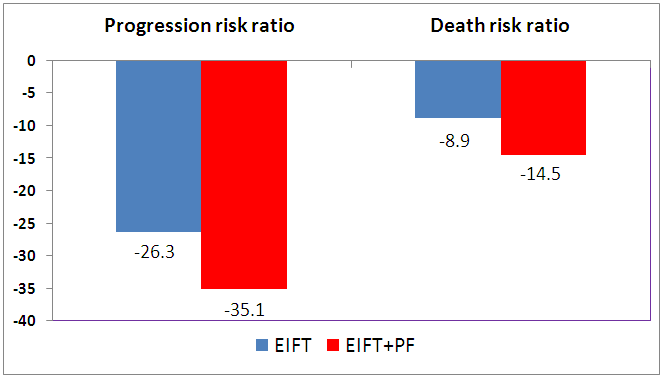 | Figure 3. Progression risk ratio (hazardratio, HR) and risk of death in patients with cervical cancer |
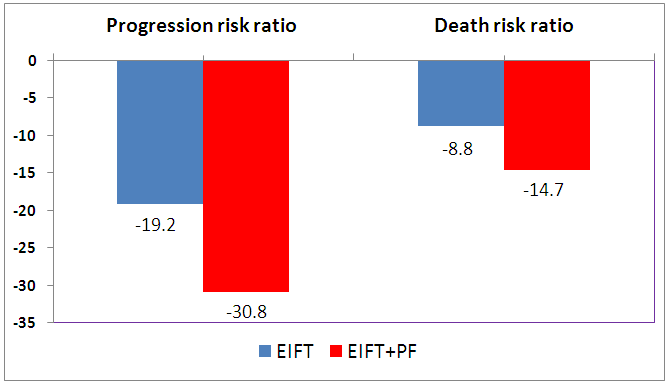 | Figure 4. Progression risk ratio (hazardratio, HR) and risk of death in patients with ovarian cancer |
6. Conclusions
- EIFT methods were designed, first of all, to reduce toxic manifestations after chemotherapy and radiation therapy, as well as to improve the general condition after an extensive surgery in patients with oncological diseases.In the course of our examinations, we developed an algorithm for preparing patients with cervical cancer and ovarian cancer to perform EIFT techniques, including: 1) the study of anamnestic data (the presence of concomitant diseases and earlier symptomatic or specific treatment); 2) the study of general clinical and biochemical analysis of blood; 3) the study of immunological parameters; 4) study of urinalysis;5) study of the degree of toxicity of chemotherapy by the CTC-NCIC scale; 6) study of the subjective general condition of patients (Performancestatus) by the Karnovsky scale and ECOG (WHO); 7) assessment of the patients life quality according to the SF-36 questionnaire; 8) the conclusion of the cardiologist; 9) if necessary, conservative fortifying, cardiotropic, hepatotropic and other types of therapy were given to patients.We also developed clinical and laboratory criteria for the inclusion of patients with cervical cancer and ovarian cancer in the study on EIFT techniques, which included: 1) a histologically confirmed diagnosis of CC and OC; 2) age from 21 to 75 years;3) Stage IIA-IIIB in patients with cervical cancer and Stage IIA-IIIC in patients with ovarian cancer; 4) condition after surgical treatment and ongoing chemotherapy or radiation therapy; 5) Performancestatus 40-80% by the Karnovsky’s scale and 1-3 points by the ECOG (WHO); 6) the degree of toxicity of chemotherapy I-IV by the CTC-NCIC scale; 7) deterioration of the physical and mental components of health according to the questionnaire SF-36;8) the absence in the history of other malignant diseases and severe comorbidities; 9) hemoglobin> 10 g / l, leukocytes> 4,000 / mm3, neutrophils> 1.5000 / mm3, platelets> 100.00 / mm3; 10) indicators of kidney function: creatinine ≤100 µmol / l; if creatinine ≥100 and ≤130 µmol / l, creatinine clearance should be > 60 ml / min.The patient does not turn on if plasma creatinine > 130 µmol / l;11) liver function indicators: total bilirubin <1.5x upper limit of normal, ALT and AST <1.55x upper limit of normal, alkaline phosphatase <5x upper limit of normal.Accordingly, criteria for excluding patients with cervical cancer and ovarian cancer from the EIFT study were developed. They included: 1) current or previous treatment with research drugs; 2) the presence of a severe pathology of the gastrointestinal tract (Crohn's disease, ulcerative colitis, partial or complete intestinal obstruction, chronic diarrhea or maldabsorption syndrome);3) the presence of severely controlled associated diseases, such as diabetes or infectious diseases; 4) the presence of a history of mental disorders; 5) a history of severe renal disease; 6) the presence of initially peripheral polyneuropathy or auditory neuropathy> 1 stage; 7) the presence of a known hypersensitivity to immunomodulators (neovir, cycloferon, polyoxidonium); 8) disseminated intravascular coagulation syndrome; 9) myocardial infarction for the last 6 months, hereditary heart diseases, decompensated heart failure, any cardiovascular pathology of the III-IV stage (according to the classification of the New York Heart Association NYHA) which are therapeutically uncorrected.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML