-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2019; 9(2): 50-53
doi:10.5923/j.ajmms.20190902.03

Ocular Birth Injuries following Forceps Assisted Delivery in a Newborn
Sagili Chandrasekhara Reddy1, 2
1Department of ophthalmology, School of Medicine, University Sains Malaysia, Kerian, Kelantan, Malaysia
2Department of Ophthalmology, Faculty of Medicine and Defence Health, National Defence, University of Malaysia, Sungai Besi Campus, Kuala Lumpur, Malaysia
Correspondence to: Sagili Chandrasekhara Reddy, Department of ophthalmology, School of Medicine, University Sains Malaysia, Kerian, Kelantan, Malaysia.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A full term baby was found to have ocular injury in the left eye after forceps assisted delivery. Examination of the face revealed forceps indentation mark on the left forehead extending downwards up to medial canthus of left eye, pressure mark on the lateral side of upper eyelid below the eyebrow, ecchymosis on the medial side of upper eyelid, and mild ecchymosis on the medial and lateral side of lower eyelid. Examination of the left eye showed small subconjunctival haemorrhage on the medial side and diffuse haziness of the cornea; iris, pupil and lens were not visible. The diagnosis of corneal oedema due to Descemet’s membrane rupture following blunt trauma by obstetrics forceps was made in the left eye. Right eye was normal. The corneal oedema resolved completely with dexamethasone eye drops, gentamicin eye drops in the left eye. Fundus examination after dilating the pupils showed normal fundus in both eyes, except superficial retinal haemorrhages on the temporal side in the left eye. After four weeks of birth injury, slitlamp examination of left eye showed vertical, linear corneal opacities on either side of pupillary area in the left eye. The followed up examination at the age of 18 months showed good vision in both eyes and vertical, linear corneal opacity on the medial side of the pupil in the left eye. It is a good practice to refer all the forceps delivered newborns to the ophthalmologist for eye examination to rule out any ocular and adnexal injuries in order to prevent subsequent visual loss.
Keywords: Ocular birth injury, Forceps delivery, Corneal oedema, Retinal haemorrhages
Cite this paper: Sagili Chandrasekhara Reddy, Ocular Birth Injuries following Forceps Assisted Delivery in a Newborn, American Journal of Medicine and Medical Sciences, Vol. 9 No. 2, 2019, pp. 50-53. doi: 10.5923/j.ajmms.20190902.03.
1. Introduction
- Injury to cornea occurs from the placement of forceps blade across the globe and orbit during delivery. Ocular injuries from forceps delivery are uncommon today because the use of forceps for the delivery of neonates that remain high in birth canal is rarely done. However, this is practiced in the developing countries where the surgical facilities for caesarean operation are not readily available.In a large series of newborns delivered through normal vaginal delivery, forceps delivery, caesarean delivery, and vacuum extraction, Jain et al [1] reported the prevalence of ocular injuries (eye or adnexa or both) was 17.3% (85 out of 491) in forceps delivery newborns and 15% (144 out of 962) in normal vaginal delivery babies. Holden et al [2] reported a significantly higher incidence of external ocular trauma in one or both eyes in a controlled study of 133 babies born with use of forceps deliveries and 133 babies born without instrumentation (normal delivery). The reasons for forceps assisted delivery in their study were foetal distress, prolonged second stage labour, and failure to progress.A rare case of ocular birth injuries (forceps pressure mark, ecchymosis on the eyelids, diffuse haziness of the cornea, and superficial retinal haemorrhages) in the left eye following successive vacuum and forceps assisted delivery in a full term newborn boy. This is the first case report of ocular birth injuries following forceps assisted delivery from Malaysia since the literature search did not show any such case from this country. A brief review of literature published in recent years on this subject is also included.
2. Case Report
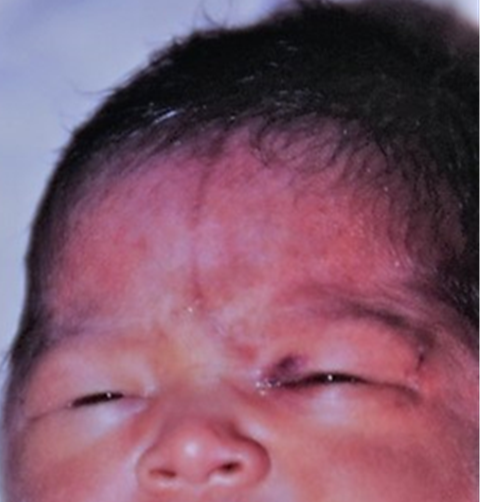
- A full term baby was found to have foetal distress/bradycardia during labour (by cardiotocography), and immediately vacuum extraction delivery was attempted but could not succeed. Then, forceps-assisted delivery was done. The newborn boy was noted to be extremely pale with irregular respiration (APGAR score 5). He was admitted to the neonatal ward. Large subaponeurotic haemorrhage, forceps pressure mark on the left forehead and left eyelids, and diffuse haziness of left cornea were noted. Vital signs were normal. Systemic examination did not reveal any abnormality. He was diagnosed to have mild birth asphyxia and anaemia. He was resuscitated for asphyxia and one unit of packed cell transfusion was given for anaemia. He was referred for an ophthalmology consultation.On examination of face, forceps indentation mark on the left forehead extending downwards up to medial canthus of left eye, pressure mark on the lateral side of upper eyelid below the eyebrow, ecchymosis on the medial side of upper eyelid, and mild ecchymosis on the medial and lateral side of lower eyelid of the left eye were noted (Fig 1).
 | Figure 2. Showing resolving corneal oedema in the left eye |
 | Figure 3. Showing vertical, linear corneal opacities on the medial side and lateral side of the pupillary area of central cornea in the left eye |
3. Discussion
- Jain et al [1] from India reported anterior segment eye injuries such as subconjunctival haemorrhage, ecchymosis of eyelid, hazy cornea, hyphema, facial palsy and corneal abscess, and and retinal haemorrhages, Purtscher’s retinopathy fundus changes in 85 newborns following, forceps delivery. Holden et al [2] from UK, in their study of 133 babies born with use of forceps delivery reported anterior segment eye injuries viz lid oedema, subconjunctival haemorrhage, conjunctival chemosis, corneal abrasion and corneal oedema.Other ocular injuries reported in the recent years from other countries in forceps delivery babies include isolated iris heterochromia and pseudo rubeosis iridis [3], full thickness corneal laceration with ruptured globe [4], full thickness corneal tear with corneal oedema [5], eyelid laceration, severe non axial proptosis, disinsertion of medial rectus muscle, mild diffuse corneal oedema and fixed mid-dilated pupil [6], ecchymosis of eyelid, vitreous haemorrhage and hyphema, oculomotor nerve palsy with intracranial haemorrhage, facial nerve palsy, corneal oedema [7], bilateral dense vitreous haemorrhage and unilateral macular hole visible after vitrectomy [8], isolated traumatic hyphema [9], seventh nerve palsy, lower eyelid laceration involving lacrimal drainage system, corneal oedema with no breaks in Descemet’s membrane, peripapillary haemorrhage in the left eye, and haemorrhage in the posterior retina in both eyes; and later on left optic nerve pallor with peripapillary pigmentary changes [10].At birth the Descemet’s membrane (DM) is much thinner (3-4 µm) than in an adult (10-12 µm) and more prone to injury. During obstetrics forceps-assisted delivery, accidental injury to eye occurs when the blade of the forceps slips over the inferior orbital rim compressing the globe vertically. This raises the intraocular pressure acutely, stretching the globe horizontally. The pressure exerted exceeds the elasticity of the DM which charectestically splits vertically or obliquely. Left eye is most frequently affected in this injury because left occiput anterior is the most common foetal presentation [11].Honig et al [12] described the following types of histological features in 11 cases of corneal injury from obstetrics forceps delivery and vacuum extraction: Type I – large tears of DM with its fragment extending into the anterior chamber at one end of the tear and scroll formation at the other end; Type II – scrolls of DM at each margin of the original break; Type III – small breaks in DM and healing by fibrosisat and posterior to the original tear; Type IV -- small break in DM with minimal fibrosis.The DM rupture causes immediate diffuse corneal oedema which heal after 1-3 weeks, eventually leaving the visible edges of the break and the clear cornea. After many years, the tears appear as thin, straight or slightly arched lines. These eyes are often amblyopic due to secondary corneal astigmatism. Prolonged corneal oedema should alert the ophthalmologist to look for probable DM detachment in these eyes. They advised for examination under anaesthesia using ultrasound and handheld optical coherence tomography [13]. In majority of the eyes, injection of air into the anterior chamber which apposes the detachment of DM to the posterior stroma.In the present case, there was clear evidence of Descemet’s membrane rupture clinically resulting in diffuse corneal haziness following obstetrics forceps delivery. In view of this dexamethasone eye drops were used to reduce the corneal oedema which cleared the oedema completely within a week. The cornea healed without much fibrosis resulting in thin vertical corneal opacities and good visual outcome at the last follow up.Scorcia et al [14] performed Descemet stripping automated endothelial keratoplasty in seven unilateral amblyopic eyes due to progressive endothelial cell loss leading to corneal decompensation with DM breaks caused by obstetrics forceps trauma. They concluded that the procedure restores corneal clarity, but the visual recovery is limited because of the pre-existing amblyopia resulting from high degree astigmatism. They suggested that low degree astigmatism may be associated with better visual outcome.Retinal haemorrhages were reported to be high in vacuum-assisted delivery (77.8%) than in forceps delivery (30.3%) by Hughes et al [15]. In another study by Williams et al [16], moderate to severe retinal haemorrhages were found in 28% of vacuum-assisted and 13% of forceps-assisted and 50% of sequential vacuum and forceps-assisted deliveries. In the present case, superficial retinal haemorrhage were present in the left eye which absorbed completely in six weeks period. The late absorption could probably be due to sequential use of vacuum followed by forceps delivery.Congenital glaucoma is the most important disease to be kept in mind in a neonate with corneal oedema. Due to chronic rise of intraocular pressure in the eye, the force exerted does not act in one direction, and more random in distribution resulting in ruptures in the DM as horizontal or circumferential to the limbus. In the present case, the intraocular pressure, corneal diameter were normal. The DM ruptures were vertical. Moreover, there was clear evidence of birth trauma to the eye during forceps delivery.Various causes of neonatal cloudy cornea include sclerocornea, tears in descemet’s membrane (congenital glaucoma), ulcer in the cornea (bacterial, viral), metabolic diseases (mucopolysacharidosis, mucolipidosis), posterior corneal defect (posterior keratoconus, Peter’s anomaly), endothelial dyastrophy (congenital hereditary, posterior polymorphous) [17].
4. Conclusions
- Improved prenatal care and elective caesarean section have greatly reduced forceps deliveries. Although ocular injuries following forceps delivery are rare now-a-days, they can damage the eye and its adnexa with a subsequent visual morbidity. It is a good practice to refer all the newborns delivered by obstetric forceps to the ophthalmologist for eye examination to rule out any ocular injuries.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML