-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2018; 8(2): 368-371
doi:10.5923/j.ajmms.20180812.03

Unilateral Proptosis in a Child: A Rare Initial Manifestation of Acute Myeloid Leukaemia
Sagili Chandrasekhara Reddy1, 2
1Department of Ophthalmology, School of Medicine, University Sains Malaysia, Kubang, Kerian, Kelantan, Malaysia
2Department of Ophthalmology, Faculty of Medicine and Defence Health, National Defence, University of Malaysia, Sungai Besi Campus, Kuala Lumpur, Malaysia
Correspondence to: Sagili Chandrasekhara Reddy, Department of Ophthalmology, School of Medicine, University Sains Malaysia, Kubang, Kerian, Kelantan, Malaysia.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A 6-year-old boy presented with painless progressive protrusion of the right eye for the past two weeks. The eyeball was protruded forwards and slightly downwards, with diffuse firm mass felt in the lateral aspect of upper eyelid under the orbital margin. Vision was 6/12 in the right eye and the conjunctiva was diffusely congested. Anterior segment was normal. Fundus examination showed normal optic disc, dilated tortuous veins and retinal striations in the macular area. The full blood counts, peripheral blood smear and bone marrow aspiration revealed the diagnosis of acute myeloid leukaemia. The CT scan orbits showed soft tissue mass in the superotemporal part of right orbit extending downwards and medially, causing proptosis; optic nerve was normal. Fine needle aspiration cytology from the mass in the orbit confirmed the infiltration of myeloblasts. The child was treated with standard regimen of chemotherapy for acute myeloid leukaemia in the paediatric oncology unit. The proptosis completely resolved and vision improved to 6/6 in the right eye after four cycles of chemotherapy. The child completed the full course of chemotherapy and is doing well. Leukaemia should be included in the differential diagnosis of proptosis in children. The full blood counts and peripheral blood smear can help in early diagnosis of leukaemia in all cases of proptosis in children. Myeloid sarcoma is an extramedullary infiltration of immature granulocytic cells in the orbit which presents as proptosis. It may occur during the course of the disease or as a presenting sign of acute myeloid leukaemia.
Keywords: Acute myeloid leukaemia, Proptosis, Granulocytic sarcoma, Myeloid sarcoma
Cite this paper: Sagili Chandrasekhara Reddy, Unilateral Proptosis in a Child: A Rare Initial Manifestation of Acute Myeloid Leukaemia, American Journal of Medicine and Medical Sciences, Vol. 8 No. 2, 2018, pp. 368-371. doi: 10.5923/j.ajmms.20180812.03.
1. Introduction
- Ocular manifesatations of leukaemia usually occur during the course of the disease. Rarely they may be the initial mode of presentation or the first manifestation of relapse of the systemic illness after chemotherapy. The spectrum of ocular involvement in childhood leukaemia can be divided into three groups: (i) direct infiltration in orbit and ocular tissues (iris, choroid, retina, optic nerve) (ii) vascular abnormalities affecting the retina (intraretinal haemorrhages, white centered haemorrhages, cotton wool spots, macular haemorrhage, subhyaloid haemorrhage and vitreous haemorrhage) which reflect changes in haematological status and (iii) neuro-ophthalmic signs (papilloedema secondary to raised intracranial pressure and isolated cranial nerve palsies) of central nervous system disease [1].Acute myeloid leukaemia (AML) accounts for nealy 15% of all leukaemias in children; and proptosis as initial presenting sign is unusual in this diseas [2]. Localised extramedullary tumours composed of immature myeloid cells were termed as granulocytic sarcoma/ myeloid sarcoma reflecting the cellular type that form these tumours, or chloromas because of their classical greenish appearance produced by a pigmented enzyme called myeloperoxidase. This constitutes a classic but uncommon clinical feature of myeloid leukaemia. Orbital involvement occurs typically in patients who are suffering from leukaemia or as initial presenting sign who show evidence of acute leukaemia during work up for the diagnosis [3].Shields et al [4] published a case of bilateral orbital myeloid sarcoma as initial sign of acute myeloid leukaemia and reviewed the laterality among orbital myeloid sarcoma in children and young adults. They estimated unilateral proptosis in 40% (36/89) and bilateral proptosis in 60% (53/89) patients of myeloid leukaemia. Murthy et al [5] reported extramedullary leukaemia in 12 children (aged 1- 17 years, mean age 8.8 years) who presented with proptosis (leukaemic cell infiltration in the orbit) as initial presenting sign (2-20 weeks duration), four in the right eye, four in the left eye and four in the both eyes. Fundus was normal in 7 children and pale centred retinal haemorrhages, disc oedema and preretinal/ subhyaloid haemorrhage were seen in other 5 children. There is no case report of unilateral proptosis presenting as initial manifestation of AML published in the literature from Malaysia and thus, this is the first case report from this country. Therefore, the present case is reported in view of its rarity.
2. Case Report
- A 6 year-old boy was referred from a district hospital to the eye clinic of our university teaching hospital with history of painless protrusion of the right eye for the past two weeks. He sustained injury to the right eye one week back with the handle of bicycle when he fell down while riding it. Child developed red eye and watering which subsided with the antibiotic eye drops given by a local general practitioner. Mother told that the child could not close the right eye completely as that of left eye for the past few days. There was no history of fever or weight loss or tiredness; and the child was active in his daily activities.Examination of the right eye showed marked protrusion of the globe forwards and slightly downwards. A diffuse, firm mass was felt in the right upper eyelid under the orbital margin below the eyebrow and above the lateral canthus (Fig. 1 and 2). The mass was non-pulsatile and non-tender. Preauricular and submandibular glands were palpable on the right side and were non-tender. Vision was 6/12. The conjunctiva was diffusely congested; and the of the anterior segment was normal. Ocular movements were slightly limited in all directions. The intraocular pressure with Tonopen was 16 mm Hg. Dilated pupil examination showed normal optic disc, dilated and tortuous veins, and retinal striations in the macular area. Left eye: Vision was 6/6, anterior segment, ocular movements, intraocular pressure and fundus were normal.
 | Figure 1. Right eye showing swelling below the eyebrow in the upper eyelid, marked protrusion of the globe forwards and slightly downwards, and diffuse conjunctival congestion |
 | Figure 2. Right eye showing marked proptosis and the extent of the swelling in the upper eyelid below the eyebrow and above the lateral canthus |
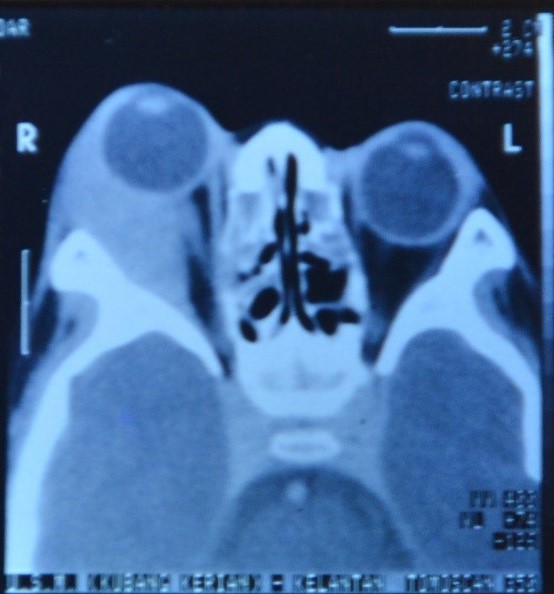 | Figure 3. CT scan axial view of both orbits showing the soft tissue mass in the superotemporal part of the right orbit extending downwards and inwards, causing proptosis |
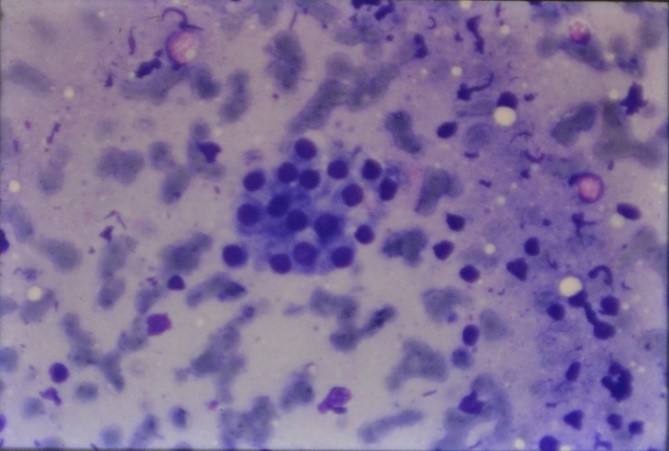 | Figure 4. Fine needle aspiration cytology from the mass in the right orbit showing clusters of epithelial cells with myeloblast cells (H & E, X 100) |
3. Discussion
- Orbital infiltration in leukaemia presents with proptosis, lid oedema and chemosis. This may appear before, after or concurrently with haematological manifestations of myeloid leukaemia. Biopsy may be necessary, especially when the underlying systemic disease presents first in the orbit and is otherwise unsuspected [2]. World Health organization has classified granulocytic sarcoma/ myeloid sarcoma into three main types, depending on degree of maturation; (i) Basic – which is composed mainly of myeloblasts, (ii) Immature – which is composed of myeloblasts and promelocytes, and (iii) Differentiated – which is composed of myelocytes and more matured myeloid cells [6]. Granulocytic sarcoma is thought to originate in the bone marrow and the cells are believed to spread via the Haversian canals to collect in the subperiosteum and form a soft tissue mass. These tumours commonly affect the skull, orbit, paransal sinuses, ribs, sacrum and sternum; involvement being related to the acive haematopoisis at these sites [2]. Unilateral proptosis presenting as initial manifestation of acute myeloid leukaemia has been reported in few cases only in the recent years [7-13] from different countries in the world. Proptosis in leukaemia cases is mainly caused by leukaemic infiltrates in the orbital tissues, retrobulbar haemorrhage, orbital muscle infiltration or venous blockage. Proptosis is the most common presenting feature of granulocytic sarcoma [3, 6]; other presentations include ptosis, lacrimal gland involvement, conjunctival masses, iridic and diffuse uveal involvement [14]. Early diagnosis of this uncommon condition is essential as timely chemotherapy helps in preservation of vision and improves survival in these children. The important investigations in all cases with proptosis include full blood counts, peripheral blood film, radiological imaging of orbits (CT/MRI) for evaluation of size and location of tumour and bone marrow aspiration to diagnose leukaemia. Fine needle aspiration cytology/ tissue biopsy for the presence of leukaemic cells in the mass will confirm the diagnosis [15]. The standard chemotherapy protocol of acute myeloid leukaemia should be started in every child under the care of the paediatric oncologist. In patients with residual orbital disease after chemotherapy, low dose of radiation (24-30 Gy in conventional fractionation) can be given to improve local disease and improve the quality of life [16].Sachachat et al [17], in a prospective study of 120 newly diagnosed cases of leukaemia, reported that 3% had primary ocular involvement, 39% showed secondary manifestations, and 5% had visual loss. The ophthalmic findings may precede the findings of leukaemia or occur concurrently with the systemic disease during the blast crisiss, or present as the first sign of relapse, with or without bone marrow involvement. Granulocytic sarcoma is a diagnostic challenge in patients presenting without prior history of leukaemia and illustrates the importance of detailed ophthalmic evaluation.In the present case, all the possible causes of unilateral proptosis in children were excluded by the investigations mentioned already and acute myeloid leukaemia with orbital infiltration was found to be responsible for the presenting symptom. The diagnosis of granulocytic/ myeloid sarcoma was confirmed by fine needle aspiration cytology [7, 14]. The proptosis resolved completely and vision improved to normal following chemotherapy.
4. Conclusions
- Granulocytic/ myeloid sarcoma is a rare manifestation of acute myeloid leukaemia, but this should be included in the differential diagnosis of proptosis in children. The full blood counts, peripheral blood smear and bone marrow aspiration should be performed in all children with proptosis to diagnose leukaemia. Fine needle aspiration cytology/ tissue biopsy from the mass in the orbit will confirm the infiltration of leukaemia. Since leukaemia is a neoplasm of high malignancy, progress of the disease is rapid unless aggressive chemotherapy is given for survival of the child and preservation of vision. In patients with residual orbital disease after chemotherapy, an additional low dosage radiation can be given to control the orbital disease.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML